Medical Imaging
Overview[edit | edit source]
Medical imaging is often perceived to designate the set of techniques that noninvasively produce images of the internal aspect of the body. It is the techniques and processes used to create images of the human body for clinical purposes such as seeking to reveal, diagnose or examine injury, dysfunction or pathology.As a discipline and in its widest sense incorporates radiology, tomography, endoscopy, thermography, medical photography and microscopy (e.g. for human pathological investigations).
In the clinical context, medical imaging is generally equated to radiology and the medical practitioner responsible for interpreting (and sometimes acquiring) the images is a radiologist. The radiographer or radiologic technologist is usually responsible for acquiring medical images of diagnostic quality, although some radiological interventions are performed by radiologists.
Imaging is a useful resource for musculoskeletal conditions and is an invaluable tool for physical therapists when used appropriately. Imaging such as MRI, X-ray, CT scans, and bone scans are prime examples of practical diagnostic imaging that facilitates accurate diagnosis, prognosis, intervention, and assessment of injuries and dysfunctions that physical therapists' address on a daily basis. It is important to know when imaging is appropriate, as unnecessary imaging will squander financial resources and increase potential for premature surgery. In many cases, studies indicate diagnostic imaging is under-utilised such as x-rays identifying fractures or bone scans identifying osteoporosis[1]. There are also studies indicating over utilisation of imaging, such as x-rays or MRI’s for acute and uncomplicated low back pain.[2][3][4]
Radiographic Imaging[edit | edit source]
Radiography is the use of ionizing electromagnetic radiation such as X-rays to view objects. This imaging modality utilizes a wide beam of x rays for image acquisition and is the first imaging technique available in modern medicine. Various forms of radiographic images are in use in medical imaging.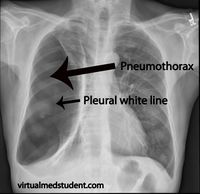
X rays (Projectional Radiography) The term x-ray refers to the radiation beam and x-ray particles, not to the film plate itself. X-ray films should be referred to as films, plain films, radiographs, or a plain film study when dialoging within the medical community.[6]
X rays are often used to determine the type and extent of a fracture as well as for detecting pathological changes in the lungs. With the use of radio-opaque contrast media, such as barium, they can also be used to visualize the structure of the stomach and intestines.
Radiography uses X-rays to view non-uniformly composed material. In the medical field, radiography is used to diagnose or treat patients through the recording of images of the internal structure of the body. These images assess the presence or absence of disease, foreign objects, and structural damage or anomaly.
Potential areas for film and/or processing errors:
- Heel effect – a source of visual error related to x-ray production, due to the fact that x-rays released by the machine are not uniform. There are two ends to an x-ray machine, a cathode end and anode end. The cathode end releases more photons than the anode end, which results in over-exposure of the film at the cathode end and under-exposure at the anode end. Due to this fact, technicians will position the patient on the table in a manner such that the thickest portion of the body region being studied is placed nearest the cathode end of the tube and the thinner end is placed near the anode end.
- Artefact – An error in the perception of the visual image of the radiograph, usually seen as an abnormal finding or foreign body. Artifacts occur when the cassettes that house the x-ray film plates get exposed to finger prints or small debris.
- Exposure – A measure of the amount of ionising radiation determined by 3 factors: time, x-ray energy, and the quantity of the x-ray photons. Exposure can be manipulated by the technician to highlight structures of interest. Over-penetration will tend to enhance bone visibility, while under-penetration will enhance soft tissue visibility.
- Movement – A blurring in the image as a result of movement by the patient the moment the x-ray exposure is made.
- Film processing – An error that occurs during the processing of the film can result in disturbances in the contrast, detail, or density of the image displayed.
Radiodensity is a representation of the relative tissue density, based on the appearance of the tone of the tissue (white, gray, or black). The following structures may be found on a medical radiograph (in order of increasing radiodensity):[6]
- Air – black appearance, often seen in structures such as the lungs, bowels, trachea
- Fat – dark grey appearance, often seen in structures such as thicker adipose tissue
- Muscle, tendon, organ tissue – appears “neutral” or mid-grey
- Bone – cancellous bone appears as light grey, while cortical bone appears as white
- Contrast media - white appearance
- Metal – white appearance, often seen in structures such as jewellery, dental fillings, or orthopaedic hardware
Caution to the radiograph viewer/interpreter – There is an inherent error that occurs when a 2-dimensional image is created to depict 3-dimensional structures that are often superimposed on one-another. Due to this fact, radiographic studies of specific body regions often include 3 or more views from different angles.
Four principle sources of radiographic error:[6]
- Enlargement occurs because the x-ray beams exit the machine in an expanding conical pattern (similar to a flashlight beam). As a result, objects placed closer to the beam source appear larger than objects placed further away from the beam source.
- Elongation is produced by the increased beam angle at the periphery of the x-ray beam cone. As a result of the increased beam angle, objects in the periphery of the x-ray beam appear smeared or spread compared to objects in the centre of the beam.
- Foreshortening is the opposite effect of elongation. This occurs when the body region to be studied is placed at an angle to the primary x-ray beam, resulting in the appearance of decreased length.
- Superimposition occurs because anatomic structures are often stacked on one another, forcing the x-ray beam to penetrate multiple structures before arriving at the film plate. Superimposition can create the appearance of increased density of structures, or the appearance of novel structures altogether.
Other uses of Xrays for Imaging[edit | edit source]
Fluoroscopy: produces real-time images of internal structures of the body in a similar fashion to radiography, but employs a constant input of x-rays, at a lower dose rate to provide moving projection radiographs of lower quality. Contrast media, such as barium, iodine, and air are used to visualize internal organs as they work. Fluoroscopy is mainly performed to view movement (of tissue or a contrast agent), or to guide a medical intervention, such as angioplasty, pacemaker insertion, or joint repair/replacement. Fluoroscopy is also used in image-guided procedures when constant feedback during a procedure is required such as intra-operative and catheter guidance.
Fluoroscopy can be used to examine the digestive system using a substance which is opaque to X-rays, (usually barium sulfate or gastrografin), which is introduced into the digestive system either by swallowing or as an enema. This is normally as part of a double contrast technique, using positive and negative contrast. Barium sulfate coats the walls of the digestive tract (positive contrast), which allows the shape of the digestive tract to be outlined as white or clear on an X-ray. Air may then be introduced (negative contrast), which looks black on the film.
Angiography is the use of fluoroscopy to view the cardiovascular system. An iodine-based contrast is injected into the bloodstream and watched as it travels around. Since liquid blood and the vessels are not very dense, a contrast with high density (like the large iodine atoms) is used to view the vessels under X-ray. Angiography is used to find aneurysms, leaks, blockages (thromboses), new vessel growth, and placeent of catheters and stents. Balloon angioplasty is often done with angiography.
Dual energy X-ray absorptiometry (or DEXA, or bone densitometry) is used primarily for osteoporosis tests. It is not projection radiography, as the X-rays are emitted in 2 narrow beams that are scanned across the patient, 90 degrees from each other. Usually the hip (head of the femur), lower back (lumbar spine) or heel (calcaneum) are imaged, and the bone density (amount of calcium) is determined and given a number (a T-score). It is not used for bone imaging, as the image quality is not good enough to make an accurate diagnostic image for fractures, inflammation etc. It can also be used to measure total body fat, though this isn't common. The radiation dose received from DEXA scans is very low, much lower than projection radiography examinations.
Computed Tomography (CT) or CT scan (previously known as CAT scan, the "A" standing for "axial") uses a high amount of ionizing radiation (in the form of X-rays) in conjunction with a computer to create images of both soft and hard tissues. It is a helical tomography which traditionally produces a 2D image of the structures in a thin section of the body. These images look as though the patient was sliced like bread (thus, "tomography"-- "tomo" means "slice"). It has a greater ionizing radiation dose burden than projection radiography; repeated scans must be limited to avoid health effects. Contrast agents are often used, depending on the tissues needing to be seen.
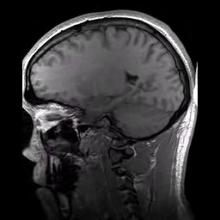
Magnetic resonance imaging (MRI)[edit | edit source]
see Magnetic resonance imaging
Ultrasound Imaging[edit | edit source]
Ultrasound uses high frequency broadband sound waves in the megahertz range that are reflected by tissue to varying degrees to produce (up to 3D) images. This is commonly associated with imaging the fetus in pregnant women. Uses of ultrasound are much broader, however. Other important uses include imaging the abdominal organs, heart, breast, muscles, tendons, arteries and veins. See also Ultrasound Scans
While it may provide less anatomical detail than techniques such as CT or MRI, it has several advantages which make it ideal in numerous situations, in particular that it studies the function of moving structures in real-time, emits no ionizing radiation, and contains speckle that can be used in elastography. It is very safe to use and does not appear to cause any adverse effects, although information on this is not well documented. It is also relatively inexpensive and quick to perform. Ultrasound scanners can be taken to critically ill patients in intensive care units, avoiding the danger caused while moving the patient to the radiology department. The real time moving image obtained can be used to guide drainage and biopsy procedures. Doppler capabilities on modern scanners allow the blood flow in arteries and veins to be assessed.
Bone Scan[edit | edit source]
Bone scan is an imaging technique that uses a radioactive compound to identify areas of healing within the bone. Bone scans work by drawing blood from the patient and tagging it with a bone seeking radiopharmaceutical. This radioactive compound emits gamma radiation. The blood is then returned to the patient intravenously. As the body begins its metabolic activity at the site of the injury, the blood tagged by the radioactive compound is absorbed at the bone and the gamma radiation at the site of the injury can be detected with an external gamma camera. A bone scan can be beneficial in determining injury to the bone within the first 24-48 hours of injury or when the displacement is too small to be detected by an x-ray or CT scan.[7]
Indications for Bone Scans:
- Primary and metastatic bone neoplasms.
- Disease progression or response to therapy.
- Paget’s disease of bone.
- Stress and/or occult fractures.
- Trauma – accidental and non-accidental.
- Osteomyelitis.
- Musculoskeletal inflammation or infection.
- Bone viability (grafts, infarcts, osteonecrosis).
- Metabolic bone disease.
- Arthritides.
- Prosthetic joint loosening and infection.
- Pain of suspected musculoskeletal etiology.
- Myositis ossificans.
- Complex regional pain syndrome (CRPS 1). Reflex sympathetic dystrophy.
- Abnormal radiographic or laboratory findings.
- Distribution of osteoblastic activity prior to administration of therapeutic radio-pharmaceuticals for treating bone pain.[8]
Electron microscopy[edit | edit source]
The electron microscope is a microscope that can magnify very small details with high resolving power due to the use of electrons as the source of illumination, magnifying at levels up to 2,000,000 times.
Electron microscopy is employed in anatomic pathology to identify organelles within the cells. Its usefulness has been greatly reduced by immunhistochemistry but it is still irreplaceable for the diagnosis of kidney disease, identification of immotile cilia syndrome and many other tasks.
Nuclear Bombs[edit | edit source]
Nuclear medicine on a whole encompasses both the diagnosis and treatment of disease using nuclear properties. In imaging, the energetic photons emitted from radioactive nuclei are used for enhancing and viewing various pathologies.
Gamma cameras are used in nuclear medicine to detect regions of biological activity that are often associated with diseases. A short lived isotope, such as 123I is administered to the patient. These isotopes are more readily absorbed by biologically active regions of the body, such as tumors or fracture points in bones.
Positron emission tomography (PET) is primarily used to detect diseases of the brain and heart. Similarly to nuclear medicine, a short-lived isotope, such as 18F, is incorporated into a substance used by the body such as glucose which is absorbed by the tumor of interest. PET scans are often viewed alongside computed tomography scans, which can be performed on the same equipment without moving the patient. This allows the tumors detected by the PET scan to be viewed next to the rest of the patient's anatomy detected by the CT scan. Another 3D tomographic technique is SPECT but uses gamma camera like method for reconstruction.
Diagnostic Imaging for Body Regions[edit | edit source]
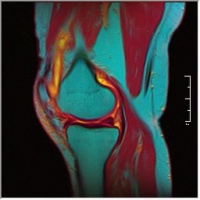
- Diagnostic Imaging of the Hip for the Physical Therapist
- Diagnostic Imaging of the Knee for the Physical Therapist
- Diagnostic Imaging of the Ankle and Foot for the Physical Therapist
- Diagnostic Imaging of the Shoulder
References[edit | edit source]
- ↑ Van Tulder MW, Tuut M, Pennick V, Bombardier C, Assendelft WJJ. Quality of primary care guidelines for acute low back pain. Spine. 2004;29(17):E357-62. Available at: http://www.ncbi.nlm.nih.gov/pubmed/15534397.
- ↑ Freeborn DK, Shye D, Muttooty JP, Eraker S, Romeo J. Primary Care Physicians ’ Use of Lumbar Spine. Journal of General Internal Medicine.3-9.
- ↑ Carey TS, Garrett J, Back C, Project P. Patterns of Ordering Diagnostic Tests for Patients with Acute Low Back Pain. Medicine. 1996.
- ↑ Anon. Isaacs_MRI_2004.
- ↑ The Audiopedia What is MEDICAL IMAGING? What does MEDICAL IMAGING mean? MEDICAL IMAGING meaning & explanation Available from: https://www.youtube.com/watch?v=Dm9iaq8uMkI (last accessed 1.10.19)
- ↑ 6.0 6.1 6.2 Biederman, R. E., Wilmarth, M. A., & Editor, C. M. D. T. (n.d.). Diagnostic Imaging in Physical Therapy Avoiding the Pitfalls. Diagnostic Imaging.
- ↑ Swain J, Bush K. Diagnostic Imaging for Physical Therapists. St. Louis: Saunders Elsevier; 2009
- ↑ College A. ACR PRACTICE GUIDELINE FOR THE PERFORMANCE OF ADULT AND PEDIATRIC SKELETAL SCINTIGRAPHY ( BONE SCAN ). North. 2007:1-5.