Manual Lymphatic Drainage
Description[edit | edit source]
Manual Lymph drainage (MLD), is a technique developed by the Vodders (Dr. Emil Vodder and his wife, Estrid) in 1936 in Paris for treatment of swollen lymph nodes[1].
Lymphatic diseases, especially lymphedema, represent a serious problem in the health community[2].
MLD is a light, skin-stretching massage that helps promote the movement of lymphatic fluid out of the swollen limb. It should not be confused with a traditional massage. MLD is specifically focused on the lymph vessels to help the flow of lymphatic fluid. Therapy is applied to your unaffected areas first, making it possible for the fluid to move out of the affected area, or “decongest” the region. MLD helps open the remaining functioning lymph collectors and move protein and fluid into them, as well as to help speed up lymph fluid flow through the lymphatics.
Deep breathing techniques call diaphragmatic breathing are usually done at the beginning and end of a therapy session to help open the deep lymphatic pathways. It’s not only relaxing, but it helps increase movement of fluid toward the heart[3].
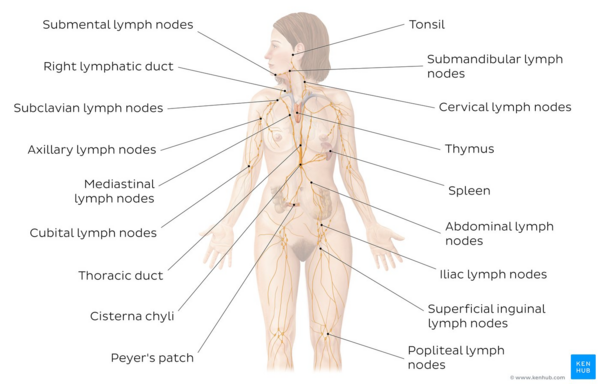
Image: Overview of the lymphatic system[4]
MLD:
- is intended to stimulate lymph nodes and increase rhythmic contractions of the lymphatics to enhance their activity so that stagnant lymphatic fluid can be rerouted.
- MLD is composed of four main strokes: stationary circles, scoop technique, pump technique, and rotary technique.
- Is effective both as a preventative treatment and as a postoperative rehabilitation treatment, and has optimal results when it is combined with the other elements of CDT (Complete Decongestive Therapy).[2]
- MLD also increases blood flow in deep and superficial veins.[5]
- Other than lymphedema, MLD may be useful in conditions such as post-traumatic and post-surgical edema, and palliative care.
Techniques[edit | edit source]
There are various techniques for MLD including the Vodder, Földi, Leduc or Casley-Smith methods.
Often, MLD is recommended as a component of the treatment plan known as Complete Decongestive Therapy (CDT), although it may be used in combination with other treatments. Research studies haven’t clearly proven the effectiveness of MLD, but they have shown that CDT is effective — and CDT usually includes MLD[2].
It often takes many hours of training in MLD, combined with years of hands-on experience, for a lymphedema therapist to become truly skilled.
The most appropriate techniques, optimal frequency and indications for MLD, as well as the benefits of treatment, all remain to be clarified, but the different methods have several aspects in common [6]
- Usually performed with the patient in the lying position
- Starts and ends with deep diaphragmatic breathing
- The unaffected lymph nodes and region of the body are treated first
- Moves proximal to distal to drain the affected areas
- Slow and rhythmical movements
- Uses gentle pressure
The video below gives a very brief explanation of Manual Lymphatic Drainage
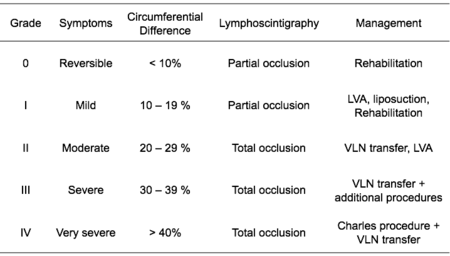
There are four primary stages of lymphedema that each impact the body in different ways, and can be categorized according to severity.
- The way duration of treatments varies depending on the stage of lymphoedema the client has eg intensive treatment may be for 2-4 weeks and less intensive treatments could last for months or for years .[2]
Different Approaches
- Vodder - Different kinds of hand motions are used on the body depending on the part being treated. It also includes treatment of fibrosis
- Foldi - Based on the Vodder technique, this method lays emphasis on thrust and relaxation. It helps in management of edema through 'encircling strokes'.
- Casley-Smith - This method involves use of small and gentle effleurage movements with the side of the hand.
- Leduc - It involves use of special 'call up' (or enticing) and 'reabsorption' movements which reflect how lymph is absorbed first in the initial lymphatics and then into larger lymphatics.[7]
Indications[edit | edit source]
- Primary or secondary lymphedema
- Lipedema
- Phlebo-lymphostatic edema
- Postoperative edema
- Posttraumatic edema [8]
- Chronic venous insufficiency [5]
- Palliative care: Provision of comfort and pain relief when other physical therapies are no longer appropriate [6]
- This technique may be used as a complement in therapies for patients with stress. [9]
- May be effective for reducing intracranial pressure in severe cerebral diseases.[10]
General Contraindications[edit | edit source]
Absolute Contraindication:
- Decompensated cardiac insufficiency
- Untreated Congestive heart failure (CHF - cardiac edema)
- Acute inflammation caused by pathogenic germs (bacteria, fungi, viruses). The germs could be spread by the manual lymph drainage, with resulting blood poisoning (sepsis).
- Acute renal failure
- Acute deep venous thrombosis (DVT)
Condition stated above must not be treated with manual lymph drainage.
Relative Contraindication:
- Malignant lymphedema caused by active cancer[11]
- Renal dysfunction
Principles[edit | edit source]
- The skin is stretched in specific directions using hand movements to promote variations in interstitial pressure without the use of oils.
- Slow repetitive movements are used which incorporate a resting phase allowing skin to return to its normal position.
- The pressure is varied according to the underlying tissue with the aim to promote lymphatic drainage.
- Areas of fibrosis are treated using deeper and firmer movements in combination with Compression therapy.
- The lymphatic drainage starts centrally and proximally with treatments usually starting around the neck.
- Functional and healthy lymph nodes are treated first, followed by proximal and contralateral areas and then ipsilateral and lymphoedematus areas.
- There is emphasis on treatment of anterior and posterior trunk in the early phases before the swollen limb is treated.
- Breathing techniques used are combined with pressure by the therapist's hands which promotes drainage of deep abdominal lymph nodes.
- Limb mobilization and relaxation techniques are often combined with lymphatic drainage.[7]
Physiotherapy[edit | edit source]
MLD is often given as part of Complete Decongestive Therapy (CDT).
- CDT is the most effective treatment for lymphedema, as it reduces the symptoms of lymphedema and improves patients’ functionality, mobility, and quality of life.
- CDT is a combination of four methods (manual lymphatic drainage, lymphedema rehabilitation exercises, compression therapy, skin care). It can achieve a 45-70% reduction in lymphedema volume.
Components of CDT include
- MLD
- Skin care
- Self-massage following instructions from their therapists
- Special light exercises designed to encourage the flow of lymphatic fluid out of the affected limb.
- Wear compression garments such as long sleeves or stockings designed to compress the arm or leg and encourage lymphatic flow out of the limb[12].
Resources[edit | edit source]
- Browse videos on this page regarding techniques on Lymphedema management.
- Manual Lymphatic Drainage (MLD) History
References[edit | edit source]
- ↑ Dr Vodder School International. Manual Lymph Drainage History (MLD). Available from: https://vodderschool.com/manual_lymph_drainage_history (Accessed 3 September 2020)
- ↑ 2.0 2.1 2.2 2.3 Tzani I, Tsichlaki M, Zerva E, Papathanasiou G, Dimakakos E. Physiotherapeutic rehabilitation of lymphedema: State-of-the-art. Lymphology. 2018 Jul 2;51(1):1-2. Available from:https://www.researchgate.net/publication/326301004_Physiotherapeutic_rehabilitation_of_lymphedema_State-of-the-art (last accessed 16.8.2020)
- ↑ Lymph care MLD Available from:https://www.lymphcareusa.com/patient/therapy-solutions/complete-decongestive-therapy/manual-lymphatic-drainage-mld.html (last accessed 17.8.2020)
- ↑ Overview of the lymphatic system image - © Kenhub https://www.kenhub.com/en/study/lymphatic-system
- ↑ 5.0 5.1 Crisóstomo RS, Candeias MS, Armada-da-Silva PA. Venous flow during manual lymphatic drainage applied to different regions of the lower extremity in people with and without chronic venous insufficiency: a cross-sectional study.Physiotherapy. 2016 Feb 1. pii: S0031-9406(16)00023-7.
- ↑ 6.0 6.1 Lymphoedema Framework. Best Practice for the Management of Lymphoedema. International consensus. London: MEP Ltd, 2006.
- ↑ 7.0 7.1 Williams AF. Manual lymphatic drainage: Exploring the history and evidence base. British Journal of Community Nursing. 2010;15(4):S18-24. DOI: 10.12968/bjcn.2010.15.Sup3.47365
- ↑ Michael Földi, Roman Strößenreuther. (2003). Basic Principles of Manual Lymph Drainage. In R. S. Michael Földi, FOUNDATIONS OF MANUAL LYMPH DRAINAGE, 3rd ed (pp. 48-49). St. Louis Missouri: Elsevier Mosby.
- ↑ Jung-Myo S, Sung-Joong K. Manual Lymph Drainage Attenuates Frontal EEG Asymmetry in Subjects with Psychological Stress: A Preliminary Study. J Phys Ther Sci. 2014 Apr; 26(4): 529–531.
- ↑ Roth C, Stitz H, Roth C, Ferbert A, Deinsberger W, Pahl R et. al. Craniocervical manual lymphatic drainage and its impact on intracranial pressure - a pilot study. Eur J Neurol. 2016 Sep;23(9):1441-6.
- ↑ Moffatt C, Doherty D, Morgan P. Lymphoedema framework. Best Practice for Management of Lymphoedema. International Consensus. London: MEP Limited;2006.58
- ↑ WEIL MLD Available from:https://www.drweil.com/health-wellness/balanced-living/wellness-therapies/lymphatic-massage-therapy/ (last accessed 28.7.2020)