Managing Disorders of the Equine Hind Limb
Introduction[edit | edit source]
To be able to accurately assess, diagnose and manage an equine patient, a good understanding of the equine anatomy is essential.
Anatomy[edit | edit source]
| Muscle | Origin | Insertion | Action | Nerve |
| Pectineus | Pubis | Femur | Adduct the limb & flex the hip | Obturator |
| Psoas Major | Ventral surface of lumbar vertebrae | Lesser trochanter of femur | Flex hip & externally rotate thigh | Ventral branches of thoracic & lumbar nerves & femoral nerves |
| Iliacus | Ventral surface of wing of the ilium | |||
| Gracilis | Pubic symphysis | Med tibia | Adduct limb | Obturator |
| Adductor | Pubic symphysis | Caudal surface of femur | Adduct limb | Obturator |
| Internal Obturator | Pelvic Floor | Trochanteric fossa of femur | Lateral rotation of femur | Ischiatic |
| Gemelli | Ischium | Trochanteric fossa of femur | Lateral rotation of femur | Ischiatic |
| External Obturator | Ventral surface of pubis and ischium | Trochanteric fossa of femur | Adduct thigh | Ischiatic |
| Quadratus femoris | Ischium | Caudal surface of femur | Extend hip & adduct thigh | Obturator |
| Deep gluteal | Body of ilium | On or near greater trochanter | Extension
Abduction |
Gluteal |
| Superficial Gluteal | Dorsal to hip joint | Third Trochanter | Abduct hip | Gluteal |
| Tensor fascia latae | Tuber coxae | Lateral femoral fascia | Hip flexion & stifle extension via tension of lat femoral fascia | Gluteal |
| Biceps femoris | Ischiatic tuberosity (Tuber Ischii) | Greater Trochanter | Extend hip
Abduct hip |
Gluteal |
| Semitendinosus | Ischiatic tuberosity | Tibia and calcaneal tub. | Extend hip
Flex stifle Extend tarsus |
Ischiatic |
| Semimembranosus | Ischiatic tuberosity | Femur and tibia | Extend hip
Flex or extend stifle |
Ischiatic |
| Middle Gluteal | Wing of ilium | Greater trochanter of femur | Extension and abduction | Gluteal |
| Rectus femoris | Ilium (cranioventral iliac spine) | Patella and patella tuberosity | Flexion of hip
Extension of stifle |
Femoral |
| Vastus lateralis | Proximal femur | Extends the stifle | ||
| Vastus medialis | ||||
| Vastus intermedius |
Table of muscles of the Hip and Stifle
| Muscle | Origin | Insertion | Action | Nerve |
| Gastrocnemius | Distocaudal surface of the femur | Calcaneal tuberosity | Extend tarsus
Flex stifle |
Tibial |
| Long digital extensor | Extensor fossa of femur | Extensor processes of digital phalanges | Flex hip
Extend stifle |
Peroneal |
| Soleus | Head of fibula | Tendon and lateral head of gastrocnemius | Extend tarsus | Tibial |
| Lateral digital extensor | Fibula | Lateral aspect of digit | Extend digits
Flex tarsus |
Peroneal |
| Deep digital flexor | Tibia and fibula | Distal Phalanx | Extend tarsus
Flex digits |
Tibial |
| Superficial digital flexor | Caudal distal femur, deep to gastrocnemius | Calcaneal tuberosity
Middle phalanx |
Flex stifle
Extend tarsus Flex digits |
Tibial |
Table of muscles of the Stifle, hock and pes
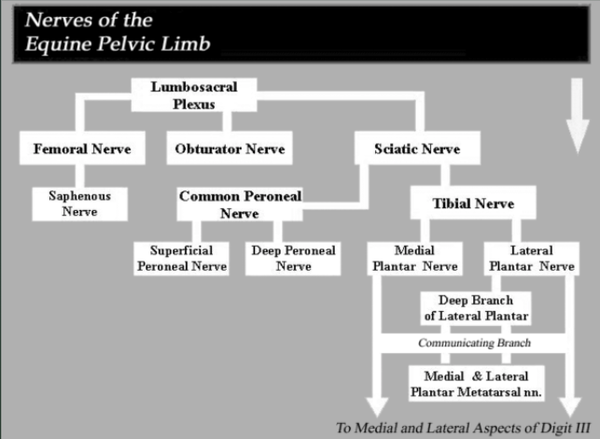
Nerves to the Pelvic Limb[edit | edit source]
- Femoral nerve (L4, L5 sometimes L3, L6)
- Muscle Innervation – Stifle extensors (quadriceps), Iliopsoas
- Cutaneous Innervation – Med aspect of limb
- Obturator nerve (L5, L6)
- Muscle Innervation– Adductors (obturator, adductors, gracilis)
- Cutaneous Innervation– nil
- Gluteal nerve (L6, L7, S1)
- Muscle Innervation– gluteals, TFL, bicaps femoris, semitenndinosus
- Cutaneous Innervation– nil
- Sciatic nerve (L6, L7, S1, S2)
- Muscle Innervation– biceps femoris, semitendinosus, semimembranosis
- Cutaneous Innervation– see tibial and fibula branches
- Tibial nerve (S1, S2)
- Muscle Innervation– extensors of hock, flexors of digits
- Cutaneous Innervation– caudal aspects of the limb below stifle
- Fibular nerve
- Muscle Innervation– flexors of the hock, extensors of the digits
- Cutaneous Innervation– cranial and lateral aspects of limb
Pelvic Limb Stay Apparatus[edit | edit source]
Function[edit | edit source]
The pelvic limb stay apparatus is what is used by the horse to support the weight of the caudal end of its body while using a minimal amount of muscular activity. When employed by one pelvic limb, the stay apparatus allows the other pelvic limb to be placed in a "resting" position with just the tip of the hoof touching the ground. Although the stay apparatus reduces the amount of energy required to remain standing, the amount of muscular effort is not reduced. This explains why you see horses switching their weight from one hind limb to another.
How does the stay apparatus function?[edit | edit source]
The pelvic limb stay apparatus has three essential elements.
- The stifle joint locking mechanism, allows the weight of the caudal body to rest, essentially, on the locked joint.
- The reciprocal mechanism, ensures that the stifle and hock joints will move in unison, and the leg will move in a smooth, coordinated manner.
- All other ligaments/tendons in the distal limb.
Hindlimb Lameness (HL)[edit | edit source]
The hind legs serve as the horse’s prime propelling force. Most lameness in the hindlimb is due to problems of the tarsus and below the hock. Hindlimb lameness is best observed while the horse is trotted away from the examiner and if the examiner observes from the side of the lame limb.[3] Observation of
- asymmetrical movement of the pelvis on the side of the lame hindlimb is the most NB and consistent abnormality.
- The tuber coxae (+ point of hip & glute) on the lame side rise higher (weight bearing) and lower (when sound limb bears weight) than the sound limb when straight trotting on a flat surface (use tape if necessary).
- The horse’s head is lowered when the lame leg contacts the ground.
- The horse’s tail head rises when the lame hindlimb bears weight (not always visible)
- Choppy, short gait lacking impulsion and no asymmetric pelvic movement may suggest bilateral hindlimb lameness
- Stride length characteristics(‘carrying’ lame hindlimb when viewed from side), height of hoof flight, sound and fetlock drop
Manipulative tests[edit | edit source]
Examine joints for:
- Decreased ROM
- Increased instability
- Crepitus
- Pain (superficial or deep – but usually results in adverse reaction to manipulation)
- Willingness or resistance of horse to undergo procedure and lack of willingness to bear weight on lame limb when the opposite (sound) limb is manipulated
- Exacerbation of lameness thus localizing pain to the ‘stressed’ part of the limb
Tests for hindlimb lameness
- Provocative test
- Not sensitive or specific
- Excessive force may ‘create’ lameness with no clinical relevance
- Must compare results with the other side
- Used in conjunction with other tests
- Flexion tests: joint to be tested held in flexed position for 45 – 60s horse then immediately trotted out and any worsening of the gait noted. Difficult to isolate due to stay mechanism. Flexion tests involve putting joint and surrounding soft tissues under stress. Not normally carried out by physio.
- Direct pressure tests: as useful as flexion tests. Response to localized pressure over painful area. Compression maintained for 30s. Horse trotted off and observed for exacerbation of lameness.
Diagnostic analgesia (nerve blocking)[edit | edit source]
- Remains the most valuable tool to localize lameness to a specific structure of a limb.
- Nociceptive nerve blocked with a local anesthetic
- Used for:
- perineural infiltration to desensitize the structures supplied by the nerve distal to the injection
- Analgesia of joints, tendon sheaths or bursa
- Direct local infiltration over suspected superficial lesions
Unless confirming a suspected lesion, nerve blocking begins at the hoof and continues up the limb blocking out certain segments. One must wait 5-10 mins for lower parts of the limb to anesthetize and up to an hour for upper limb blocks. If lameness improved more than 70% after block, it is considered diagnostic.
- Diffusion of local analgesia can cause false positives so tests must be done within 5-10mins of administration
- If lameness persists, this could be due to chronic or deep bone pain
Diagnostic Imaging[edit | edit source]
For more details and accurate orthopedic diagnoses – used in conjunction with findings from history, physical and lameness examinations
- X-ray
- Mainstay of diagnostic imaging in horses
- Gives information on bones, joints, ligaments, tendons and joint capsule insertions
- Done following identification of site of pain
- As in humans, association between radiographic findings and pain and disfunction is not always clear cut[5]
- CT & MRI
- Available in training institutes and large animal hospitals
- Provides detailed images in any plain
- Machine size limits scans to mid-radius and tibia and upper mid-cervical, spine and head
- Nuclear scintigraphy
- Involves intravenous administration of a radioactive isotope (technetium 99) which emits gamma radiation
- This gamma radiation is taken up where there is a high rate of bone remodeling which is indicative of disease
- The increased gamma radiation emitted from a particular site is called a hot spot
- Scintigraphy has allowed early recognition of a subtle change in blood flow, soft tissue and bone lesions (OA and osteitis) and stress fractures which were previously missed
- Involves intravenous administration of a radioactive isotope (technetium 99) which emits gamma radiation
- Ultrasound
- Affordable, non-invasive diagnostic technique, Allows for repeated assessment of tissue lesion over time
- High frequency (>1mHz) emitted from transducer to image tissues of the body
- Bone is hyperechoic as is seen as a white image.
- Soft tissues / tendons are hypoechoic and are seen as a grey image.
- Fluid / blood is anechoic and is seen as a black region
- Indicated for:
- Tendons, tendon sheaths, ligaments, muscles, joint capsule and bursal defects
- Monitoring the effect of training on tendons and ligaments to prevent potential injury
- Comparison with opposite limb
- Monitoring healing of tendons and ligaments
- Assessment of fluid accumulation
- Evaluation of bony surfaces eg. Tuber-coxae, knee, hock Bone Fractures
Fracture[edit | edit source]
Complete fracture[edit | edit source]
- Due to excessive load or traumatic event
- Obvious with significant lameness regardless of size and location
- Acute, non-weight bearing lameness can be indicative of a complete fracture, but could also be bone, joint or tendon sheath injuries
- OCD of a carpal bone may only produce a low-grade lameness
Incomplete fracture (stress fracture)[edit | edit source]
- Commonly occurs at metacarpus / metatarsus, tibia, humerus and pelvis
- Seen most often in race horses
- Due to chronic micro-trauma which weakens the bone
- Difficult to diagnose
- Usually diagnosed with scintigraphy
Classification and prognosis of fractures[edit | edit source]
- Complete / incomplete (stress)
- Stable / unstable (displaced or non-displaced)
- Open / closed
- Oblique / transverse / spiral / multiple / comminuted
- Location: articular / non-articular / chip / epiphyseal / slab
- Poor prognosis – unstable / displaced / above carpus or tarsus / open / comminuted / uncooperative horses > 450kg
- Depending on prognostic factors, a fracture can take 12 months or more to heal
Undesirable consequences of fracture healing where physiotherapy could play a part[edit | edit source]
- Equine joints become stiff from degenerative ankylosis rather than disuse
- Tendons become flaccid from external immobilization
- Muscles atrophy from external immobilization
- Tendons, ligaments and muscles may be impaired by scar tissue formation
- Flexion deformities develop in young horses due to immobilisations
- If there is infection, fibrous tissue may lead to severe loss of function
- Consider the other limbs carrying excessive weight
- Physiotherapy can be of help especially in the early stages after cast removal or several weeks after internal fixation
Risk factors in fractures[edit | edit source]
- Bone infection
- Osteitis – inflammation of the periosteum
- Osteomyelitis – an infection which extends into the medullary cavity
- Treated with antibiotics
Tendons and Ligaments[edit | edit source]
Signs and symptoms[edit | edit source]
The main signs and symptoms when there has been a tendon or ligament injury is pain, oedema, heat and lameness.
- Tendons and ligaments in the equine are highly prone to injury and the SDF tendon operates close to its physiological limits when galloping at maximum speed or jumping over large fences
- Consequently, minor repetitive damage occurs to tendons and can result in tendinitis. This can sometimes be avoided by ensuring tendons and ligaments are stronger and stiffer using a graduated fitness and strengthening programme.
- Tendons can suffer from extrinsic or traumatic injury or intrinsic cumulative micro-strain of individual fibrils until tendon rupture occurs
Mechanism of injury[edit | edit source]
- Sudden excessive overextension
- Direct low-grade mechanical forces due strenuous exercise which leads to micro-damage of the fibrils due to cumulative fatigue of the tendon matrix. Damage may be exacerbated by poor foot and limb conformation, landing from a jump, lack of fitness, deep surfaces, fatigue and weak stabilizing muscles
- Tendons / ligaments appear to have little ability to adapt after skeletal maturity, so they suffer age related degeneration (this might explain the presence of pathological tendon damage in older horses without clinical signs)
- Due to poor circulation in tendons and ligaments, galloping horses have hot tendons (up to 45 degrees) which damages matrix proteins
- Variable blood flow after maximal exercise results in ischemia and reperfusion injuries
Healing of tendons and ligaments[edit | edit source]
- Hemorrhage, oedema, acute inflammation, fibroblastic proliferation, collagen production and chronic remodeling[6]
- Unchecked inflammation in early stages can cause progression of the lesion
- Tendon tissue is replaced by scar tissue which is weaker, predisposed to re-injury and results in adhesions
- It remodels over more than 6 months but it is never a normal tendon again. Controlled exercise during this phase may improve collagen fibral alignment
- Takes 15 - 18 months to heal completely but will have poor elasticity resulting in increased strain of adjacent regions and opposite limbs or other supporting ligamental structures including the suspensory apparatus.
Common Conditions[edit | edit source]
- Tendonitis
- Inflammation of tendon/Musculo-tendinous attachments caused by excessive strain
- Desmitis
- Inflammation of a ligament
- Minor tears to avulsion from bony attachment
- Forelimbs more commonly affected than hindlimbs as they carry 70% of the horse’s bodyweight
- SDF more commonly affected than DDF
- Localised to mid-metacarpal region because cross-sectional area smallest and blood supply poorest
- Diagnosis: Ultrasound scan which is also used to monitor recovery
- Highest frequency of injuries seen:
- Racehorses
- Inadequate training
- Muscle fatigue
- Poor conformation
Treatment[edit | edit source]
- Stop training and complete box rest for 4 – 6 weeks
- Controlled exercise for a minimum of 6 – 10 months
- Control inflammation
- Minimise excessive scar formation
- Ice immediately
- IRAP; stem cell therapy
- Therapeutic shoeing
- Shockwave
- High Power Laser[7][8]
- Controlled exercise and rehabilitation starting with hand walking on hard surfaces progressing to ridden exercise in straight lines on hard surfaces over 3 – 4 months, gradually introducing softer surfaces and then big to smaller circles
Note: although clinical signs are often resolved with a short period of rest, much longer is needed before optimal healing has occurred.
- Surgical therapy: one can do an accessory ligament desmotomy which increases the use of the SDF muscle to reduce load on the tendon. Unfortunately results are inconclusive.
The Tendon Sheath[edit | edit source]
Tenosynovitis[edit | edit source]
Tenosynovitis (synovial effusion of the tendon sheath) may be idiopathic, acute, chronic or septic
- Idiopathic: most commonly found in extensor tendon sheaths, over carpus, in foals
- Tarsal sheath which encloses DDF tendon over hock (thoroughpin)
- Digital flexor sheath enclosing SDF/DDF tendon above/below fetlock (windgalls)
- Risk factors include chronic low-grade trauma and poor conformation
- Acute
- Direct trauma DDF and SDF tendonitis or suspensory ligament desmitis are potential causes
- Rapidly developing effusion, most commonly seen in digital tendon sheath of the extensor tendon over the carpus
- Accompanied by distension, heat, pain and possibly lameness
- Chronic
- Persistent synovial effusion with non-inflammatory swelling and fibrous thickening of the tendon sheath
- Caused by repetitive micro-trauma
- Commonly follow acute unresolved tenosynovitis
- Accompanied by adhesions and thickening of the sheath. Reduced function with inability to flex carpus if extensor sheath affected
- Reduced function with inability to flex fetlock if digital tendon sheath affected
- Ultrasound evaluates sheath thickening, adhesions and tendon injury
- Septic
- Emergency infection introduced via a penetrating wound or contaminated needle
- Critical due to difficulty in eliminating infection which could lead to a chronic infection which can cause tendon rupture and laminitis in the opposite limb
- Digital flexor; extensor and tarsal sheaths involved
- Diagnosis confirmed by synovial fluid analysis. Ultrasound used to identify adhesions, injuries of tendons and involvement of annular ligament
- Treatment: antibiotics and lavage of sheath
- Adhesion formation may result in failure to return to previous activity
Principles of management[edit | edit source]
- Box rest
- Control inflammation
- Reduce effusion and adhesion formation
- Control infection in septic tenosynovitis
- Surgery
- Arthroscopy for chronic/septic tenosynovitis to assess sheath to drain fluid, break down adhesions, flush tendon sheath, perfuse with antibiotics or release annular ligament
Arthritis[edit | edit source]
- Single or repetitive episodes of trauma involved in pathogenesis
- One disorder may progress to the next with significant overlap
- Traumatic arthritis
- Idiopathic synovitis & capsulitis
- Sprain, sub luxations, meniscal tears and intra-articular fractures
- OA and septic arthritis
- Non-inflammatory disorder of a joint
- Characterised by loss of articular cartilage and development of new bone on joint surfaces and margins
- Develops in four ways:
- Acute – synovitis encapsulitis involving high motion joints such as the carpus and fetlock
- Insidious – high load, low motion joints (ring bone is interphalangeal OA), intertarsal (bone spavin). Main cause is repetitive trauma in young, mature and aged active horses[9]
- Non-progressive articular cartilage erosion. Associated with age and continued low-level use. Possibly with no clinical significance
- Secondary to intra articular fractures, luxations, sprains, wounds, septic arthritis and osteochondrosis
Main pathogenic mechanisms which are hypothesized
- Defective cartilage which fails under a normal load
- Microfractures of sub-chondral and epiphyseal due to excessive mechanical stresses
- Repetitive impact trauma leads to cartilage micro fractures and alteration in chondrocytes
- Damaged chondrocytes lead to flawed repair which causes the release of cytokines and leads to cartilage fissuring, separation and decreased viscoelasticity
Septic Arthritis[edit | edit source]
- The most severe joint problem in horses and the most common cause of death in foals
- Involves bacterial colonization of synovial membrane which then necroses
- Inflammatory mediators eventually lead to cartilage degradation
- Bacteria enter joints via blood from the umbilicus, respiratory or GI infections
- Local penetration by direct trauma to the joint
- Intra articular injection of cortisone or joint surgery
The tarsocrural (tibiotarsal joint of the hock) is most commonly affected, followed by fetlock, carpus and stifle
Medical Therapy[edit | edit source]
- Rest and immobilization to prevent further physical damage
- Control pain and inflammation
- Remove mediators using joint lavage
- Antibiotics
- Allow sufficient time for cartilage healing
- Re-introduce controlled exercise once infection is controlled and lameness cleared
- Surgical therapy: to treat primary causes of OA such as osteochondrosis, intra articular fractures, chips and meniscal tears using an arthroscopic technique
- Surgical arthrodesis for joint laxation and end state OA (eg. Pastern and distal tarsal joints)
- Synovectomy: to remove fibrous synovial membrane, to lower the concentration of harmful enzymes
- Arthroscopy for open drainage in septic arthritis
Locking Stifle[edit | edit source]
[West, C. M. (2012). Physical Therapy for Stifle Problems in Horses. www.thehorse.com]
- In order for horses to sleep standing up, there is a clever adaptation which locks the stifle to minimize muscular effort. When the patella fails to disengage from the bony ridge, the leg remains extended giving the characteristic stance seen in horse’s locking stifle.
- The horse’s leg gets ‘stuck’ in an extended position
- Intermittent upward fixation of the patella
- Treatment of upward fixation of the patella in horses and anterior knee pain in humans involves client education
- Signs and symptoms:
- Horse is often clumsy with a hind limb that ‘gives in’
- Sometimes one hears an audible click or pop
- Horse can be overweight
- Weak abdominal and topline muscles
- General deconditioning and muscle wasting
Treatment:[edit | edit source]
- More movement, not less
- Preferably 24 hour turn out in a large field with hills and a companion to encourage movement
- Place feed in small piles around the field to make them move more
- Stretching:[11]
- High flexion – hip in full flexion
- Protraction – bring limb under horses belly
- Retraction – stretch limb backwards past the tail
- Adduction – bring horse’s leg under belly towards midline & opposite side
- Strengthening:
- Isometric
- Lateral tail pull towards involved sign
- Pick up opposite hind limb without allowing horse to rest on you
- Isotonic
- Active walking tracking up properly
- Increased load with rider’s weight or walking through water
- Rein back in-hand with a good stride
- Walking up and down inclines
- Walking on hard to soft surfaces
- After 2 weeks, start transitions (walk to trot, trot to walk) in hand
- Turning on the forehand
- Backing up and down the hill
- Long line
- Ground polls
- After 8 weeks: progress to canter
- Isometric
References[edit | edit source]
- ↑ The Horse's Skeleton: Hind Limbs. Available from https://www.youtube.com/watch?v=Y7xbcWGWLc4
- ↑ Equine Pelvic Limb Stay and Reciprocal Apparatus. Available from https://www.youtube.com/watch?v=Iw3lkbC1pPY
- ↑ McGowan C, Goff L, Stubbs N. Animal physiotherapy. Assesment, Treatment and Rehabilitation of Animals JAV: Blackwell Publishing. 2007.
- ↑ Vet Basics ll Hindlimb Lameness Identification. Available from https://www.youtube.com/watch?v=dDUDL488zqQ
- ↑ Hinkle FD, Johnson SA, KT, Selberg, MF Barrett. A review of normal radiographical variants commonly mistaken for pathological findings in horses. Equine Veterinary Education. 2020;32(12):664-72.
- ↑ Dakin SG. A review of the healing processes in equine superficial digital flexor tendinopathy. Equine vet. Educ. 2017;29(9):516-20.
- ↑ Zielińska P, Nicpoń J, Kiełbowicz Z, Soroko M, Dudek K, Zaborski D. Effects of High Intensity Laser Therapy in the Treatment of Tendon and Ligament Injuries in Performance Horses. Animals (Basel). 2020;10(8):1327.
- ↑ Pluim M, Martens A, Vanderperren K, van Weeren R, Oosterlinck M, Dewulf J, Kichouh M. High-power laser therapy improves healing of the equine suspensory branch in a standardized lesion model. Frontiers in Veterinary Science. 2020;7:600.
- ↑ Vandeweerd JM, Coisnon C, Clegg P, Cambier C, Pierson A, Hontoir F et al. Systematic review of efficacy of nutraceuticals to alleviate clinical signs of osteoarthritis. J Vet Intern Med. 2012;26(3):448-56.
- ↑ Locking stifle before and after treatment. Available from https://www.youtube.com/watch?v=0Pbt_kk4Nes
- ↑ Haussler KK. Equine manual therapies in sport horse practice. Veterinary Clinics: Equine Practice. 2018 Aug 1;34(2):375-89.