Lung Compliance
Original Editor - Shalini Varadhan
Top Contributors - Kapil Narale, Shalini Varadhan, Lucinda hampton, Kim Jackson, Uchechukwu Chukwuemeka and Mohit Chand
Introduction[edit | edit source]
Pulmonary compliance, a measure of the lung expandability, is important in ideal respiratory system function. It refers to the ability of the lungs to stretch and expand. Lung compliance can be calculated by dividing volume by pressure.
- Factors affecting lung compliance include elasticity from the elastin in connective tissue and surface tension, which is decreased by surfactant production.
- Lung compliance participates in the lung-chest wall system by opposing the outward pull of chest wall compliance.
- The net compliance (lung-chest wall system) allows the lungs to achieve appropriate functional residual capacity, the volume remaining after passive expiration[1].
Transmural Pressures[edit | edit source]
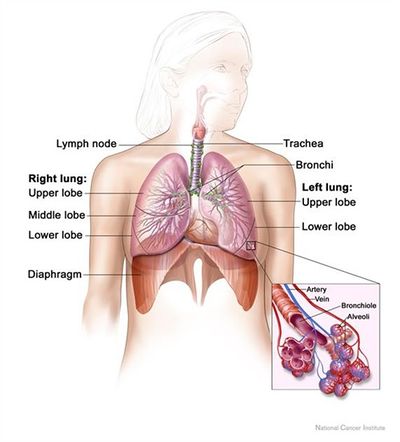
The compliance of the lung describes the relationship between the transmural pressure (ie pressure passing through a wall eg hollow structure) across the lung compared with organ's volume. By transmural pressure, we mean the relative pressure between the alveoli compared with that in the intrapleural space. Positive transmural pressures mean greater alveolar pressures than intrapleural pressures.[2]
- Although positive transmural pressures are required to expand the lung, they are not achieved by generating positive alveolar air pressures. Rather, lung expansion is achieved by generating progressively negative pressures within the intrapleural space. Conceptually, one can think of this as inflating a balloon not by breathing into it and thus increasing the internal pressure above that of atmospheric pressure, but rather by placing it within a chamber and generating a progressive vacuum around the balloon. Appreciation of this important feature of lung expansion is critical for understanding how lung expansion can be achieved given the fact that the lung is not physically attached to the chest wall and is instead separated by the intrapleural space.
- Similar to a balloon, the lungs expand by generating positive transmural pressures. However, unlike a balloon, these positive transmural pressures are generated by creating negative surrounding pressure within the intrapleural space. As shown, the pressure of air within the lungs remains equivalent to that of the atmosphere at the peak inspiration or expiration[3].
Function[edit | edit source]
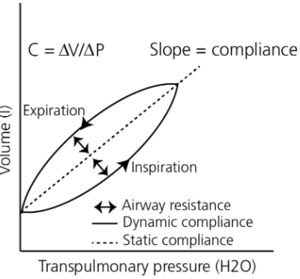
Compliance of the respiratory system describes the expandability of the lungs and chest wall. There are two types of compliance: dynamic and static.
- Dynamic compliance describes the compliance measured during breathing, which involves a combination of lung compliance and airway resistance. Defined as the change in lung volume per unit change in pressure in the presence of flow.
- Static compliance describes pulmonary compliance when there is no airflow, like an inspiratory pause. Defined as the change in lung volume per unit change in pressure in the absence of flow.
For example, If a person was to fill the lung with pressure and then not move it, the pressure would eventually decrease; this is the static compliance measurement. Dynamic compliance is measured by dividing the tidal volume, the average volume of air in one breath cycle, by the difference between the pressure of the lungs at full inspiration and full expiration. Static compliance is always a higher value than dynamic[4].
Pressure-volume curves are common schemes to express the relationship of dynamic and static compliance where the slope is compliance.[5]
Important Factors[edit | edit source]
Two important factors of lung compliance are elastic fibers and surface tension.[6] More elastic fibers in the tissue lead to ease in expandability and, therefore, compliance. Surface tension within the alveoli is decreased by the production of surfactant to prevent collapse. Compliance is more easily achieved by decreasing surface tension.
- Elastin: a highly stretchable protein that is found widely throughout the pulmonary interstitial connective tissue. Molecularly, elastin proteins naturally tend toward a globular structure but can be stretched if a force is applied; however, once the protein is fully extended the molecule is highly resistant to further stretching, similar to a rubber band. The elastic recoil of the lung and its tendency to have higher compliance at lower lung volumes is in large part explained by the combined action of the elastin fibers spread throughout the pulmonary interstitium. These fibers serve to powerfully recoil the lung and only stretch when a force is applied; however, once the lung is stretched to large volumes, these proteins become highly resistant to further stretching.
- Surface Tension: a physical property of water that causes surfaces of water to achieve the smallest possible area. Surface tension arises from the energetic preference of water molecules to interact with one another through hydrogen bonding rather than with air. Individual alveoli all contain a highly thin inner lining of water-based fluid whose surface tension exerts a collapsing force on the alveolus. This is because smaller alveolar volumes would naturally reduce the surface area of the thin fluid lining.
The combined force of surface tension throughout the lung's alveoli serves as a powerful contributor to the elastic recoil of the lung.
Increased lung volumes would require expansion of individual alveoli which is highly resisted by the surface tension of the alveolar fluid inner lining. In fact, the recoiling force of alveolar surface tension is so powerful that special surfactant chemicals must be synthesized and secreted into the inner lining fluid to reduce the surface tension. Failure to produce these surfactants is an important contributor to major pulmonary pathologies; eg Neonatal Respiratory Distress Syndrome.[3]
Pathophysiology[edit | edit source]
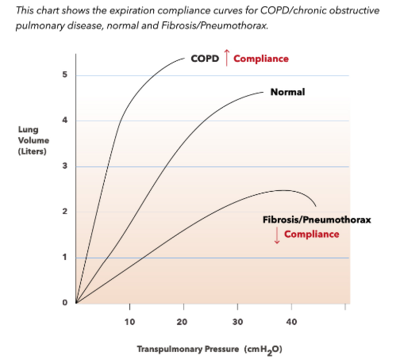
Lung compliance changes can indicate when there are issues with the lungs.
- A decreased compliance might show restrictive lung diseases. Restrictive lung disease can result from mechanical issues with peripheral hypoventilation, including poor muscular effort or structural dysfunction. Conditions like muscular dystrophy, polio, myasthenia gravis, and Guillain-barre syndrome can cause poor muscular effort. Scoliosis or morbid obesity can also cause structural limitations
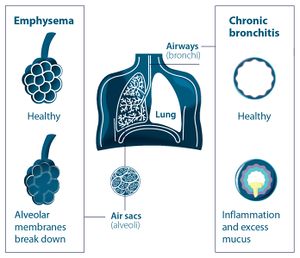
- Increased compliance can indicate a state of disease where there is degeneration of tissue that causes the lungs to have to work harder to expand, such as emphysema. With emphysema, the tissue damage means that it is easier to inhale, as there is less resistance, but it is harder to exhale[4]
- There are cases of lung compliance pathology caused by problems with the surfactant. The recoiling force of alveolar surface tension is so powerful that special surfactant chemicals must be synthesized and secreted into the inner lining fluid to reduce the surface tension. Failure to produce these surfactants is an important contributor to major pulmonary pathologies eg Neonatal Respiratory Distress Syndrome.[3].[4]
- Pneumothorax: This condition characteristically demonstrates the accumulation of air in the intrapleural space. This leads to the equalization of intrapleural pressure with atmospheric pressure. As a result, the chest wall protrudes outward, and lungs collapse as this is the natural tendency without transmural pressure. The patient will commonly present with dyspnea, chest pain, uneven expansion of the chest, and diminished breath sound on the affected side. Without proper transmural pressure, lung-chest wall compliance is inoperable.
- Obesity results in low lung compliance with reduced functional residual capacity and expiratory reserve volume.
- Scoliosis decreases the chest wall and lung compliance that results in increased respiratory workload.
- Aging is accompanied by a decrease in muscular strength and elastic recoil. Therefore, lung compliance increases and chest wall compliance decreases as age increases[1]
| Lung compliance | Chest wall compliance |
Increased lung compliance
|
Increased chest wall compliance
|
Decreased static lung compliance
Decreased dynamic lung compliance
|
Decreased chest wall compliance
|
References[edit | edit source]
- ↑ 1.0 1.1 Edwards Z, Annamaraju P. Physiology, Lung Compliance.2020 Available from:https://www.statpearls.com/articlelibrary/viewarticle/24496/ (accessed 17.4.2021)
- ↑ Iotti G, Braschi A. Measurements of respiratory mechanics during mechanical ventilation. Rhäzüns, Switzerland: Hamilton Medical Scientific Library. 1999
- ↑ 3.0 3.1 3.2 Pathway medicine Lung compliance Available from:http://pathwaymedicine.org/lung-compliance (accessed 17.4.2021)
- ↑ 4.0 4.1 4.2 Infobloom Lung compliance Available from:https://www.infobloom.com/what-is-lung-compliance.htm (accessed 17.4.2021)
- ↑ Harris RS. Pressure-volume curves of the respiratory system. Respiratory care. 2005; 50(1): 78-99.
- ↑ 6.0 6.1 LibreTexts. Factors Affecting Pulmonary Ventilation: Compliance of the Lungs. [Internet]. 2020 [cited 20 April 2021]. Available from:https://med.libretexts.org/Bookshelves/Anatomy_and_Physiology/Book%3A_Anatomy_and_Physiology_(Boundless)/21%3A_Respiratory_System/21.6%3A_Factors_Affecting_Pulmonary_Ventilation/21.6B%3A_Factors_Affecting_Pulmonary_Ventilation%3A_Compliance_of_the_Lungs