Lumbar Traction
Original Editors - Sarah Neubourg
Top Contributors - Samuel Adedigba, Admin, Kim Jackson, Liese Magnus, Rachael Lowe, Sarah Neubourg, Uchechukwu Chukwuemeka, Laura Ritchie, Lucinda hampton, Ines Musabyemariya, Jess Bell, 127.0.0.1 and Eric Robertson
Definition/Description[edit | edit source]
Various forms of lumbar traction has been used for the relief of pain since the time of Hippocrates. During the 1950’s and 1960’s it became popular, and until today it is used by physiotherapists for threatening patients with low back pain and leg pain.[1] Although its effectiveness is still being questioned by a few clinical trials (see further), there are three benefits described of lumbar traction: distraction to increase the intervertebral space, tensing of the posterior longitudinal vertebral ligament and suction to draw the disc protrusion towards the center of the joint.[2]
Different types of lumbar traction have been described:[3]
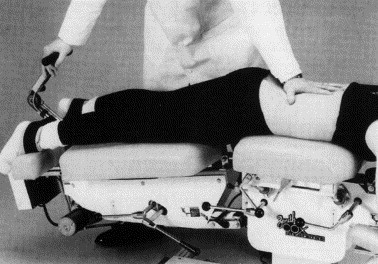
- First of all there is mechanical traction, using a mechanical device and a specially designed table that is divided into two sections.[2] The device delivers a certain tension to perform the traction. The patient wears a harness, which consists of two rings, to support the patient.[4]
- Autotraction also utilized a table divided into two sections, the patient provides the traction force by pulling with the arms and/or pushing with the feet.[2]
- Finally there is manual traction performed by the therapist, pulling at the patient his ankles. Another way of manual traction is with the patient his legs over the therapist his shoulders, the therapist will place his arms on the patient’s thighs and pull.[4]
Continuous traction is applied for several hours with the use of a small amount of weight. Sustained traction has a shorter duration but a larger tension force.[3] Intermittent traction is similar sustained traction but alternately applies and releases the traction force at certain intervals.[2]
Clinically Relevant Anatomy[edit | edit source]
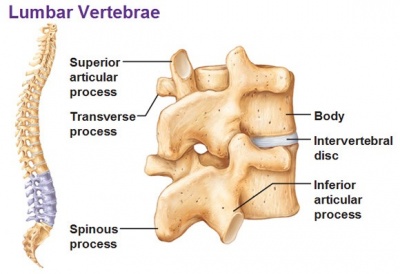
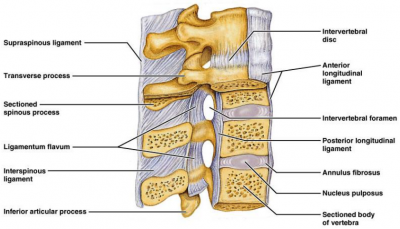
The lumbar spine amount to 5 moveable vertebrae numbered L1-L5. This complex anatomy is a considerable combination of these strong vertebrae, multiple bony component linked by joint capsules, ligaments/tendons, muscles and highly sensitive nerves. The upper body weight is distributed to the lower extremities by way of the sacrum and pelvis. This reduces the amount of work required by spinal muscles.[5] [6]
To achieve these functions:, the lumbar spine must consist of:
Resistance:
- Kyphotic and lordotic sagittal plane curves
- Increased mass of each vertebra from C1 to the sacrum
And Elasticity:
- Lordotic and kypohoic curves
- Motion segments (or functional unit): composed of two adjoining vertebrae, intervertebral disc, ligaments, two facet joints and capsules
Structure of the lumbar vertebrae:
- Ligaments:
- Anterior longitudinal ligament (ALL): from C2 to the sacrum
- Costal ligaments: connect the heads of the ribs to the vertebrae
- Intertransverse ligaments: inferior surface to the superior surface
- Posterior longitudinal ligament (PLL): from C2 caudally to the sacrum
- Interspinous
- Ligamentum flavum
- Intervertebral disks
- Facet joints
- Spinal cord/nerve roots
- Vertebral arch
- Cauda equina [5]
Epidemiology /Etiology[edit | edit source]
Low Back Pain: Low back pain (LBP) poses a significant problem to society. In the Netherlands, the 1-year-period prevalence in the general population was 44% in 2003. Almost one-fourth of the employed population with LBP reported sickness leave in 2009. LBP can also be caused by pathological conditions such as lumbar disc degeneration [7]. Low back pain is the world's number one cause of disability and one of the most prevalent health conditions. Most patients also report radicular syndromes [8] . Specific low back pain represents only 15% of all back-pain problems, and 50% of specific back pain is due to a prolapsed intervertebral disc (PID), in which the nucleus pulposus herniates through a tear in the annulus fibrosus, resulting in irritation of the adjacent nerve root and causing a typical radiculopathic pain. Generally, pain that lasts less than 4 weeks is classified as acute pain. The main clinical phenomena in acute LBP are pain and neurological disorders that affect daily activities.[9]
Lumbar disc herniation: Disc degeneration might be caused by several conditions[7]. Considerable proportion of patients with lumbar disc herniation remains symptomatic even after undergoing conservative treatments [8]
Lumbago – Sciatica: Epidemiological studies have shown that the rate of persistent sciatica is 1.6% in a given population while this rate increases to 25% with aging up to 64 years. [7]
Mechanism of Action[edit | edit source]
Several theories have been proposed to explain the possible clinical benefit of traction therapy. Distracting the motion segment is thought to change the position of the nucleus pulposus relative to the posterior annulus fibrosus [10] [2] or change the disc-nerve interface [11]. These effects are plausible based on studies examining the kinematics of the lumbar spine during traction therapies. In addition to separating the vertebrae, traction has been shown to reduce nucleus pulposus pressure [12] [13]and increase foraminal area [13]. However, it is unlikely that mechanical changes observed in a prone position will be sustained after a patient resumes an upright, weight bearing posture. Any lasting clinical response to traction therapy would more likely be because of the effect of traction on the mechanobiology of the motion segment or neural tissues. Complicating the issue further is that not all traction therapies exert the same force on the spine and animal studies have found the mechanobiology of the disc to be sensitive to the amount, frequency, and duration of loading [14]. It is possible that some forms of traction stimulate disc or joint repair[15] whereas others promote tissue degradation[16] . Although these variables have not been systematically examined, even in animal models, what is known regarding disc mechanobiology should alert us to the possibility that not all traction therapies are equal. If distracting the spine can influence disc and joint mechanobiology, different modes of traction may result in different clinical results. Systematic reviews of lumbar traction therapy have typically not considered that different effects may exist based on force and time parameters[17] . Traction trials have most often included patients with a mix of clinical presentations including back-dominant low back pain (LBP), leg-dominant LBP, or both. However, a patient with only dominant LBP and no radiculopathy is likely experiencing pain from a sclerotomal source, such as facet joints or disc, whereas sciatic pain, even if caused by disc herniation, may be predominately of neural origin. Although it is reasonable to suspect that traction therapies may affect these conditions differently, there is insufficient evidence to support this hypothesis. Distraction-manipulation and positional distraction are mechanically different than traditional traction (intermittent or sustained). Rather than allowing forces to be dispersed throughout the lumbar tissues, these treatments attempt to concentrate them in a smaller area. AT, for example, allows the patient to concentrate the force by finding the position that most relieves their pain and applying distraction in that position. Distraction-manipulation, most often used by chiropractors and physical therapists, is performed on treatment tables that allow the operator to determine the moment-to-moment vector and timing of the distractive force. These techniques include FD (Cox technique), Leander technique, and Saunders Active Trac method, among others. [17]
Differential Diagnosis[edit | edit source]
In an effort to maximize conservative treatment in a population with higher rates of progression to costly interventions, such as surgery and injections, a trial of traction could be considered for patients who have a preference for this treatment or who are unresponsive to other physical therapy interventions. Summary evidence in recent systematic reviews and clinical practice guidelines concludes that mechanical lumbar traction is not effective for treating acute or chronic nonspecific low back pain (LBP). However, many physical therapists continue to use it, primarily as an additional modality.[18] Indeed, expert clinical opinion, theoretical models, and some research evidence suggest that certain patients with LBP respond positively to traction. A study published in the March 2016 issue of JOSPT investigates the effectiveness of traction in prone as an adjunct to an extension-oriented exercise program in patients with LBP and leg pain and explores whether a previously identified set of patient characteristics is associated with better outcomes from traction.[19]
- Low back pain - Either alone or in combination with other treatments, traction has little or no impact on pain intensity, functional status, global improvement and return to work among people with low back pain.[20]
- Lumbar disc herniation - Herniated lumbar disks are the central cause of sciatica. Cohort studies suggest that the condition of many patients with a herniated lumbar disk improves in 6 weeks. In other words a conservative therapy is generally recommended for 6 weeks in the absence of a major neurologic deficit. There is no proof that conservative treatments change the natural history but some offer slight relief of symptoms. A few examples are NSAIDs (= reduce back pain, but they have a less clear benefit in patients with sciatica). A meta-analysis of 32 randomized trials showed no significant benefit of lumbar traction.[21]
- Sciatica - Traction and exercise therapy were significantly inferior to surgery. [22]
Outcome Measures[edit | edit source]
The McGill Pain Questionnaire (MPQ) is a self-reporting measure of pain used for patients with a number of diagnosis. It is composed of 78 words, of which respondents choose those that best describe their experience of pain. [23]
The Roland-Morris Disability Questionnaire (RMDQ) is designed to assess self-rated physical disability caused by low back pain.[24]
Oswestry Low Back Pain Disability Questionnaire is to assess pain-related disability in persons with low back pain (LBP). It consists of 10 questionnaires about how pain affects daily activities, scored from 0 to 5 for each section, with higher values indicating more severe impact; and a 12-item short-form health survey (SF-12) that consists of 12 questions concerning general health and can be divided into two aggregate summary measures: the physical component summary (PCS) and the mental component summary (MCS). [9]
VAS-pain: intensity of pain. which is a horizontal scale graded from zero, representing no pain, to 100mm, re- presenting the worst imaginable pain.VAS-Lu: intensity of pain for lumbar pain. VAS-Le: intensity of pain for leg pain. [9]
Numerical pain rating scale (NPRS): on a box scale from 0–10 describing ‘usual level of pain in the last week’.[25]
Numerical rating scale of limitation of activities (NLARS) on a box scale from 0–10 describing ‘ability to perform usual activities in the last week’. [25]
Evidence
[edit | edit source]
Lumbar traction is used in many disorders of the low back.
Lumbar disc herniation:
Several studies have investigated the effect of lumbar traction on lumbar disc herniation. Tesio et al (1993)[26] demonstrated that autotraction showed continued improvement after three months, pain ratings remained stable but disability scores decreased to 0 to 23% of the pretreatment value. Autotraction does not change the location and size of an herniation but there is an marked clinical improvement in the patients.[27] According to Ljunggren et al. autotraction and manual traction are equally efficient, in both treatments the pain intensity was significantly reduced.[28] Mechanical lumbar traction as additional therapy to extension exercises facilitates the patient’s improvement in pain and return to prior level of function. After 5 weeks patients no longer experience low back pain and improved in terms of functional status and pain-related disability.[29] Lumbar traction in combination with a physical therapy program also gives a decrease in the size of herniated disc material.[30] Unlike the previous studies, Rattanatharn et al. showed no benefit of traction (together with routine conservative treatment) for patients with acute herniated disc syndrome.[31] Both the traction group and the sham traction group had improvement of their symptoms, which means the patients can be treated conservatively at home with proper instructions.
Low back pain:
Several studies found no positive effect of lumbar traction for low back pain. There is no improvement in functional status, pain, range of motion and work absence due to lumbar traction (compared with sham traction).[32] Also the addition of intermittent mechanical traction to a standard graded activity program gives no extra advantages for people with low back pain. There is no difference in outcome of the graded activity program with or without the lumbar traction.[7] Borman et al. had the same effect in their study: no specific effect of traction in standard physical therapy for low back pain was observed.[33]
Although previous conclusions give no benefit to lumbar traction for low back pain, Cai et al.[34] searched prediction rules for those patients who have an improvement. The presence of non-involvement of manual work, low level fear-avoidance beliefs, no neurological deficit and age above 30 years increase the probability of response to mechanical lumbar traction.
Lumbago - sciatica:
In the treatment of lumbago – sciatica lumbar autotraction is a better method than the use of a corset and rest. It gave an immediate relief of pain and a normalizing of the SLR test, also after three weeks.[35]Autotraction has also an improvement in long term results for people with chronic lumbago and sciatica.[27]
How much % of body weight must be used?[edit | edit source]
In deciding what traction weight to apply, one must consider 2 aspects:
- what weight will overcome friction between the body and the bed; and
- what amount of force is required to exert an effect on the lumbar spine. Judovich showed that a traction force of 26% of the patient’s body weight was required to overcome friction. The use of a split tabletop with friction-free rollers reduces this to a negligible amount. In its absence, a force in excess of 26% of the body weight must be used before any effect can be produced at the lumbar spine. [36]
Optimal weights for traction have been investigated by assuming that intervertebral widening or reduction of disk protrusion achieves the effect of traction; however, only the former has been demonstrated experimentally. Despite the studies, it remains unclear what magnitude of force is required to cause the desired effect in the intact human spine. The mechanism by which traction may have its effects is not fully understood, and the neuromodulation of pain, which may require very low weight, must also be considered as a possible effect. This notwithstanding, clinical experts recommend using motorized traction on a friction-free surface and advocate a wide range of traction weights within their treatment regimes. Maitland suggests 10 to 65kg, with an average of 30 to 45kg; Cyriax suggests 40 to 85kg; Grieve suggests 13 to 34kg; and Hicklings suggests 32 to 68kg. [36]
Of all kinds motorized traction is the most interesting, because it is the only type of traction that can be adequately standardized and is commonly used in clinical practice. It is also the only form of traction that can be adequately standardized in respect to weight applied. . [36]
Placebo comparison[edit | edit source]
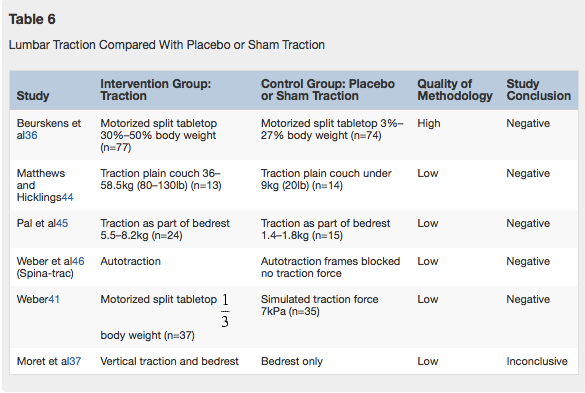
From a systematic review[36] six studies compared traction with sham traction (table 6). Sham traction is a low-weight or placebo traction that the given researcher considers to be ineffective. Three studies used motorized traction (2 on a split tabletop, 1 on a plain tabletop)), 1 used autotraction, 1 used gravitational traction, and 1 used traction as part of bedrest. Only the study by Beurskens et al was of a high quality, and all gave negative results except for the inconclusive result of Moret et al.[36]
Clinical Bottom Line[edit | edit source]
Lumbar traction is used by physiotherapist for threatening patients with low back pain and leg pain. There are different types of lumbar traction: mechanical traction, autotraction and manual traction. There had been shown that lumbar traction reduce nucleus pulposus pressure. Lumbar traction can be used in many disorders of the low back: lumbar disc herniation, low back pain and lumbago-sciatica. A few clinical trials still questioned the effectiveness of lumbar traction.
Presentations[edit | edit source]
 |
Evidence for the Use of Traction in Patients with Low Back Pain
This presentation, created by Leigh Langerwerf as part of the Evidence in Motion Fellowship, discusses the current best evidence for lumbar traction. Evidence for the Use of Traction in Patients with Low Back Pain |
References[edit | edit source]
- ↑ Lee RY et al. Loads in the lumbar spine during traction therapy. Australian Journal of Physiotherapy. 2001; 47(2): 102-108. (LEVEL 3B)
- ↑ 2.0 2.1 2.2 2.3 2.4 Pellecchia GL et al. Lumbar traction: A review of the literature. J Orthop Sports Phys Ther. 1994 Nov;20(5):262-267. (LEVEL 1A)
- ↑ 3.0 3.1 Saunders HD. Lumbar traction*. J Orthop Sports Phys Ther. 1979; 1(1): 36-45. (LEVEL 1A)
- ↑ 4.0 4.1 http://www.surgery-lumbar.com/lumbar_traction(level of evidence 5)
- ↑ 5.0 5.1 http://emedicine.medscape.com/article/1899031-overview(Level of evidence: 5)
- ↑ 7.0 7.1 7.2 7.3 Schimmel JP et al. No effect of traction in patients with low back pain: a single centre, single blind, randomized controlled trial of Intervertebral Differential Dynamics Therapy. Eur Spine J. 2009 (18): 1843-1850. (LEVEL 1B)
- ↑ 8.0 8.1 Nikoobakht, M., et al., Plasma disc decompression compared to physiotherapy for symptomatic contained lumbar disc herniation: A prospective randomized controlled trial, neurologia i neurochirurgia polska 50 (2016) 24–30 (Level of evidence: 1B)
- ↑ 9.0 9.1 9.2 Konstantinovic, L.M., et al., Acute Low Back Pain with Radiculopathy: A Double-Blind, Randomized, Placebo-Controlled Study, Photomedicine and Laser Surgery Volume 28, Number 4, 2010 (level of evidence: 1B)
- ↑ Cox JM, Feller J, Cox-Cid J. Distraction chiropractic adjusting: clinical application and outcomes of 1,000 cases. Topics Clin Chiropractic 1996;3:45–59. (level of evidence 3a)
- ↑ Knutsson E, Skoglund CR, Natchev E. Changes in voluntary muscle strength, somatosensory transmission and skin temperature R.E. Gay and J.S. Brault / The Spine Journal 8 (2008) 234–242 241
- ↑ Ramos G, Martin W. Effects of vertebral axial decompression on intradiscal pressure. J Neurosurg 1994;81:350–3. (level of evidence 2b)
- ↑ 13.0 13.1 Gudavalli MR, Cox JM, Baker JA, Cramer G, Patwardhan AG. Intervertebral disc pressure changes during a chiropractic procedure. Adv Bioeng 1997;36:215–6. (level of evidence 3a)
- ↑ MacLean JJ, Lee CR, Alini M, Iatridis JC. The effects of short-term load duration on anabolic and catabolic gene expression in the rat tail intervertebral disc. J Orthop Res 2005;23:1120–7. (level of evidence 2b)
- ↑ Kroeber M, Unglaub F, Guehring T, et al. Effects of controlled dynamic disc distraction on degenerated intervertebral discs: an in vivo study on the rabbit lumbar spine model. Spine 2005;30:181–7. (level of evidence 2a)
- ↑ Iatridis JC, MacLean JJ, Ryan DA. Mechanical damage to the intervertebral disc annulus fibrosus subjected to tensile loading. J Biomech 2005;38:557–65. (level of evidence 1b)
- ↑ 17.0 17.1 Ralph E. Gay, et al. Evidence-informed management of chronic low back pain with traction therapy. The Spine Journal 8 (2008) 234–242 (level of evidence 1a)
- ↑ Madson TJ, Hollman JH. Lumbar traction for managing low back pain: a survey of physical therapists in the United States. J Orthop Sports Phys Ther. 2015;45:586-595. http://dx.doi. org/10.2519/jospt.2015.6036 (level of evidence 3b)
- ↑ Thackeray A, Fritz JM, Childs JD, Brennan GP. The effectiveness of mechanical traction among subgroups of patients with low back pain and leg pain: a randomized trial. J Orthop Sports Phys Ther. 2016;46:144-154. http://dx.doi. org/10.2519/jospt.2016.6238 (level of evidence 1a)
- ↑ Wegner I, Widyahening IS, van Tulder MW et.al. Traction for low-back pain with or without sciatica. Cochrane Database systematic review. (2013 aug 19). https://www.ncbi.nlm.nih.gov/pubmed/23959683 (Level of evidence: 1a)
- ↑ Deyo RA, Mirza SK. Clinical practice – Herniated Lumbar Intervertebral Disk. N Engl J Med. (2016 May 5). http://www.nejm.org/doi/10.1056/NEJMcp1512658 (Level of evidence: 5 )
- ↑ Ruth A. Lewis et. al, Comparative clinical effectiveness of management strategies for sciatica: systematic review and network meta-analyses. The Spine Journal. Volume 16. (2015 June 1). http://www.sciencedirect.com/science/article/pii/S1529943013014976 (Level of evidence: 1a)
- ↑ http://www.physio-pedia.com/McGill_Pain_Questionnaire (level of evidence: 2A)
- ↑ http://www.physio-pedia.com/Roland%E2%80%90Morris_Disability_Questionnaire (level of evidence: 2A)
- ↑ 25.0 25.1 Glazov, G., et al., Low-dose laser acupuncture for non-specific chronic low back pain: a double-blind randomised controlled trial, Acupunct Med, 2014;32:116–123 (Level of evidence: 1B)
- ↑ Tesio L et al. Autotraction versus passive traction: an open controlled study in lumbar disc herniation. Arch Phys Med Rehabil. 1993 Aug; 74(8): 871-876. (LEVEL 1B)
- ↑ 27.0 27.1 Gillström P et al. Autotraction in lumbar disc herniation. A myelographic study before and after treatment. Arch Orthop Trauma Surg. 1985; 104(4): 207-210. (LEVEL 1B) Cite error: Invalid
<ref>tag; name "Gillström" defined multiple times with different content - ↑ Ljunggren AE et al. Autotraction versus manual traction in patients with prolopsed lumbar intervertebral discs. Scand J Rehabil Med. 1984; 16(3): 177-124. (LEVEL 1B)
- ↑ Gagne AR et al. Lumbar extension exercises in conjunction with mechanical traction for the management of a patient with a lumbar herniated disc. Physiother Theory Pract. 2010 May; 26(4): 256-266. (LEVEL 3B)
- ↑ Ozturk et al. Effect of continuous lumbar traction on the size of herniated disc material in lumbar disc herniation. Rheumatol Int. 2006 May; 26(7): 622-626. (LEVEL 1B)
- ↑ Rattanatharn R et al. Effectiveness of lumbar traction with routine conservative treatment in acute herniated disc syndrome. J Med Assoc Thai. 2004 Sep; 87 (2): 272-277. (LEVEL 1B)
- ↑ Beurskens AJ et al. Efficacy of traction for nonspecific low back pain, 12-week and 6-month result of a randomized clinical trial. Spine. 1997 Dec1; 22(23): 2756-2762. (LEVEL 1B)
- ↑ Borman P et al. The effect of lumbar traction in the management of patients with low back pain. Rheumatol Int. 2003; 23(2): 82-86. (LEVEL 1B)
- ↑ Cai C et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with mechanical lumbar traction. Eur Spine J. 2009; 18(4): 554-561. (LEVEL 1B)
- ↑ Larsson U et al. Auto-traction for the treatment of lumbago-sciatica, a multicentre controlled investigation. Acta orthop Scand. 1980; 51; 791-798. (LEVEL 1B)
- ↑ 36.0 36.1 36.2 36.3 36.4 Harte, A., et al.,The efficacy of traction for back pain: a systematic review of randomized controlled trials, Arch Phys Med Rehabil, Volume 84, Issue 10, Pages 1542–1553 October 2003 (Level of evidence: 1A)