Lumbar Instability
Original Editors - Anke Jughters,
Top Contributors - Sam Van de Mosselaer, Tessa de Jongh, Anke Jughters, Andeela Hafeez, Admin, Kim Jackson, Lucinda hampton, Simisola Ajeyalemi, Rachael Lowe, Kai A. Sigel, WikiSysop, 127.0.0.1, Tony Varela, Elien Clerix, Vandoorne Ben, Liese Bosman, Shaimaa Eldib, Tony Lowe, Elaine Lonnemann, Robert Pierce and Mats Vandervelde
Definition/Description[edit | edit source]
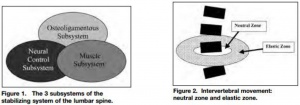
Lumbar instability is an important cause of low back pain and can be associated with substantial disability.[1] The word ‘instability’ is still poorly defined. But it is most widely believed that the loss of a normal pattern of spinal motion causes pain and/or neurologic dysfunction. The American Academy of Orthopaedics Surgeons [2] state: ‘Segmental instability is an abnormal response to applied loads, characterized by motion in motion segments beyond normal constraints.’ Panjabi published a spinal stabilization system represented by 3 subsystems: the passive, the active and the neural control subsystem.[1]
Segmental instability is defined by Panjabi [3] “as a significant decrease in the capacity of the stabilizing system of the spine to maintain the intervertebral neutral zones within the physiological limits so that there is no neurological dysfunction, no major deformity, and no incapacitating pain.”The ability to maintain an efficient coordination between these systems would allow the patient to function without undue stress on the tissues in the body. Panjabi suggests that a loss of integrity within the passive subsystem may make segments unstable unless the neuromuscular subsystem compensates for that loss.[4],[5], [4]
Within lumbar instability, we distinguish functional (clinical) instability and structural (radiografic) instability. [6] Functional instability, which can cause pain despite the absence of any radiological anomaly, can be defined as the loss of neuromotor capability to control segmental movement during mid-range. Whereas structural or mechanical instability can be defined as the disruption of passive stabilisers, which limit the excessive segmental end range of motion (ROM). There is also a possibility to have a combined instability.[4]
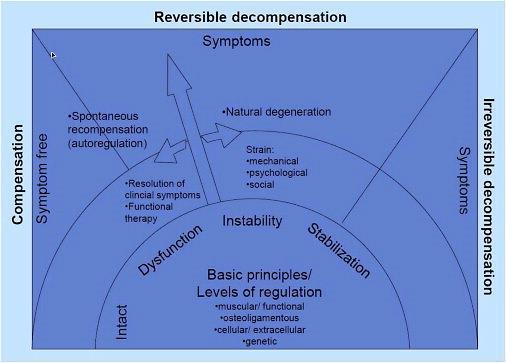
T. Barz etal. [1] proposed a new conceptual model of compensation/decompensation in lumbar segmental instability (LSI). In LSI, structural deterioration of the lumbar disc initiates a degenerative cascade of segmental instability (see figure 1). Over time, radiographic signs become visible (see etiology). Influenced by non-functional factors (psychosocial factors), functional elements of the spine (ligaments, muscles) allow a compensation of degeneration. This may lead to an alleviation of clinical symptoms. In return, the target condition of decompensation of LSI may cause the new occurrence of symptoms and pain. Individual differences of identical structural disorders could be explained by compensated or decompensated LSI leading to changes in clinical symptoms and pain.
Clinically Relevant Anatomy[edit | edit source]
The lumbar spine is intended to be very strong, so it can protect the sensitive spinal cord and spinal nerve roots and it has to carry the most weight. Having regard to the form of the joints in the lumbar region, flexion and extension are the main motion directions. [7] Panjabi’s spinal stabilization system[1],[8]:
- Passive subsystem: intervertebral disc, ligaments, facet joints and capsules, vertebrae and passive muscle support
- active subsystem: spinal muscles and tendons, thoracolumbar fascia
- neural control system: nerves and central nervous system
The passive subsystem plays its most important stabilizing role in the elastic zone (near end range) of spinal ROM. Flexion of the spine is mostly stabilized by the posterior ligaments (interspinous and supraspinous ligaments), the facet joints, the joint capsules and the intervertebral discs. End-range extension is stabilized primarily by the anterior longitudinal ligament, the anterior aspect of the annulus fibrosus and the facet joints. [5]
The neuromotor control subsystem controls segmental motion during the mid-range, while the osseoligamentous (passive) subsystem limits segmental motion at the extremes of lumbar motion.[9]
The neutral zone is defined as a portion of the total physiologic range of intervertebral motion. The total physiologic range involves a neutral zone and an elastic zone. The neutral zone, is the zone of movement close to the neutral position of the segment, a zone in ☃☃which movement occurs with little resistance. The elastic zone starts at the end of the neutral zone and stops at the end of physiologic range of motion. [4],[3]
For detailed anatomy: Lumbosacral Biomechanics
Epidemiology /Etiology[edit | edit source]
Lumbar spinal instability may be caused by [7] :
• degenerative disease
• facet joint hypertrophy
• postoperative status
• postoperative spinal fusion
• trauma to the spine or its surrounding structures
• development disorders, like scoliosis and other congenital spine lesions
• infection
• tumors
Abnormal segmental motion noted on kinetic MR images is closely associated with disc degeneration, facet joint osteoarthritis, and the pathological characteristics of interspinous ligaments, ligamentum flavum (hypertrophy) and paraspinal muscles. Other spine pathology such as annular tears or traction spurs has also been associated with segmental instability. [7]When a disorder or injury occurs, the whole motion segment is affected and the degenerative cascade begins which can lead to the symptoms and signs of LSI (see figure 2).
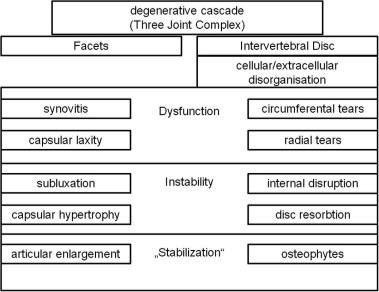
Figure 2 [7]
A constant morphological modification of the spine alters the biomechanical loading from back muscles, ligaments, and joints, and can harvest back injuries.[9]Granata et al., described that body mass, task asymmetry, and level of experience affected the scale and variability of spinal load during repeated lifting efforts.[4] In older people, bending and lifting activities produce loads on the spine that exceed the failure of vertebrae with low bone mineral density, which is linked with spinal degeneration. The degenerative transformation has influence on the intervertebral discs, ligament and bone.[9]
The estimated prevalence of low back pain due to lumbar segmental instability is about 33% for patients with functional instability, compared to 57% for patients with evidence of structural instability, as indicated by positive flexion–extension radiograph. [7], [9]
Characteristics/Clinical Presentation[edit | edit source]
Patients with lumbar instability are common patients with chronical recurrent low back pain, a constant nagging pain which gradually increases. This pain can also be a residue of acute complaints.[3] [LOE 2A]
There’s still a controversy about the exact meaning of the term lumbar instability. Cook et al. describe following subjective and objective signs& symptoms that could indicate lumbar instability:
Besides that, the following characteristics can indicate lumbar instability [3] [LOE 2A], [2] [LOE 2A]:
- The feeling of instability, giving way
- A visually observable or palpable hitch at a moving segment in the lumbar spine, mostly during change of position.
- Segmental shifts or hinging associated with the painful movement.
- Moving or jumping of the vertebra accompanied with pain in active trunk flexion or deflexion.
- An increased mobility at the concerned movement segment, mostly in passive segmental lumbar flexion and extension.
- Excessive intervertebral motion at the symptomatic level or an increased intersegmental motion at the level above the concerned movement segment.
- Local pain.
- Low back pain during long static load and deflexion.
- Pain during change of position and while bending or lifting.
- An abnormal motion sensation in postero-anterior movements of the vertebra.
- Decreased repositioning accuracy.
- Decreased postural control.
- Decreased activation of stabilizing muscles.
- Disruptions in the patterns of recruitment and co-contraction of the large trunk muscles (global muscle system) and small intrinsic muscles (local muscle system). This affects the timing of patterns of co-contraction, balance and reflexes.
- Pain and the observation of movement dysfunction within the neutral zone.
- A painful arc.
- Gowers sign: the inability to return to erect standing from forward bending without the use of the hands to assist this motion.
- Frequently crack or pop the back to reduce the symptoms, self-manipulation.
Differential Diagnosis[edit | edit source]
• Facet Joint Syndrome (arthritis of the facet joints)
• Osteoporosis
• Sciatica
Diagnostic Procedure[edit | edit source]
The diagnosis of lumbar instability is commonly based on the imaging finding of abnormal vertebral motion. This only shows anatomical instability and not functional instability. Abnormal translation and/or rotation around the x-, y-, and z-axes of the three-dimensional system by Panjabi and White can be found. Lumbar instability is mostly multidirectional, but the resulting displacement is evaluated in one plane at the time. Sagittal and coronal displacements are evaluated with radiographs, displacements on the axial plane are evaluated with computed tomographic (CT) or magnetic resonance (MR). [11][12][9]
Functional flexion-extension radiographs taken at the end-range of movement are the most frequently used, but show only the function of the passive stabilizing subsystem and fail to address the active and neural control subsystems.[5]
The relationship between imaging instability and its symptoms remains difficult to appoint. [11]
- Neutral radiography:[11]Shows many indirect signs that are associated with spinal instability.
- Functional radiography [11]: Functional radiography in the sagittal plane can occur in flexion and extension or with passive axial traction and compression. Intervertebral instability or abnormal motion between two vertebrae can be observed. Dynamic radiographs obtained in both flexion and extension, determine motion segment instability and can also indicate the lesions located in specific areas.
- Magnetic resonance imaging[11][6] MR imaging is commonly considered to be the most accurate imaging method for diagnosing degenerative abnormalities of the spine and is often used for the diagnosis of patients with chronic low back pain.
- Intraoperative measurement system[9] :This technique is recently developed and implies in vivo measurements of vertebral segment displacement during the application of a controlled load to produce motion.The operator grasps the spinous process to move it caudally. A device is developed to preserve the supraspinal ligament after clearing the paravertebral muscles and hammering the two pins into the two spinous processes lying on either side of the lumbar vertebrae so the stability can be measured.[7]
- Computed tomography[9]: CT can show spinal degenerative changes and facet joint orientation. It can demonstrate predisposing anatomic factors, such as facet joint asymmetry. If a CT scan shows a gap in the facet joints during rotation of the trunk, this could be an indirect sign of spinal instability.
- Quantitative Stability Index (QSI)[9] QSI is a novel objective test for sagittal plane lumbar instability. A QSI > 2 standard deviations from normal in an asymptomatic and radiographically normal population, would indicate that the amount of translation per degree of rotation is abnormal. A QSI = 4 would indicate far greater instability.
Outcome Measures[edit | edit source]
- Oswestry Disability Index: subjective percentage score of level of function (disability) in activities of daily living in those rehabilitating from low back pain.
Minimal detectable chance is 5-6 points and the minimum clinically important difference is 6 points.[9] Scores from 0% to 20% indicate minimal disability ,20% to 40%, moderate disability, 40% to 60%, severe disability; 60% to 80%, crippled 80% to 100%, bedbound or exaggerating [4]
- Quebec Back Pain Disability Scale:
The Quebec back pain disability scale (QBPDS) is a condition-specific questionnaire developed to measure the level of functional disability for patients with low back pain.[3] The end score will be between 0 (no limitation) and 100 (totally limited). The minimum clinically important difference is 15 points when suffering acute low back pain of chronic low back pain.[2]
- Roland Morris Disability Questionnaire:
This questionnaire is designed to assess self-rated physical disability caused by low back pain.
o When the score at intake is < 9 points; Minimal detectable change (MDC) = 6,7 points and the minimum clinically important difference (MCID) is 2-3 points.[7]
o When the score at intake is between 9-16: MDC = 4-5 points and MCID = 5-9 points.[11],[5]
o When the score at intake is > 16 points: MDC = 8,6 points and MCID = 8-13 points.[5]
MIC absolute cutoff, minimal important change = 5 points for patients with low back pain. MIC (% improvement from baseline) = 30%[6]
- Patient Specific Functional Scale:
This useful questionnaire can be used to quantify activity limitation and measure functional outcome for patients with any orthopaedic condition.[12] The Minimal detectable change (MDC) is for chronic pain = 2 points, for low back pain = 1,4 points and the minimum clinically important difference (MCID)= 2,0 points.[9]
Stratford et al[4] found the average of the MCID scores for 3 activities to be 0.8 (“small change”), 3.2 (“medium change”), and 4.3 (“large change”) PSFS points in patients with chronic low back pain. - Waddell Disability Index:
The WDI evaluates disability because of low back pain. The scale consists of nine items. These questions are answered with yes or no and are about impairments in activities of daily living (not related to a specific period). The final score is calculated by adding up positive items, and ranges from 0 to 9.21. ICCs = 0.79[2],[3]
Physical examination[edit | edit source]
The physical examination may consist of multiple tests :
• Low midline sill sign:
First there is an inspection of the midline of the patient’s low back to detect the low midline sill sign. If lumbar lordosis increases and there is a sill like a capital “L” on the midline, the test is considered positive. Next the examiner palpates the interspinous space and evaluates the position of the upper spinous process in relation to the lower spinosus process.[1] If the upper spinous process is displaced anterior to the lower spinous process, the test positive.[3]
 Figure 3
Figure 3
Interspinous gap change during lumbar flexion – extension motion:
This test is used for the detection of lumbar instability. First there is an inspection of the low back to detect the interspinous gap change. The patient stands shoulder – width, flex his back and place both hands on an examination table. After inspection of the lower back in flexion, palpates and evaluates the physiotherapist the width of the individual interspinous spaced and the position of the upper spinous process in relation to the lower one.[3]
After this, the physiotherapist will ask the patient to extend (to hollow) the low back while he evaluates the interspinous gap change during this motion. [7], [3] Figure 4
Figure 4
• Sit – to – stand test:[5]
The test is positive (there is an association with instability) if the person feels pain immediately when sitting down in a chair and if the pain is (partially) relieved by standing up. The test result might vary (time of the day, type of seat, the patients’ symptom levels before the test). Sensitivity: 30, specificity: 100, LR+: cannot be calculated and LR-: 0,7
• Passive Accessory Intervertebral Movements (PAIVM): [2]sensitivity: 46, specificity: 81 , LR+: 2,4 and LR-: 0,7
• Prone Instability Test : [2][7] has a sensitivity of 61, specificity: 57, LR+: 1,4 and LR-: 0,7
• Beighton score : [2] [7] has sensitivity of 36, specificity: 86, LR+: 2,5 and LR-: 0,8
• Passive Physiological Intervertebral Motion (PPIVM ):[2],[11]
The patient side lies. The test consisted of moving the patient’s spine through sagittal forward – bending ( flexion ) and backward – bending ( extension ) , using the lower extremities. Meanwhile, the examiner palpates between the spinous process of the adjacent vertebrae to assess the motion taking place at each motion segment. [5]
PPIVM (flexion): sensitivity: 5 specificity: 99,5 ,LR+: 8,7 and LR-: 1,0
PPIVM (extension): sensitivity: 16 ,specificity: 98 , LR+: 7,1 and LR-: 0,9
- Passive Lumbar Extension Test (PLE test ):
The patient is in prone position. The therapist elevates both lower extremities were elevated ( passive ) to a height of about 30cm. The knees maintain extended while gently pulling the legs. The examiner fixates T12 ventrocaudal. [2],[11]This test can also be done in lateral position of the patient with the legs bended. The test is positive if it provokes similar complaints. Sensitivity: 84, specificity: 90, LR+: 8,8 and LR-: 0,2
• Instability catch sign (active flexion test):
The patient bend his or her body forward as much as possible and then return to the neutral position. The test is positive when the patient isn’t able to return to the neutral position.[2], [15]This test is a provocation test. Sensitivity: 26, specificity: 86, LR+: 1,8 and LR-: 0,9[2]
• Painful catch sign :
The patient is in supine position and then the examiner asks the patient to lift both lower extremities. The knees must be extended. Then the examiner asks the patient to return slowly to the start position. If the lower extremities fell down instantly because of the low back pain , the test was positive. [5] Sensitivity: 37 ,specificity: 73, LR+: 1,4 and LR-: 0,9
•Apprehension sign :
The examiner asks the patient if he or she has a sensation of lumbar collapse because of the low back pain while performing ordinary acts like bending back and forward, bending from side to side, sitting down or standing up. The test was positive if the patient had a sensation of lumbar collapse. [5]The condition has a unique clinical presentation that displays its symptoms and movement dysfunction within the neutral zone of the motion segment. The loosening of the motion segment secondary to injury and associated dysfunction of the local muscle system renders it biomechanically vulnerable in the neutral zone. The clinical diagnosis of this chronic low back pain condition is based on the report of pain and the observation of movement dysfunction within the neutral zone and the associated finding of excessive intervertebral motion at the symptomatic level. Four different clinical patterns are described based on the directional nature of the injury and the manifestation of the patient's symptoms and motor dysfunction. A specific stabilizing exercise intervention based on a motor learning model is proposed and evidence for the efficacy of the approach provided.[16],[17] [11] Sensitivity: 18, specificity: 88, LR+: 1,6 and LR-: 0,9
In acute overt instability, stabilization of the spine is required in all cases. In this context, medical treatment refers to the use of external bracing for spine stabilization. If instability is due to an osseous fracture, if the fracture fragments can be reduced to near-anatomic alignment, and if there is no significant neural compression after reduction, the patient may be treated nonsurgically with a brace until the fracture heals.
In anticipated instability (eg, extensive discitis and osteomyelitis) The majority of the tests has high specificity but low sensitivity. Data suggest that PLE is the most appropriate tests to detect lumbar instability in specific LBP. The PLE test ( Passive Lumbar Extension test) has a sensitivity of 84% , a specificity of 90% , a LR+ rate of 8,8 and an LR- rate of 0,2.[18],[19],[5]
Medical Management[edit | edit source]
A significant subgroup within chronic low back pain patients, are the ones with lumbar segmental instability.[2] level of evidence 2A Medical treatment and surgery is more often recommended in chronic overt instability and covert instability, than in the other cases. When there’s no direct risk for neurological damage or side effect, the first medical treatment for patients with acute overt instability should be external bracing before surgery. This might even solve the patients complains when the cause for instability is a fracture of the spine.[3] level of evidence 4
But when conservative treatment fails, this may be reconsidered.
Another part of the medical treatment is medication. Depending on the complains of the patient and de physiological indication, analgesics, anti-inflammatories, muscle relaxants can be prescript.
Surgical management[edit | edit source]
Surgery should always be the last option, because it’s never without risks. The main problem of fusion is the disruption of the biomechanics of the rest of the spine; leading to adjacent level disease.[7]Level evidence: 1A There are different ways to fuse a spine segment.
- Anterior approach: The intervertebral disc is removed from a front approach (trough the abdomen) and replaced with bone graft or instrumentation.
Posterior approach: This surgery is either the same as the anterior approach, but from the back or there’s a fusion of a segment.
- Combined approach: In some cases, it’s not possible to complete the fusion only from the front or the back. In this scenario the surgeon will reach the spine from both sides.
- Instrumented fusion: Utilisation of titanium, titanium-alloy, stainless steel or non-metallic material to replace the intervertebral disc.
- Non-instrumented fusion: Also known as arthrodesis. This type of surgery uses bone graft to replace the original intervertebral disc.[9]
The existing literature does not identify significant differences between unilateral instrumentation or bilateral in the lumbar spine. The most used fusion is single-level.[5] There’s also growing evidence for the use of minimally invasive spine surgery (MIS) instead of open surgery.[6] Still the indications for surgery are controversial and more research is much needed. The main problem lies in the definition and the diagnosis of lumbar instability. [12]
However, despite the fact that indications for the procedure are uncertain, that costs and complication rates are higher than for other surgical procedures performed on the spine, and that long-term outcomes are uncertain, the rate of lumbar spinal fusion is increasing rapidly in the United States.[3] Level evidence: 2B,[2] Level evidence: 2A The rate of back surgery and especially of spinal fusion operations is at least 40% higher in the US than in any other country and is five times higher than in the UK.[7] Level evidence: 2B Although there have been no randomized trials evaluating the effectiveness of lumbar fusion for spinal instability, the feeling remains that the operation should be reserved for patients with severe symptoms and radiographic evidence of excessive motion (greater than 5 mm translation or 10° of rotation) who fail to respond to a trial of non-surgical treatment.[11] Level evidence: 4 The latter should consist of a combination of patient education, physical training and sclerosing injections.[5] Level evidence: 5
A good fusion still doesn’t guarantee pain relief, because the presence of micromotion between the vertebrae. [4] A solid fusion at one segment doesn’t prevent micromotion in the rest of the spinal unit. [1]
Physical Therapy Management[edit | edit source]
It’s important to understand Panjabi's hypothesis, that spinal stability is dependent on an interplay between the passive, active, and neural control systems. This indicates that you need to train different aspects to improve you spinal stability. The size of the neutral zone is also a better indicator of clinical spine instability than the overall range of motion. [4] Level of evidence: 2A
Patient education is important in the treatment of patients with segmental instability.This education should not only focus on the moments that the patient should not perform. But it should motivate the patient to stay active, knowing which movements shouldn’t be or with great care performed. These movements are loaded flexion movements, as they may create a posterior shift of the disc. [2] level of evidence 1A And any end-range positions of the lumbar spine should also be avoided because these overload the posterior passive stabilizing structures.
Physical therapy for segmental instability focuses on exercises designed to improve stability of the spine. As the lumbar erector spinae muscles are the primary source of extension torque for lifting tasks, strengthening of this muscle group has been supported.[7], level of evidence 1B
Intensive dynamic exercises for the extensors proved to be significantly superior to a regime of standard treatment of thermotherapy, massage and mild exercises in patients with recurrent LBP.[11],[5],[6], level of evidence 1B
The abdominal muscles, particularly the transversus abdominis and oblique abdominals, have also been proposed as having an important role in stabilizing the spine by co-contracting in anticipation of a tested load. However, exercises proposed to address the abdominal muscles in an isolated manner usually involve some type of sit-up manœuvre that imposes dangerously high compressive and shear forces on the lumbar spine [[12], level of evidence 5 ] and may provoke a posterior shift of the (unstable) disc (see figure 5).
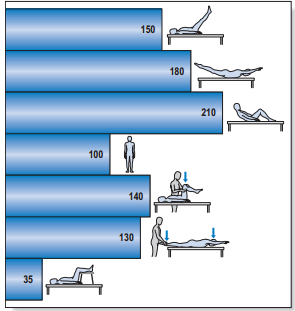
Figure 5: Intradiscal pressure in % of that of the standing position
Alternative techniques should therefore be tested when training these muscles. Some authors strongly suggest that the transversus abdominis [[9], level of evidence 2A ] and the multifidus muscles make a specific contribution to the stability of the lower spine [[4], level of evidence 2B ] [[1] , level of evidence 2A ] and an exercise programme that proposes the retraining of the co-contraction pattern of the transversus abdominis and multifidus muscles has been described. [[3] , level of evidence 1C ]
The exercise programme is based on training the patient to draw in the abdominal wall while isometrically contracting the multifidus muscle, and consists of three different levels:
• First, specific localized stabilization training is given. Lying prone, sitting and standing upright, the patient performs the isometric abdominal drawing-in manœuvre with co-contraction of the lumbar multifidus muscles. = Segmental control over primary stabilizers (mainly TrA, deep multifidus, pelvic floor and diaphragm) [[6], level of evidence 5 ]
During this phase we also teach the patient about locale segmental control.[3] A stabilizer is a very useful to teach this to your patient. The pressure should stay between 38 and 42 mmHg.[2] Level of evidence:4
• During the phase of general trunk stabilization, the co-contraction of the same muscles is carried out on all fours, and then elevating one arm forwards and/or the contralateral leg backwards, or on standing upright and elevating one arm forwards and/or bringing the contralateral leg backwards. =Exercises in closed chain, with low velocity and low load [[6] , level of evidence 5 ]
• Third, there is the stabilization training. Once accurate activation of the co-contraction pattern is achieved, training is given in functional movements, such as standing up from a sitting or lying position, bending forwards and backwards and turning. All daily activities are then integrated. A significant result from a randomized trial has recently been reported comparing this exercise programme with one of general exercise (swimming, walking, gymnastic exercises) in a group of patients with chronic LBP.[[2] , level of evidence 1B ]= Exercises in open chain, with high velocity and load [[6] level of evidence 5 ]
The training of this stabilisation muscles has positive results on pain control. Still it’s not entirely clear how this mechanism works. But we know that when the muscles contract, and especially when they do simultaneously, they compress the entire lumbar spine. This makes it harder for the joints and intervertebral discs to move in inefficient directions.[12] , level of evidence 2B The training creates a rigid cylinder around the spine. An exercises program should always be individualised accordingly to the patients (pain) complains. [9] , level of evidence 2A
For more information, see Exercises for Lumbar Instability
Back School[edit | edit source]
The effectivity of back school program for treatment of low back pain and functional disability has been shown and is more effective than any educational intervention in general health status and in decreasing acetaminophen and NSAID intake. It was ineffective in the other quality of life domains, in pain, functional status, anxiety and depression. [[2] , level of evidence 1B ] Back school should be a part of the physical treatment, next to exercise and physical treatment modalities. [4], level of evidence: 1B
Moderate evidence suggested that back schools have better short- and intermediate-term effects on the functional status and pain than other treatments for patients with recurrent and chronic low back pain (LBP) Moderate evidence suggests that a back school for chronic LBP in an occupational setting are even more effective than the other treatments.
Acupuncture, back schools, behavioural therapy, and spinal manipulation may reduce pain in the short term, but effects on function are unclear. In this systematic review, they don't know whether back schools are more effective than placebo gel, waiting list, no intervention, or written information at reducing pain ( low-quality evidence ). Compared with other treatments: They don't know whether back schools are more effective than spinal manipulation, non-steroidal anti-inflammatory drugs (NSAIDs), physiotherapy, calisthenics, or exercise at reducing pain (low-quality evidence). [[12], Level of evidence: 1A]
Key Research[edit | edit source]
• McGill SM. Estimation of force and extensor moment contributions of the disc and ligaments at L4–L5. Spine 1988;13:1395–402. Level of evidence: 1A
• Callaghan JP, Gunning JL, McGill SM. The relationship between lumbar spine load and muscle activity during extensor exercises. Phys Ther 1998;78:8–18. Level of evidence: 1B
• Manniche C, Hesselsoe G, Bentzen L, et al. Clinical trial of intensive muscle training for chronic low back pain. Lancet 1988;24– 31;2(8626–8627):1473–1476. Level of evidence: 1B
• Manniche C, Lundberg E, Christensen I, et al. Intensive dynamic back exercises for chronic low back pain: a clinical trial. Pain 1991;57:53–63.Level of evidence: 1B
• Hansen FR, Bendix T, Skov P, et al. Intensive dynamic back-muscle exercises, conventional physiotherapy, or placebocontrol treatment of low back pain. Spine 1993;18:98–107. Level of evidence: 1B
• O’Sullivan PB, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 1997;22: 2959–67.Level of evidence: 1B
• L.H. Ribeiro, F. Jennings, A. Jones, R. Furtado, J. Natour. Effectiveness of a back school program in low back pain. Clinical and Experimental Rheumatology 2008; 26: 81-88. Level of evidence: 1B
Resources[edit | edit source]
http://www.allaboutbackandneckpain.com/understandingconditions/segmentalinstability.asp
http://emedicine.medscape.com/article/310353-differential
Clinical Bottom Line[edit | edit source]
Patient education may be important in the treatment of patients with segmental instability. Education should, first of all, focus on preventing loaded flexion movements, as they may create a posterior shift of the disc. Therapy and exercises are useful.
The effectivity of back school program has been shown and is more effective than any educational intervention. The exercise programme is based on training the patient to draw in the abdominal wall while isometrically contracting the multifidus muscle, and consists.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 T. Barza, M. Melloh etal. A conceptual model of compensation/decompensation in lumbar segmental instability. Medical Hypotheses. Volume 83, Issue 3, September 2014, Pages 312–316 Level of evidence: 4
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 American Academy of Orthopaedic Surgeon : A glossary on spinal terminology. Chicage 1985
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Dis. 1992;5:390-397. Level of evidence: 4
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Biely SA, Smith SS, Silfies SP. Clinical instability of the lumbar spine: diagnosis and intervention. Orthpaedic Physical Therapy Practice. 2006;18:11-19. Level of evidence: 4
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Lumbar instability. Elsevier et al. Chapter 37, p523 – 529, 2013. Level of evidence: 5
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 18.Beazell J. R. (2010). Lumbar instability: an evolving and challenging concept. J Man Manip Ther., 18(1), p. 9–14 Level of evidence: 2A
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 Kisher, S. Lumbar Spine Anatomy (overview), 2015. Level of evidence: 5
- ↑ Panjabi MM. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Dis. 1992;5:390-397. Level of evidence: 4
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 80. Alyazedi FM, Lohman EB, Wesley Swen R, Bahjri K. The inter-rater reliability of clinical tests that best predict the subclassification of lumbar segmental instability: structural, functional and combined instability. The Journal of Manual & Manipulative Therapy. 2015;23(4):197-204. Level of evidence: 3B
- ↑ Physiotutors. Lumbar Spine Instability | Symptoms, Assessment and Diagnosis. Available from: https://www.youtube.com/watch?v=9uns1OrBUG8
- ↑ 11.00 11.01 11.02 11.03 11.04 11.05 11.06 11.07 11.08 11.09 11.10 Leone A. (2007). Lumbar Intervertebral Instability: A Review. Radiology, 245(1) Level of evidence: 2A
- ↑ 12.0 12.1 12.2 12.3 12.4 12.5 Nizard R. S. (2001). Radiologic assessment of lumbar intervertebral instability and degenerative spondylolisthesis. Radiol Clin North Am, 39(1), p. 55-71 Level of evidence: 2A
- ↑ Physiotutors. Low Midline Sill Sign / Slipping Palpation | Spondylolisthesis. Available from: https://www.youtube.com/watch?v=sND1YsNZhzo
- ↑ Physiotutors. Interspinous Gap Change | Lumbar Spine Instability. Available from: https://www.youtube.com/watch?v=Jk1MxlQ98Us
- ↑ Kasai, Yuichi, et al. "A new evaluation method for lumbar spinal instability: passive lumbar extension test." Physical therapy 86.12 (2006): 1661-1667.fckLRLevel of evidence: 3b
- ↑ P.B. O'Sullivan. Masterclass. Lumbar segmental ‘instability’: clinical presentation and specific stabilizing exercise management. Manual therapy Volume 5, Issue 1, Pages 2–12, February 2000. Level of evidence: 2B
- ↑ James R Beazell, Melise Mullins and Terry L Grindstaff .Lumbar instability: an evolving and challenging concept. J Man Manip Ther. 2010 Mar; 18(1): 9–14. Level of evidence: 2A
- ↑ Abdullah M .Alqarni et al. Clinical tests to diagnose lumbar segmental instability : a systematic review. Journal of orthopaedic and sports physical therapy. March 2011. Level of evidence : 2A
- ↑ Ferrari et al. A literature review of clinical tests for lumbar instability in low back pain : validity and applicability in clinical practice. Chiropractic & Manual Therapies. 2015. Level of evidence : 2A