Levator Ani Muscle
Original Editor - Agoro Bukola Zainab
Top Contributors - Agoro Bukola Zainab and Leana Louw
Description[edit | edit source]
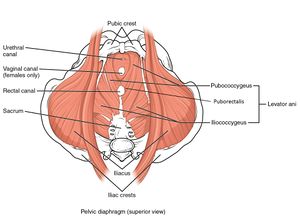
Levator ani muscle is the largest component of the pelvic floor. It is a broad muscular sheet that attaches to the bodies of the pubic bones anteriorly, ischial spines posteriorly and to a thickened fascia of the obturator internus muscle.[1] The levator ani muscle provides support to the pelvic visceral structures and play an important role in urinary voiding, defecation and sexual function. It consists of three parts: puborectalis, pubococcygeus and iliococcygeus muscle.[2]
Anatomy[edit | edit source]
Structure[edit | edit source]
Puborectalis is a thick narrow, medial part of the levator ani. It forms a U-shaped muscular sling around and behind the rectum, just cephalad to the external sphincter.[1]
Pubococygeus, also known as pubovisceral is the wider but thinner intermediate part of the levator ani. Within the pubovisceral muscle are parts that attach to the perineal body (puboperineal), a part that inserts into the anal canal (puboanal), and pubovaginal which inserts into the vaginal wall.
Iliococcygeus is a thin sheet of muscle that traverses the pelvic canal from the tendinous arch of the levator ani to the midline iliococcygeal raphe where it joins with the muscle of the other side and connects with the superior surface of the sacrum and coccyx.[3]
Origin and Insertion[edit | edit source]
| Origin | Insertion | Action | |
| Pubococcygeal
(Pubovisceral) |
|||
|
Pubis | Perineal body | Tonic activity pulls perineal body ventrally towards pubis |
|
Pubis | Vaginal wall at the level of the mid-urethra | Elevates vagina in region of mid-urethra |
|
Pubis | Intersphineteric groove between internal and external anal sphincter to end in the anal skin | Inserts into the intersphinteric groove to elevate the anusand its attached anoderm |
| Puborectal | Pubis | Sling behind rectum | Forms the sling behind the rectum forming the anorectal angle and closing the pelvic floor |
| Iliococcygeal | Tendinous arch of the levator ani | Two sides fuse in the iliococcygeal raphe | The two sides form a supportive diaphragm that spans the pelvic canal |
Nerve[edit | edit source]
- Nerve to the levator ani (branches of S4)
- Inferior anal (rectal) nerve
- Coccygeal plexus[1]
Artery[edit | edit source]
Blood supply to the levator ani muscle come from branches of the:[2]
- Inferior gluteal artery
- Inferior vesical artery
- Pudendal artery
Function[edit | edit source]
- The major function of Levator ani is to provide support to the pelvic viscera and also resist increses in intra-abdomial pressure.[1]
- Puborectalis muscle acts in association with the internal and external anal sphincter during the process of defecation
- Pubococcygeus muscle supports the vagina and prostrate in females and males, respectively. It aids ejaculation and assists in proper positioning of the fetus head.[5]
- Iliococcygeus which meets the fibers from the opposite side at the midline raphe provides a secure anchoring for the pelvic floor.[2]
Clinical relevance[edit | edit source]
- Vagina birth increases the likelihood of a woman having pelvic floor dysfunction.[6] The levator ani muscles and pelvic floor undergo remarkable changes during the second stage of labour to dilate sufficiently for the fetal head to be delivered.[7] Studies have shown that 13% to 36% of women after vaginal birth had injury to the levator ani muscle.[8][9][10] The studies involved the examination of women before and after vaginal birth using 3D ultrasound. Factors such as use of forceps, increased second stage length and larger head circumference were associated with increased risk of injury.
- Pelvic Organ Prolapse[11]
- Levator Ani Syndrome[2]
Assessment[edit | edit source]
Palpation[edit | edit source]
Assessing for levator muscle tear and contraction is possible through palpation even though it requires experience and skills to be able to discern muscle integrity, scarring and the width between the medial borders of the pelvic floor muscles.
The morphological integrity of puborectalis is assessed by placing the palpating finger parallel to the urethra with the tip of the finger at the bladder neck, and its palmar surface pressed against the posterior/dorsal surface of the symphysis pubis.[12]
Evaluation of Pelvic floor muscle function and strength
Treatment[edit | edit source]
Treatment includes electrogalvanic stimulation, sitz bath, biofeedback, to relieve pain and spasm in the levator ani.[13] Pelvic floor muscle training, also known as kegel exercises is done to strengthen the pelvic floor muscles which includes the levator ani.[2] Find out more on kegel exercises in the links below.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Moore KL, Dalley AF. Clinically oriented anatomy. Wolters kluwer india Pvt Ltd; 2018 Jul 12.
- ↑ 2.0 2.1 2.2 2.3 2.4 Gowda SN, Bordoni B. Anatomy, Abdomen and Pelvis, Levator Ani Muscle. InStatPearls [Internet] 2020 Mar 27. StatPearls Publishing.
- ↑ 3.0 3.1 Ashton-Miller J, DeLANCEY JO. Functional anatomy of the female pelvic floor. Bø K, Berghmans B, Mørkved S, van Kampen M, Evidence based physical therapy for the pelvic floor—Bridging science and clinical practice. 2014 Nov 4:19-33.
- ↑ Levator Ani Muscle - Origin, Insertion & Function. Available from: https://www.youtube.com/watch?v=ZaIRPhXavVg&list=WL&index=2&t=15s [last accessed 18/9/2020]
- ↑ Wu QK, Mao XY, Luo LM, Ying T, Li Q, Teng YC. Characteristics of pelvic diaphragm hiatus in pregnant women with stress urinary incontinence detected by transperineal three-dimensional ultrasound. Zhonghua fu chan ke za zhi. 2010 May;45(5):326.
- ↑ Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Urinary incontinence after vaginal delivery or cesarean section. New England Journal of Medicine. 2003 Mar 6;348(10):900-7.
- ↑ Bø K, Sherburn M, Vodušek DB. Measurement of pelvic floor muscle function and strength and pelvic organ prolapse. Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice. 2014;2:47-53.
- ↑ Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG: An International Journal of Obstetrics & Gynaecology. 2010 Nov;117(12):1485-92.
- ↑ Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO. Obstetrical factors associated with levator ani muscle injury after vaginal birth. Obstetrics and gynecology. 2006 Jan;107(1):144.
- ↑ Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstetrics & Gynecology. 2005 Oct 1;106(4):707-12.
- ↑ DeLancey JO, Morgan DM, Fenner DE, Kearney R, Guire K, Miller JM, Hussain H, Umek W, Hsu Y, Ashton-Miller JA. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstetrics & Gynecology. 2007 Feb 1;109(2):295-302.
- ↑ Dietz HP, Halban, Lee D, Gainey, Dietz, Kearney, Dietz, Valsky, Lien, Svabik, Shek. Pelvic floor muscle trauma. Expert Review of Obstetrics & Gynecology. 2010 Jul 1;5(4):479-92.
- ↑ Ng CL. Levator ani syndrome - a case study and literature review. Aust Fam Physician. 2007 Jun;36(6):449-52