Lateral Epicondylitis
Original Editors - Hannah Norton
Top Contributors - Angeliki Chorti, Adam Vallely Farrell, Admin, Charlotte Sirago, Elien Vanderlinden, Nikhil Benhur Abburi, Vanwymeersch Celine, Johnathan Fahrner, Kim Jackson, Celien Van den Meerssche, Rachael Lowe, Evan Thomas, Hannah Norton, Assia Dad, Ruben Vellemans, Simisola Ajeyalemi, Kai A. Sigel, Wanda van Niekerk, Maëlle Cormond, Pacifique Dusabeyezu, Quentin Desantoine, Jelien Wouters, Naomi O'Reilly, Irene Leahy, Jolien Rottie, Wendy Walker and Candace Goh
Description[edit | edit source]
Lateral epicondylitis, also known as "Tennis Elbow", is the most common overuse syndrome in the elbow. It is a tendinopathy injury involving the extensor muscles of the forearm. These muscles originate on the lateral epicondylar region of the distal humerus. In a lot of cases, the insertion of the extensor carpi radialis brevis is involved.
It should be remembered that only 5% of people suffering from tennis elbow relate the injury to tennis! Contractile overloads that chronically stress the tendon near the attachment on the humerus are the primary cause of epicondylitis. It occurs often in repetitive upper extremity activities such as computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration. Despite the name you will also commonly see this chronic condition in other sports such as squash, badminton, baseball, swimming and field throwing events. People with repetitive one-sides movements in their jobs such as electricians, carpenters, gardeners also commonly present with this condition.[1][2] [3][4][5]
Clinically Relevant Anatomy[edit | edit source]
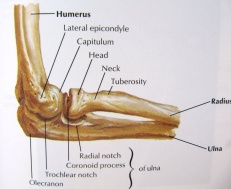
The elbow joint is made up of three bones: the humerus (upper arm bone), the radius and ulna (two bones in the forearm). At the distal end of the humerus there are two epicondyles, one lateral (on the outside) and one medial (on the inside).
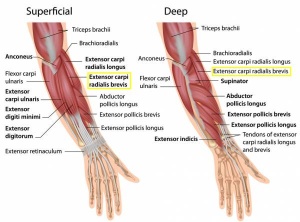
The area of maximal tenderness is usually an area just distal to the origin of the extensor muscles of the forearm at the lateral epicondyle. Most commonly, the extensor carpi radialis brevis (ECRB) is involved, but others may include the extensor digitorum, extensor carpi radialis longus (ECRL), and extensor carpi ulnaris.[6] [7]
The radial nerve is also in close proximity to this region, and divides into the superficial radial nerve and the posterior interosseous nerve.
Epidemiology/Aetiology[edit | edit source]
Lateral epicondylitis is classified as an overuse injury that may result in hyaline degeneration of the origin of the extensor tendon. Overuse of the muscles and tendons of the forearm and elbow together with repetitive contractions or manual tasks can put too much strain on the elbow tendons. These contractions or manual tasks require manipulation of the hand that causes maladaptions in tendon structure that lead to pain over the lateral epicondyle. Mostly, the pain is located anterior and distal from the lateral epicondyle.[3]
Epicondylitis occurs at least five times more often and predominantly occurs on the lateral rather than on the medial aspect of the joint, with a 4:1 to 7:1 ratio. It affects 1-3% of the population, with those 35-50 years old most commonly being affected. If a patient is <35 , it is important to consider differential diagnosis (growth plate disorder, referral from the cervical spine. If a patient is >50, consider OA, referred cervical spine pain. In a study by Nirschl, 1973, of 200 tennis players aged >30, 50% had symptoms of tennis elbow at some stage. [8]
This injury is often work-related, any activity involving wrist extension, pronation or supination during manual labour, housework and hobbies are considered as important causal factors.[9] Lateral epicondylitis is equally common in both sexes. Between the ages of 30-50 years the disease is most prevalent. Obtaining of the condition at the both lateral epicondyle is rare, the dominant arm has the greatest chance of the occurrence of lateral epicondylitis. Twenty percent of cases persist for more than a year. [6]
A systematic review identified 3 risk factors: handling tools heavier than 1 kg, handling loads heavier than 20 kg at least 10 times per day, and repetitive movements for more than 2 hours per day. Other risk factors are overuse, repetitive movements, training errors, misalignments, flexibility problems, ageing, poor circulation, strength deficits or muscle imbalance and psychological factors.[10]
There are several opinions concerning the cause of lateral epicondylitis:
1.Inflammation
Although the term epicondylitis implies the presence of an inflammatory condition, inflammation is present only in the earliest stages of the disease process. [11]
2. Microscopic tearing
- Nirschl and Pettrone attributed the cause to microscopic tearing with formation of reparative tissue (angiofibroblastic hyperplasia) in the origin of the extensor carpi radialis brevis (ECRB) muscle. This micro-tearing and repair response can lead to macroscopic tearing and structural failure of the origin of the ECRB muscle.
- That microscopic or macroscopic tears of the common extensor origin were involved in the disease process, was postulated by Cyriax in 1936.
- The first to describe macroscopic tearing in association with the histological findings were Coonrad and Hooper.
- Histology of tissue samples shows "collagen disorientation, disorganisation, and fibre separation by increased proteoglycan content, increased cellularity, neovascularisation, with local necrosis." Nirschl termed these histological findings bangiofibroblastic hyperplasia. The term has since been modified to bangiofibroblastic tendinosis. He noted that the tissue was characterised by disorganized, immature collagen formation with immature fibroblastic and vascular elements. This grey, friable tissue is found in association with varying degrees of tearing involving the extensor carpi radialis brevis.
3. Degenerative Process
The histopathological features of 11 patients who had lateral epicondylitis were examined by Regan et al. They determined that the cause of lateral epicondylitis was more indicative of a degenerative process than an inflammatory process. The condition is degenerative with increased fibroblasts, vascular hyperplasia, proteoglycans and glycosaminoglycans, and disorganized and immature collagen. Repetitive eccentric or concentric overloading of the extensor muscle mass is thought to be the cause of this angiofibroblastic tendinosis of the ECRB. Epicondylitis is a degenerative condition in which increased fibrolastic activity and granulation tissue formation occur within the tendon. [3] [4]
3. Hypovascularity
Because this tendinous region contains areas that are relatively hypovascular, the tendinous unit is unable to respond adequately to repetitive forces transmitted through the muscle, resulting in declining functional tolerance. [12]
Clinical Presentation[edit | edit source]
The most prominent symptom of epicondylitis lateralis is pain, this pain can be produced by palpation on the extensor muscles origin on the lateral epicondyle. The pain can radiate upwards along the upper arm and downwards along the outside of the forearm and in rare cases even to the third and fourth fingers. Furthermore it is also often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. [3] [4]
According to Warren, there are four stages on the development of this injury with regard to the intensity of the symptoms.
1. Faint pain a couple of hours after the provoking activity.
2. Pain at the end of or immediately after the provoking activity.
3. Pain during the provoking activity, which intensifies after ceasing that activity.
4. Constant pain, which prohibits any activity.[13]
Furthermore it is also often seen that the flexibility and strength in the wrist extensor and posterior shoulder muscles are deficient. At least patients report weakness in their grip strength or difficulty carrying objects in their hand, especially with the elbow extended. This weakness is due to finger extensor and supinator weakness. Some people have a sense of paralysis but this is rare.[13] [9][14]
Symptoms last, on average, from 2 weeks to 2 years. 89% of the patients recover within 1 year without any treatment except perhaps avoidance of the painful movements .(sport injuries)[15] [16][17]
Assessment[edit | edit source]
A thorough assessment and examination are key elements in ensuring that the correct treatment plan is implemented, enhancing the recovery process. The assessment should also include elements to exclude a differential diagnosis.
Subjective Assessment[edit | edit source]
- Onset of pain 24-72hours after provocative activity involving wrist extension
- Pain may radiate down forearm as far as the wrist and hand
- Difficulty with lift and grip (Pain+/- weakness)
- Changes in biomechanical factors- new tennis racquet, wet ball, overtraining, poor technique, shoulder injury[18][19]
Objective Assessment[edit | edit source]
- Pain and point tenderness over lateral epicondyle and/or 1-2cm distal to epicondyle
- Pain and weakness on resisted wrist extension
- Weakness on grip strength testing (Dynamometer)
- Pain and/or decreased movement on passive elbow extension, wrist flexion and ulnar deviation and pronation
- Weak elbow extensors and flexors[18][19]
Differential Diagnosis[edit | edit source]
- Radial Tunnel Syndrome [20]
- Pain in the posterolateral area of the forearm
- Pain sometimes spreads to the dorsal side of the wrist
- Parasthesia
- Weakness (overuse injuries of the musculoskeletal system)
- Posterior Interosseus Syndrome [21] [22][23]
- Pain
- Weakness involving wrist extension and finger extension
- Motor deficits
- Elbow osteoarthritis
- Pain
- Loss of range of motion
- Fractures
- Distal Radial Fractures
- Radial Head Fracture
- Olecranon Fracture
- Cervical Radiculopathy
- Radiating arm pain corresponding to the dermatomes
- Neck pain
- Parasthesia
- Muscle weakness in myotome
- Reflex impairment/loss
- Headaches
- Scapular pain
- Sensory and motor dysfunction in upper extremities and neck
- Cervical Disc Disease
- Cervical Myofascial Pain
- Cervical Spondylosis
- Fibromyalgia
- Medial Epicondylitis
Diagnostic Procedures[edit | edit source]
The diagnose starts with asking about the activity level , occupation risk factors, recreational sports participation, medication and other medical problems. During the physical exam, the medicine will feel the structure of the elbow and other joints. Also the nerves, muscles, bones and skin are examined. It’s important to know which activities cause symptoms and where on your arm the symptoms occur.[1]
Investigations
Investigations are usually not performed in the straightforward case of lateral elbow pain. However, in longstanding cases, plain X-ray (AP and lateral views) of the elbow may show osteochondritis dissecans, degenerative joint changes or evidence of heterotopic calcification.
Ultrasound examination may prove to be a useful diagnostic tool in the investigation of patients with lateral elbow pain. Ultrasound may demonstrate the degree of tendon damage as well as the presence of a bursa. [19]
- X-rays: These may be taken to rule out arthritis of the elbow. 16% calcification along lateral epicondyle[19]
- Magnetic Resonance Imaging (MRI): if the symptoms are related to a neck problem, an MRI scan may be ordered. This will show if there is a possible herniated disk or arthritis in your neck. Both of these conditions often produce arm pain. MRI- 100% thickening[19]
- Electromyography (EMG): An EMG is used to rule out nerve compression. Many nerves travel around the elbow, and the symptoms of nerve compression are similar to those of tennis elbow.
Outcome Measures[edit | edit source]
- Pain reported outcome measures;
- Numeric Pain Rating Scale (NPRS)
- Visual Analogue Scale (VAS)
- Self-reported Questionnaires;
- The Upper Limb Functional Index (ULFI):
- Patient Rated Tennis Elbow Evaluation (PRTEE):
- QuickDASH (Disabilities of the Arm Shoulder and Hand):
- Patient Specific Functional Scale (PSFS) - although the PSFS has not yet been validated for lateral epicondylalgia, it has been shown to be valid, reliable and responsive to change in other conditions such as knee dysfunction, cervical radiculopathy, acute low back pain, mechanical low back pain, and neck dysfunction (Pain ICC = 0.89-0.99, Function ICC = 0.83-0.99, Total ICC = 0.89-0.99)[24][25][26]
Examination[edit | edit source]
The diagnosis of lateral epicondylitis is substantiated by tenderness over the ECRB or common extensor origin. By the following methods, the therapist or physiotherapist should be able to reproduce the typical pain:
- To examine the severity of the tennis elbow, there is a dynamometer and a Patient-rated Tennis Elbow Evaluation Questionnaire (PrTEEQ).[27] [28] The dynamometer measures grip strength. [29][30] The PrTEEQ is a 15-item questionnaire, it’s designed to measure forearm pain and disability in patients with lateral epicondylitis. The patients have to rate their levels of tennis elbow pain and disability from 0 to 10, and consists of 2 subscales. There is the pain subscale (0 = no pain, 10 = worst imaginable) en the function subscale (0 = no difficulty, 10 = unable to do).
- Cozen’s test: Cozen’s test is also known as the resisted wrist extension test. The elbow is stabilized in 90° flexion. The therapist palpates the lateral epicondyle and the other hand positions the patient’s hand into radial deviation and forarm pronation. Then the patient is asked to resist wrist extension. The test is positive if the patient experiences a sharp, sudden, severe pain over the lateral epicondyle.[31] [32][[33]
- Chair test: The patient grasps the back of the chair while standing behind it and attempts to lift the chair by using a three finger pinch (thumb, index long fingers) and the elbow fully extended. The test is positive when pain occurs at the lateral epicondyle. [33]
- Mill's Test: The patient is seated with the upper extremity relaxed at side and the elbow extended. The examiner passively stretches the wrist in flexion and pronation. Pain at the lateral epicondyle or proximal musculotendinous junction of wrist extensors is positive for lateral epicondylitis. [33][34] [3]
- Maudsley’s test: The examiner resist extension of the third digit of the hand, while palpating the lateral epicondyle. A positive test is indicated by pain over the lateral epicondyle.[3][34]
- The coffee cup test (by Coonrad and Hooper): While doing a specific activity such as picking up a full cup of coffee or a milk bottle. The patient is asked to rate their pain on a scale of zero to ten.[3][34]
Medical Management[edit | edit source]
Non-Operative Treatment[1][4][edit | edit source]
Non-Operative medical management of lateral epicondylitis is initially based on the following principles: relieving pain and controlling inflammation. Relieving pain can be countered by rest and avoiding painful activities. Inflammation on the other hand can be prevented by NSAIDs in the acute cases. The use of ice three times per day for 15 minutes is also recommended because it reduces the inflammatory response by decreasing the level of chemical activity and by vasoconstriction, which reduces the swelling. Elevation of the extremity is also indicated if an oedema of the wrist or fingers is present.[4]
The use of an elbow counterforce brace can be helpful because it plays the role of a secondary muscle attachment site and relieves tension on the insertion at the lateral epicondyle. The brace is applied around the forearm (below the head of the radius) and is tightened enough so that, when the patient contracts the wrist extensors, he or she does not fully contract the muscles.[1]
Injections should be given subperiosteally to the extensor brevis origin. These injections have an early and beneficial effect. During the initial 24-28 hours, increased pain be experienced. A steroid injection should be followed by 1-2 weeks’ rest and should not be repeated more than 2 times. Steroid injection seems to be effective for about 3 months, indicating that the patient must continue with the exercise program.[4]
Surgical treatment [1][11][edit | edit source]
If the symptoms of epicondylitis lateralis will prove to be resistant surgical treatment is indicated. Usually this is after a failed conservative treatment for more than 6 months.
Most surgical procedures for tennis elbow involve removing diseased muscle and reattaching healthy muscle back to bone. The right surgical approach for you will depend on a range of factors. These include the scope of your injury, your general health, and your personal needs.
Open surgery.[1][11] The most common approach to tennis elbow repair is open surgery. This involves making an incision over the elbow. Open surgery is usually performed as an outpatient surgery. It rarely requires an overnight stay at the hospital.
Arthroscopic surgery.[1] [11] Tennis elbow can also be repaired using tiny instruments and small incisions. Like open surgery, this is a same-day or outpatient procedure.
Physiotherapy Management[edit | edit source]
There are different types of therapies to treat lateral epicondylitis, all with the same aim: reduce pain and improve function. General physiotherapy management includes: [19]
- Education/Advice- on pain control and/or modification of activities
- Manual therapy- Mulligan - Mobilisation with movement
- Exercises- Strengthening and Stretching
- Modalities- Ultrasound, Transcutaneous electrical nerve stimulation (TENS)
- Braces/Splints/Straps- No clear evidence
- Medications- NSAIDs offer a short term benefit (3-4 weeks pain relief)
- Corticosteroids injection- Short term effect (<6 weeks)
- Sport/Occupation Specific Rehabilitation
Evidence for Physiotherapy[edit | edit source]
The study of Nagrale et al. demonstrate that Cyriax physiotherapy is a better treatment compared to phonophoresis and exercise for treating lateral epicondylalgia. The cyriax physiotherapy group had significantly better scores for all measurements at follow up (p<0.05). [35] Rajadurai et al demonstrate that supervised exercise program may be the first treatment in managing tennis elbow in comparison to Cyriax physiotherapy. Much more studies should be done to prove the evidence of using manual treatment like Cyriax physiotherapy)[36]
Physical therapy interventions including elbow joint mobilization with movement combined with exercise has been shown to have better results than"Therapeutic Corticosteroid Injection" at 6 weeks and to wait and see at 6 weeks but not 52 weeks. Recent research regarding cervicothoracic joint mobilization in conjunction with local treatment for lateral epicondylalgia has shown improvements in strength, pain, and tolerance to activity compared to local treatment alone. [37]
Corticosteroid injections have a short-term beneficial effect on lateral epicondylitis, but a negative effect in the intermediate term. Evidence on the long-term effect is conflicting. Manipulation and exercise and exercise and stretching have a short-term effect, with the latter also having a long-term effect.[1]
Physical therapy management including only the use of "Therapeutic Ultrasound for Lateral Epicondylitis', massage, and exercise has been shown to be no better than a "wait and see" treatment method.[38] Activity modification, when possible, can help prevent recurrent episodes of lateral epicondylalgia, as well as use of a counterforce brace as needed.
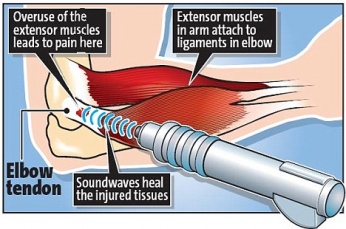
Extracorporeal Shockwave therapy
Shockwave Therapy is a method of treatment for multiple tendonopathies that can be used for the treatment of lateral epicondylitis. ESTW is a treatment technique in which patients are exposed to a strong mechanical wave impulses which can be used on a fairly accurate position. here are several studies[39][40][41][42][43] that examine the effects of extracorporeal shockwave on lateral epicondylitis. Statistical analysis of visual analogue scale (VAS), disabilities of the arm, shoulder, and hand (DASH) questionnaire and pain-free grip strength test scores has shown, both after treatment and to the follow-up at 6 months, significant difference comparing study group versus control group (P <0.001) [44] .The use of RSWT allowed a decrease of pain, and functional impairment, and an increase of the pain-free grip strength test, in patients with tennis elbow.[5]
Although the technique is widely reported to be safe, there is a potential for haemorrhage and local soft tissue damage through cavitation and this appears to be more likely with high doses. Studies has shown that Extracorporeal shockwave therapy offers a significant placebo effect with a moderate dos of ESWT in subjects with lateral epicondylitis. However there is no evidence of added benefit of treatment when compared to sham (placebo) therapy. This may be the reason why there are significant improvements noted by other studies.[39] [40][41][42][43]
Cyriax Physiotherapy [45][46][47][48]
It’s a very common intervention that combines the use of deep transverse friction (DTF) with Mill’s manipulations, which was used with success by Cyriax and Cyriax for treating lateral epicondylitis. Both the treatment components mentioned above must be used jointly in the sequence specified. Patient must follow the protocol three times a week for four weeks.[45]
There are several contraindications regard to this therapy: active infections, bursitis, disorders of the nerve structures, ossification and calcification of the soft tissues, active rheumatoid arthritis, anticoagulant.
Rajadurai et al demonstrate that supervised exercise program may be the first treatment in managing tennis elbow in comparison to Cyriax physiotherapy. Much more studies should be done to prove the evidence of using manual treatment like Cyriax physiotherapy. [45]
Deep Transverse Frictions
Deep transverse friction is a specific type of connective tissue massage applied precisely to the soft tissue structures. The therapist must try to reach an analgesic effect applying the DTF at the point of the lesion for 10 min till a numbing effect has been reached, that all for preparing the tendon for Mill’s manipulations. Pain during the friction massage is considered as a wrong indication. An interval of 48 hours between two sessions is necessary. (Comparison of effectiveness of supervised exercise… )[45]
The purpose of the deep friction massage is to maintain the mobility within the soft tissue structures. [49] It seems to have a pain relief function, due to modulation of the nociceptive impulses (gate control theory), a better alignment of connective tissue fibrils, softens the scar tissue, and blood flow increases, but further studies are needed.
The patient should be positioned with arm fully supinated in 90° of elbow flexion, identify the area of tenderness on the lateral epicondyle and apply pressure (DTF), with the tip of the thumb on the lateral epicondyle, in a posterior direction on the teno-osseous junction. The other hand stabilized the patient’s wrist.[45]
Mills Radial Head Manipulation video provided by Clinically Relevant
Mill's manipulation is the most common technique used by physiotherapists and is a small-amplitude high-velocity thrust performed at the end of elbow extension while the wrist and hand are held flexed.[50] the aim of this technique is to elongate the scar tissue by rupturing adhesions within the teno-oseous junction, making the area mobile and pain free. It’s used to imitate the mechanism of spontaneous recovery. [50]
Mill’s intention was to shift the annular ligament and replace it. Cyriax found out that the annular ligament applies the greatest possible stretching tension to the extensor carpi radialis muscles, that’s why the manipulative procedure should be carried out with a sharp jerk, in order to open the tear in the tendon and relieve tension on the tendon scar by converting a tear.[50]
This manipulation must only be performed if a fully pain-free elbow extension can be achieved, and with a properly technique. To prevent symptoms worsening, full wrist flexion must be achieved during the procedure. [50]
Patient seated with the affected extremity in 90° abduction and internal rotation (olecranon faced up).Therapist stands behind the patient , stabilized the patient’s wrist in full pronation and flexion, while the other hand is placed on the olecranon. The maintenance of full wrist flexion is important as failure to maintain this position could lead to a majority of the thrusting force being bome by the humeroulnar joint. The high-velocity low amplitude (HVLA) thrust at the end range of elbow extension, is a quick movement in the direction illustrated.[51]
This manipulation may produce mild discomfort at the instant of its performance.
The clinician applies this procedure a 2-3 times a week until cure, with a range of 4-12 sessions.[51]
Exercise therapy
Exercise therapy is a regimen or plan of physical activities designed and prescribed for specific therapeutic goals. Its purpose is to restore normal musculoskeletal function or to reduce pain caused by diseases or injuries.
Strength, stamina and mobility should be improved by exercises once the pain and inflammation are under control. [45][51]
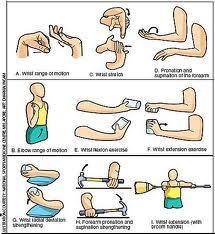
Stretching
The literature on the treatment of a Lateral Epicondylitis suggests that strengthening and stretching exercises are the most important components of exercise programmes, for the reason that tendons should not only be strong but also flexible. The stretching exercises are intended to improve the flexibility of the extensor group of the wrist. These exercises ought to be instituted and continued until the range of motion of the wrist is the same as that of the uninvolved side
The underlying principle of the stretching phase is that , by lengthening the tendon during relaxation, we can reduce its stretching during offending movements. The best stretching position for the Extensor Carpi Radialis Brevis tendon, is reached with the elbow in extension, forearm in pronation, wrist in flexion and with ulnar deviation of the wrist, according to the patient’s tolerance. This stretching should be held for 30- 45 s and 3 times before and after the eccentric exercises, during each treatment session with a 30 s rest interval.
Other programs says that stretching exercises for the extensor muscles of the wrist and fingers should be performed in the following manner: fully extend the elbow and palmary flex the wrist. Remain in the point of maximum non painful extension for a period of 15 to 25s. this exercises is repeated four to five times a day with two series of ten exercises in each session: the patient should always stop at the first sign of pain. In this phase of therapy, the patient should also perform isotonic exercises, once a day, according to the following plan:[45]
1. Stretching exercises = repeat 10 times (15-25 seconds)
2. Isotonic exercises = repeat 15 times (3 series)
3. Stretching exercises = repeat 10 times (15-25 seconds)
4. Icing = massage the tender area with ice or crushed ice for 10-15 minutes
Eccentric exercises
There are three principles of eccentric exercises. These are load ( resistance), speed (velocity) and frequency of contractions.[52]
- Load ( resistance): Increasing the load ensures the tendon is subjected to greater stress and forms the fundamental basis of the progression of the exercise programme. The basis of all physical training programmes is formed by this principle of progressive overloading. According to the patient’s symptoms, it is important that the load of these eccentric exercises should be increased. If it’s not increased then the possibility of re-injury will be high.
- Speed ( velocity): The speed (velocity) of contractions is also a fundamental principle of successful eccentric exercises. In each treatment session the speed of the eccentric training should be increased. Hence the load on the tendon increases to stimulate the mechanism of the injury. However the therapists must ensure that the patients perform the eccentric exercises slowly to avoid pain.
- Frequency of contractions: The frequency of contractions is the third principle of eccentric exercises. There can be variations of sets and repetitions in the literature. According to the therapists 3 sets of 10 repetitions can normally be performed without overloading the injured tendon, as determined by the tolerance of the patient. The elbow is in full extension, forearm in pronation and the arm is supported. The greatest strengthening result for the extensor tendons of the wrist is reached in this position. This is a recommendation and the frequency must be patient specific.[52]
Theraband Exercise:
Theraband exercises (or exercises with a small weight) are performed each day for 3 sets of 10. You fix one side of the theraband under you feet or another place and you take the other side in your hand or you have a small weight in your hand.
The patient starts the exercise in wrist flexion, then he/she does a wrist extension and comes back to the start position very slowly. [13] This exercise is an concentric en eccentric exercise for the wrist extensors. They concluded that supervised exercise consisting of static stretching and eccentric strengthening produced the largest effect in reducing pain, strenght and improving function. Once the patients can do this, they can progress to another colour of theraband or you increase the weight. [13]
In this study the subjects were assigned to group A or group B. Group A received supervised therapeutic exercise program which included static stretching of the Extensor Carpi Radialis Brevis followed by eccentric strengthening of the wrist extensors. Group B was treated with Cyriax physiotherapy. The groups that performed supervised exercise program (group A) for 4 weeks showed significantly greater improvement in reduction of pain and functional status than the Cyriax physiotherapy treatment.[13]

Flexbar® Exercises [54]
The Flexbar® is an effective and beneficial eccentric exercise for patients with lateral epicondylitis. This resistance device is easy to use at home and is an excellent example of true “evidence-based practice” in physical therapy. Instructions for the 5 Steps of the Exercise:
- Hold FlexBar® in the affected (right) hand. Make sure it's in full wrist extension..
- The other end of the device must be held with your unaffected (left) hand.
- Twist FlexBar® with unaffected wrist while holding.
The FlexBar® exercise is performed each day for 3 sets of 15. It takes 4 seconds to complete each repetition and between each set of 15 repetitions there is 30 seconds of rest. Once the patients can perform 3 sets of 15, they progress to another colour FlexBar® with a higher intensity of eccentric resistance.The treatment continued until the patient had a resolution of symptoms, which occurred at an average of 7 weeks of treatment with 10 clinic visits. The treatment should be continued until this resolution occurs. The treatment should be continued until this resolution occurs.
Clinical Bottom Line[edit | edit source]
Lateral epicondylitis is the most common overuse syndrome in the elbow. It is an injury involving the extensor muscles of the forearm. In a lot of cases, the insertion of the extensor carpi radialis brevis is involved. Contractile overloads that chronically tension or stress the tendon near the attachment on the humerus are the primary cause of epicondylitis. It occurs often in repetitive upper extremity activities such as computer use, heavy lifting, forceful forearm pronation and supination, and repetitive vibration. Medical management consist of NSAID, ice, elevation and the use of an elbow counterforce brace. If the symptoms will prove to be resistant surgical treatment is indicated. Concerning physical management there are different types of therapies to treat lateral epicondylitis. The most important methods are: Cyriax therapy, stretching and exercises with the Flexbar.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Alexander J. Chien et All. Sonography and MR Imaging of Posterior Interosseous Nerve Syndrome with Surgical Correlation. The American Journal of Roentgenology, number 1, volume 181, July 2003, p219-221. Level of Evidence: 2C
- ↑ D. M. Walz, J. S. Newman, G. P. Konin, and G. Ross, Epicondylitis: Pathogenesis, Imaging, and Treatment, RadioGraphics, January 1, 2010; 30(1): 167 - 184. Level of Evidence: 2C
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Tuomo Pienimäki, M.D Ph.D et al. Associations Between Pain, Grip Strength, and Manual Tests in the Treatment Evaluation of Chronic Tennis Elbow . The clinical journal of pain 18: 164-170 2002. Level of Evidence: 3B.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Whaley AL, Baker CL. Lateral epicondylitis. Clin Sports Med 2004;23:677– 691. Level of Evidence: 1C.
- ↑ 5.0 5.1 Phil Page., a new exercise for tennis elbow that works, N Am J Sports Phys Ther. 2010 Sep; 5(3): 189–193. Level of Evidence: 1A.
- ↑ 6.0 6.1 D. M. Walz, J. S. Newman, G. P. Konin, and G. Ross, Epicondylitis: Pathogenesis, Imaging, and Treatment, RadioGraphics, January 1, 2010; 30(1): 167 - 184. Level of Evidence: 2C
- ↑ D. Stasinopoulos et al, Cyriax physiotherapy for tennis elbow/lateral epicondylitis, 2004, British Journal of Sports Medicine. Level of Evidence: 1B.
- ↑ Nirschl RP. Tennis elbow. Orthop North Am. 1973;4:787-99.
- ↑ 9.0 9.1 Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). May 2009;48(5):528-36. A1 http://rheumatology.oxfordjournals.org/content/48/5/528.full.pdf (accessed 17 Nov 2010)
- ↑ Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders at the elbow: a systematic literature review. Rheumatology (Oxford). May 2009;48(5):528-36. A1http://rheumatology.oxfordjournals.org/content/48/5/528.full.pdf (accessed 17 Nov 2010)
- ↑ 11.0 11.1 11.2 11.3 Baker CL, Plancher KD. Operative treatment of elbow injuries. New York: Springer, 2002.
- ↑ Davenport TE, Kulig K, Matharu Y, Blanco CE. The EdUReP Model for Nonsurgical Management of Tendinopathy. Phys Ther. 2005;85(10):1093-103. http://ptjournal.apta.org/content/85/10/1093.long
- ↑ 13.0 13.1 13.2 13.3 13.4 Warren, RF. Tennis elbow (epicondylitis): epidemiology and conservative treatment, in AAOS Symposium and Upper Extremity Injuries in Athletes, Pettrone, F.A., Ed. St. Louis: C.V. Mosby, 1986; 233-243. Level of Evidence: 1B
- ↑ Richard B. Birrer et al., Sport Medicine for the Primary Care Physician, 2002. Level of evidence 5
- ↑ Wright JG. Evidence-based orthopaedics: the best answers to clinical questions. Philadelphia: Saunders Elsevier, 2008.
- ↑ Cyriax JH. The pathology and treatment of tennis elbow. J Bone Joint Surg 1936; 18: 921–
- ↑ Smidt N, van der Windt D, Assendelft W, Devillé W, Korthals-de Bos I, Bouter L. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. Lancet 2002; 359: 657–62. A2 http://www.physio-pedia.com/images/9/9e/Smidt_et_al_RCT_lateral_elbow.pdf (accessed 30 Dec 2010)
- ↑ 18.0 18.1 Nirschl RP, Ashman ES. Elbow tendinopathy: tennis elbow. Clinics in sports medicine. 2003 Oct 1;22(4):813-36.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.
- ↑ Roles NC, Maudsley RH. Radial tunnel syndrome: Resistant tennis elbow as nerve entrapment. J Bone Joint Surg Br 54:499-508, 1972.http://web.jbjs.org.uk/cgi/reprint/54-B/3/499 (accessed 20 Nov 2010)
- ↑ Portilla Molina et All. The posterior interosseous nerve and the radial tunnel syndrome: an antatomical study. International Orthopaedics, number 2, volume 22, p102-106. Level of Evidence: 1B
- ↑ Alexander J. Chien et All. Sonography and MR Imaging of Posterior Interosseous Nerve Syndrome with Surgical Correlation. The American Journal of Roentgenology, number 1, volume 181, July 2003, p219-221. Level of Evidence: 2C
- ↑ Bionka M. et All. Interventions for treating the posterior interosseus nerve syndrome: a systematic review of observational studies. Journal of the Peripheral Nervous System, number 2, volume 11, 15 JUNE 2006, p101-110. Level of Evidence: 3A
- ↑ Leung HB, Yen CH, Tse PYT. Reliability of Hong Kong Chinese version of the Patient ratedfckLRForearm Evaluation Questionnaire for lateral epicondylitis. Hong Kong Med J 2004;10:172-7.
- ↑ Newcomer KL, Martinez-Silvestrini JA, Schaefer MP, Gay RE, Arendt KW. Sensitivity of the Patient-rated Forearm Evaluation Questionnaire in lateral epicondylitis. J Hand Ther 2005;18:400-6.
- ↑ Overend TJ, Wuori-Fearn JL, Kramer JF, MacDermid JC. Reliability of a patient-rated forearm evaluation questionnaire for patients with lateral epicondylitis. J Hand Ther 1999;12:31-7.
- ↑ Rompe JD, Overend TJ, MacDermid JC. Validation of the Patient-rated Tennis Elbow Evaluation Questionnaire. J Hand Ther. 2007 Jan-Mar;20(1):3-10. http://www.ncbi.nlm.nih.gov/pubmed/17254903 (accessed 30 Dec 2010)
- ↑ MacDermid JC. The Patient-Rated Tennis Elbow Evaluation (PRTEE)© User Manual. 2007 http://www.srs-mcmaster.ca/Portals/20/pdf/research_resources/PRTE_UserManual_Dec2007.pdf (accessed 30 Dec 2010)
- ↑ Mathiowetz V. Comparison of Rolyan and Jamar dynamometers for measuring grip strength. Occup Ther Int. 2002;9(3):201-9.
- ↑ http://www.fysio-web.nl/Handheld_Dynamometer_1_2_11_jun.pdf (accessed 30 Dec 2010)
- ↑ ooper G. Pocket guide to musculoskeletal diagnosis. New Jersey: Humana Press, 2006
- ↑ Bhargava AS, Eapen C, Kumar SP. Grip strength measurements at two different wrist extension positions in chronic lateral epicondylitis-comparison of involved vs. uninvolved side in athletes and non athletes: a case-control study. Sports Med Arthrosc Rehabil Ther Technol. 2010 Sep 7;2:22.
- ↑ 33.0 33.1 33.2 Frydrychowicz A, Lubner MG, Brown JJ, Merkle EM, Nagle SK, Rofsky NM, Reeder SB (2012). "Hepatobiliary MR imaging with gadolinium-based contrast agents". J Magn Reson Imaging 35 (3): 492–511. Level of Evidence: 5
- ↑ 34.0 34.1 34.2 aldes K, LaStayo P. The value of provocative tests for the wrist and elbow: a literature review. Journal of Hand Therapy, 2013; 26: 32-43. Level of Evidence: 1A
- ↑ mit V. Nagrale; Christ opher R. Herd; Shyam Ganvir; Gopichand Ramteke,Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical Trial, J Man Manip Ther. 2009; 17(3): 171-178 Level of evidence:1B
- ↑ Rajadurai Viswas, Rejeeshkumar Ramachandran, and Payal Korde Anantkumar, “Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow Lateral Epicondylitis): A Randomized Clinical Trial”, The ScientificWorld Journal Volume 2012, Article ID 939645, 8 pages doi:10.1100/2012/939645 Level of evidence: 1B
- ↑ Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: a pilot clinical trial. J Man and Manip Ther. 2005;13(3):143-151.
- ↑ Smidt N, Van der Windt DAWM, Assendelft WJJ, Deville WLFM, Korthals-de Bos IBC, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomised controlled trial. LANCET. 2002;359:657-662.
- ↑ 39.0 39.1 Hammer DS, Rupp S, Ensslin S, Kohn D, Seil R. Extracorporal shock wave therapy in patients with tennis elbow and painful heel. Archives of orthopaedic and trauma surgery. 2000 Apr 8;120(5):304-7.
- ↑ 40.0 40.1 Crowther MA, Bannister GC, Huma H, Rooker GD. A prospective, randomised study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow. Bone & Joint Journal. 2002 Jul 1;84(5):678-9.
- ↑ 41.0 41.1 Rompe JD, Hopf C, Küllmer K, Heine J, Bürger R, Nafe B. Low-energy extracorporal shock wave therapy for persistent tennis elbow. International orthopaedics. 1996 Feb 1;20(1):23-7.
- ↑ 42.0 42.1 Krischek O, Hopf C, Nafe B, Rompe JD. Shock-wave therapy for tennis and golfer’s elbow–1 year follow-up. Archives of orthopaedic and trauma surgery. 1999 Feb 8;119(1):62-6.
- ↑ 43.0 43.1 Stasinopoulos, D. and Johnson, M.I., 2005. Effectiveness of extracorporeal shock wave therapy for tennis elbow (lateral epicondylitis). British journal of sports medicine, 39(3), pp.132-136.
- ↑ Phil Page., a new exercise for tennis elbow that works, N Am J Sports Phys Ther. 2010 Sep; 5(3): 189–193. Level of Evidence: 1A.
- ↑ 45.0 45.1 45.2 45.3 45.4 45.5 45.6 Viswas R., et al. Comparison of Effectiveness of Supervised Exercise Program and Cyriax Physiotherapy in Patients with Tennis Elbow (Lateral Epicondylitis): A Randomized Clinical Trial, 2012, Scientific World Journal. Level of Evidence: 1B
- ↑ Warren, RF. Tennis elbow (epicondylitis): epidemiology and conservative treatment, in AAOS Symposium and Upper Extremity Injuries in Athletes, Pettrone, F.A., Ed. St. Louis: C.V. Mosby, 1986; 233-243. Level of Evidence: 1B
- ↑ Kochar M, Dogra A. Effectiveness of a specific physiotherapy regimen on patients with tennis elbow: clinical study. Physiotherapy, 2002; 88: 333–341. Level of Evidence: 1A
- ↑ James Walrod, MD, Craig C Young et al. Lateral epicondilitis; Medscape ; 2015. Level of Evidence: 1A.
- ↑ GAIL J. CHAMBERLAIN, MA, PT*, Cyriax's Friction Massage: A Review, 0196-601 1 /82/0401-0016$02.00/0 THE JOURNAL OF ORTHOPAEDIC AND SPORTSP HYSICALT HERAPY Copyright O 1982 by The Orthopaedic and Sports Physical Therapy Sections of the American Physical Therapy Association Level of evidence:2 A
- ↑ 50.0 50.1 50.2 50.3 Bill Vicenzino, PT, PhD, Joshua A. Cleland, PT, PhD, OCS, FAAOMPT, and Leanne Bisset, PT, MPhty (Sports), Joint Manipulation in the Management of Lateral Epicondylalgia: A Clinical Commentary, J Man Manip Ther. 2007; 15(1): 50–56 Level of evidende:2A
- ↑ 51.0 51.1 51.2 V. Nagrale; Christ opher R. Herd; Shyam Ganvir; Gopichand Ramteke,Cyriax Physiotherapy Versus Phonophoresis with Supervised Exercise in Subjects with LateralEpicondylalgia: A Randomized Clinical Trial, J Man Manip Ther. 2009; 17(3): 171-178 Level of evidence:1B
- ↑ 52.0 52.1 Stanish WD, Rubinovich RM, Curwin S. Eccentric exercise in chronic tendinitis. Clinical orthopaedics and related research. 1986 Jul 1;208:65-8.
- ↑ https://goo.gl/images/dG2t3E
- ↑ Phil Page, et al, A new exercise for tennis elbow that works, 2010, North American Journal of Sports Physical Therapy. (Level of Evidence 2C)