Kidney
Original Editor - Manisha Shrestha
Top Contributors - Manisha Shrestha and Lucinda hampton
Introduction[edit | edit source]
There are two kidneys present in the human body. Kidneys are bean-shaped, approximately fist-size internal organs located on either side of the spine in the retroperitoneal space between the parietal peritoneum and the posterior abdominal wall, well protected by muscle, fat, and ribs. The kidneys are well vascularized, receiving about 25 percent of the cardiac output at rest. The main function of the kidney is to excrete a variety of waste products produced by metabolism into the urine.
Gross Anatomy of Kidney[edit | edit source]
External Anatomy[edit | edit source]
- The left kidney is located at about the T12 to L3 vertebrae, whereas the right is lower due to slight displacement by the liver. The upper portions of the kidneys are somewhat protected by the eleventh and twelfth ribs.
- The right kidney sits just below the diaphragm and posterior to the liver. The left kidney sits below the diaphragm and posterior to the spleen.
- Each kidney weighs about 125–175 g in males and 115–155 g in females. They are about 11–14 cm in length, 6 cm wide, and 4 cm thick, and are directly covered by a fibrous capsule composed of dense, irregular connective tissue that helps to hold their shape and protect them.
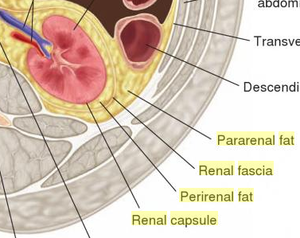
- Each kidney, with its adrenal gland on top is surrounded by shock-absorbing two layers of fat: the perirenal fat present between renal fascia and renal capsule and pararenal fat superior to the renal fascia.
- The renal fascia and, to a lesser extent, the overlying peritoneum serves to firmly anchor the kidneys to the posterior abdominal wall in a retroperitoneal position.
- So basically, the external layers of the kidney are a renal capsule in close proximity followed by perirenal fat pad, renal fascia, and then pararenal fat pad.
Internal Anatomy[edit | edit source]
- A frontal section through the kidney reveals division of renal parenchyma into an outer region called the renal cortex and an inner region called the medulla.
- Grossly, these structures take the shape of eight to 18 cone-shaped renal lobes, each containing renal cortex surrounding a portion of medulla called a renal pyramid. The pyramids and renal columns taken together constitute the kidney lobes.
- The renal columns are connective tissue extensions that radiate downward from the cortex through the medulla to separate the most characteristic features of the medulla, the renal pyramids and renal papillae.
- The papillae are bundles of collecting ducts that transport urine made by nephrons to the calyces of the kidney for excretion.
- The renal columns also serve to divide the kidney into lobes and provide a supportive framework for vessels that enter and exit the cortex.
- The papilla of each pyramid empties urine into a minor calyx; minor calyces empty into major calyces, and major calyces empty into the renal pelvis and thus become a ureter.
- At the hilum, the ureter and renal vein exits whereas renal artery and renal nerve enter.
Microscopic Anatomy of Kidney[edit | edit source]
Nephrons are the structural and functional unit of renal system. Each human adult kidney contains around 1 million nephrons. The microscopic structure of kidney consist of two main parts: Nephrons and Collecting ducts. Nephron is divided into two parts; renal corpuscles (Glomerulus and Bowman's capsule) and tubules (Proximal convoluted tubules, Loop of Henle and Distal convoluted tubules.
Renal corpuscle[edit | edit source]
The renal corpuscle consists of a tuft of capillaries called the glomerulus that is largely surrounded by Bowman’s (glomerular) capsule. The glomerulus is a high-pressure capillary bed between afferent and efferent arterioles. Bowman’s capsule surrounds the glomerulus to form a lumen, and captures and directs this filtrate to the PCT. The outermost part of Bowman’s capsule, the parietal layer, is a simple squamous epithelium. It transitions onto the glomerular capillaries in an intimate embrace to form the visceral layer of the capsule. Here, the cells are not squamous, but uniquely shaped cells (podocytes) extending finger-like arms (pedicels) to cover the glomerular capillaries. These projections interdigitate to form filtration slits, leaving small gaps between the digits to form a sieve. As blood passes through the glomerulus, 10 to 20 percent of the plasma filters between these sieve-like fingers to be captured by Bowman’s capsule and funneled to the PCT. Where the fenestrae (windows) in the glomerular capillaries match the spaces between the podocyte “fingers,” the only thing separating the capillary lumen and the lumen of Bowman’s capsule is their shared basement membrane. These three features comprise what is known as the filtration membrane. This membrane permits very rapid movement of filtrate from capillary to capsule though pores that are only 70 nm in diameter.
A second cell type in this apparatus is the juxtaglomerular cell. This is a modified, smooth muscle cell lining the afferent arteriole that can contract or relax in response to ATP or adenosine released by the macula densa. Such contraction and relaxation regulate blood flow to the glomerulus. If the osmolarity of the filtrate is too high (hyperosmotic), the juxtaglomerular cells will contract, decreasing the glomerular filtration rate (GFR) so less plasma is filtered, leading to less urine formation and greater retention of fluid. This will ultimately decrease blood osmolarity toward the physiologic norm. A second function of the macula densa cells is to regulate renin release from the juxtaglomerular cells of the afferent arteriole. Active renin is a protein comprised of 304 amino acids that cleaves several amino acids from angiotensinogen to produce angiotensin I. Angiotensin I is not biologically active until converted to angiotensin II by angiotensin-converting enzyme (ACE) from the lungs. Angiotensin II is a systemic vasoconstrictor that helps to regulate blood pressure by increasing it. Angiotensin II also stimulates the release of the steroid hormone aldosterone from the adrenal cortex. Aldosterone stimulates Na+ reabsorption by the kidney, which also results in water retention and increased blood pressure.
Proximal Convoluted Tubule (PCT)[edit | edit source]
Filtered fluid collected by Bowman’s capsule enters into the PCT. It is called convoluted due to its tortuous path. Simple cuboidal cells form this tubule with prominent microvilli on the luminal surface, forming a brush border. These microvilli create a large surface area to maximize the absorption and secretion of solutes (Na+, Cl–, glucose, etc.), the most essential function of this portion of the nephron. These cells actively transport ions across their membranes, so they possess a high concentration of mitochondria in order to produce sufficient ATP.
Loop of Henle[edit | edit source]
The descending and ascending portions of the loop of Henle (sometimes referred to as the nephron loop) are, of course, just continuations of the same tubule. They run adjacent and parallel to each other after having made a hairpin turn at the deepest point of their descent. The descending loop of Henle consists of an initial short, thick portion and long, thin portion, whereas the ascending loop consists of an initial short, thin portion followed by a long, thick portion. The descending thick portion consists of simple cuboidal epithelium similar to that of the PCT. The descending and ascending thin portions consists of simple squamous epithelium. As you will see later, these are important differences, since different portions of the loop have different permeabilities for solutes and water. The ascending thick portion consists of simple cuboidal epithelium similar to the DCT.
Distal Convoluted Tubule (DCT)[edit | edit source]
The DCT, like the PCT, is very tortuous and formed by simple cuboidal epithelium, but it is shorter than the PCT. These cells are not as active as those in the PCT; thus, there are fewer microvilli on the apical surface. However, these cells must also pump ions against their concentration gradient, so you will find of large numbers of mitochondria, although fewer than in the PCT.
Collecting Ducts[edit | edit source]
The collecting ducts are continuous with the nephron but not technically part of it. In fact, each duct collects filtrate from several nephrons for final modification. Collecting ducts merge as they descend deeper in the medulla to form about 30 terminal ducts, which empty at a papilla. They are lined with simple squamous epithelium with receptors for ADH. When stimulated by ADH, these cells will insert aquaporin channel proteins into their membranes, which as their name suggests, allow water to pass from the duct lumen through the cells and into the interstitial spaces to be recovered by the vasa recta. This process allows for the recovery of large amounts of water from the filtrate back into the blood. In the absence of ADH, these channels are not inserted, resulting in the excretion of water in the form of dilute urine. Most, if not all, cells of the body contain aquaporin molecules, whose channels are so small that only water can pass. At least 10 types of aquaporins are known in humans, and six of those are found in the kidney. The function of all aquaporins is to allow the movement of water across the lipid-rich, hydrophobic cell membrane.
Blood supply of Kidney[edit | edit source]
Arterial supply
- Renal artery in each side, are the direct branches of abdominal aorta and are large in size.
- Renal artery further divides into segmental arteries, then to interlobar arteries that communicate with one another via arcuate arteries.
- The arcuate arteries give off branches called interlobular arteries that extend into the cortex.
Venous Supply
- Venous return of the blood is via similarly named veins which then ends into inferior venacava. the left renal vein is longer than the right.
Lymphatic drainage
- Lymphatic drainage is into the lateral aortic nodes.
Nerve supply of kidney[edit | edit source]
- Kidney and nervous system communicates via renal plexus .
- Renal nerve arise from superior mesenteric ganglion and enter the hilum of each kidney and follow branches of renal artery to reach individual nephrons.
- These nerves consist mostly of sympathetic fibers that trigger vasoconstriction in kidney.
- Sensory input from the kidney travels to the T10 -11 levels of spinal cord and is sensed in the corresponding dermatome. thus, pain in the flank region may be referred from corresponding kidney.[4]
Function of Kidney[edit | edit source]
Primary Function
- It is a major excretory organ for elimination of metabolic wastes from the body.[5]
- The overall renal function of the system filters approximately 200 liters of fluid a day from renal blood flow which allows for toxins, metabolic waste products, and excess ion to be excreted while keeping essential substances in the blood.
- It regulates plasma osmolarity by modulating the amount of water, solutes, and electrolytes in the blood.
Secondary Function
- It ensures long term acid-base balance
- It also produces erythropoietin which stimulates the production of red blood cell.
- It also produces renin for blood pressure regulation
- It carries out the conversion of vitamin D to its active form, ultimately helps in calcium absorption.[6][7]
References[edit | edit source]
- ↑ Anatomic Wisdom. The External Gross Anatomy of the Kidney. Available from: https://www.youtube.com/watch?v=OmMzMBSsaU4. [Lasted accessed: 2021-4-30]
- ↑ Kidneys and Urinary System LO2 - Internal Gross Anatomy. Available from: https://www.youtube.com/watch?v=25CO_f7o_c4. [lasted accessed: 2021-4-30]
- ↑ Microscopic structure of kidney-Nephron. Available from: https://www.youtube.com/watch?v=OoIZ1N-haL8. [Lasted accessed: 2021-4-30]
- ↑ Kidney. From Wikipedia, the free encyclopedia Available from: https://en.wikipedia.org/wiki/Kidney. Lasted accessed: 2021-5-2
- ↑ Finco DR. Kidney function. In Clinical biochemistry of domestic animals 1997 Jan 1 (pp. 441-484). Academic Press.
- ↑ Ogobuiro I, Tuma F. Physiology, renal. StatPearls [Internet]. 2019 Feb 10.
- ↑ Microscopic Anatomy of the Kidney. Available from: https://bio.libretexts.org/Courses/Lumen_Learning/Book%3A_Biology_of_Aging_(Lumen)/13%3A_The_Urinary_System/13.05%3A_Microscopic_Anatomy_of_the_Kidney. Lasted Accessed: 2021-5-2