Introduction to Plantar Heel Pain
Original Editor - Merinda Rodseth based on a course by Bernice Saban
Top Contributors - Merinda Rodseth, Kim Jackson, Jess Bell, Ewa Jaraczewska and Tarina van der Stockt
Terminology[edit | edit source]
Many terms have been used to describe pain under the plantar aspect of the heel, including:[1][2][3]
- Gonorrhoeal heel
- Policeman’s heel
- Heel spur syndrome
- Calcaneal spur
- Fat pad syndrome
- Subcalcaneal pain
- Jogger’s heel
- Plantar fasciitis
- Plantar fasciopathy
- Plantar fasciosis
- Plantar heel pain
Many of the terms used to describe pain under the heel are related to specific pathologies, even when the actual underlying pathology of pain under the heel remains largely unknown.[1][4] Many clinicians have focused on the plantar fascia when presented with complaints of pain under the heel, but sufficient evidence now exists to indicate that the plantar fascia is not the only culprit.[1] Therefore, in order to facilitate effective communication between clinicians, improve patient’s understanding of their condition, encourage shared decision making and enhance treatment outcomes, consistent and unambiguous terminology is needed.[1] The term “plantar heel pain” was hence proposed to describe the condition of pain under the heel where no differential diagnosis exists.[1][3]
Anatomy and Function of the Heel[edit | edit source]
Anatomy[edit | edit source]
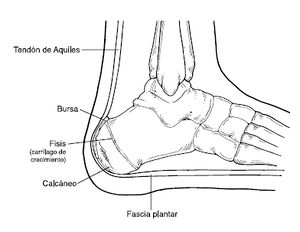
The calcaneal bone is the largest bone in the foot and specifically adapted to sustain high tensile, bending and compressive forces, especially during weight-bearing:[5][6]
- Numerous ligaments and muscles attach to the calcaneus and help with its role in human bipedal biomechanics [7]
- It articulates with the talus superiorly and the cuboid anteriorly and shares a joint space with the talocalcaneonavicular joint.
The posterior part of the calcaneus is circular, with three facets (superior, middle and inferior):
- The superior facet is separated from the calcaneal tendon by the retrocalcaneal bursa.
- The middle facet provides the attachment site for the calcaneal tendon (Achilles tendon).
- The inferior facet curves anteriorly and is continuous with calcaneal tuberosity on the plantar surface.
The plantar surface of the calcaneal tuberosity projects forward on the plantar surface as a medial (larger) and lateral (smaller) process and at its most anterior projection is the calcaneal tubercle, where the short plantar ligament attaches.[8]
On the lateral aspect of the calcaneus is the peroneal tubercle, anterior to the middle of the surface, where the tendons of the fibularis brevis and longus muscles pass above and below respectively.
Protruding anteromedially from upper margin of the medial surface is the sustentaculum tali which supports the more posterior part of the head of the talus.
At its inferior aspect is a groove accommodating the flexor hallucis longus tendon.
Superiorly is the middle talar articular facet for the corresponding middle facet of the head of talus as part of the subtalar joint.
The anterior and posterior facets of the talocalcaneal joint are on the superior surface of the calcaneus. The anterior facet is small and the posterior facet is large. Between these two facets runs a fairly deep sulcus, the calcaneal sulcus, which together with the opposing talar sulcus forms the tarsal sinus.
The anterior surface has a convex articular facet for the cuboid bone.[9]
Function[edit | edit source]
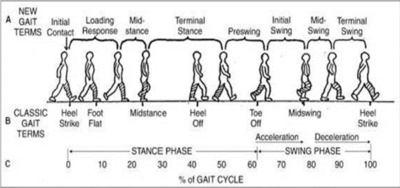
Weight-bearing is not equally distributed over the foot during stance but concentrated on the heel area. The inferior part of the calcaneus is roughened and covered by strong fibrous tissue, the fat of the heel pad and thick skin.[6] The lowest part of the posterior calcaneus transfers body weight from the heel to the ground during the heel-strike phase of walking.[6] The heel is very active in the gait cycle and takes weight for about 40% of the gait cycle - from heel strike to heel off.[10] The anteromedial aspect of the calcaneus also provides attachment to the plantar fascia, an important structure in the maintenance of the longitudinal arches of the foot.[6]
Prevalence of Plantar Heel Pain[edit | edit source]
Plantar heel pain (PHP) is one of the most common musculoskeletal conditions affecting the lower limb,[11] with an estimated prevalence of 3.6-9.6%. [4][11] It accounts for 11-15% of all foot complaints in adults seeking professional care.[12] It affects very active people with high training volumes, such as runners, as well as middle-aged to older sedentary individuals (40-60 years) with high body mass indexes.[1][12] PHP can be long-standing and it negatively impacts the quality of life. It is also associated with significant disability due to the pain complicating everyday and sports activities.[4][12]
Despite the significant personal disability, as well as the societal burden associated with this condition, the aetiology of PHP remains unclear.[2][11] PHP is associated with a range of foot-level factors such as:
- pronated foot type
- limited ankle joint dorsiflexion
- first metatarsophalangeal joint dorsiflexion
- reduced muscle strength in the foot and the ankle
As well as personal-level factors such as:
- high body mass index
- depression
- anxiety
- stress
- occupations requiring prolonged periods of standing[2][11]
These factors may not infer causation, but they support the view that PHP is a complex and multifactorial problem.[2][11] The complexity of PHP combined with the limited understanding of its aetiology leads to uncertainty regarding the most effective intervention strategies.[2]
Location of the Pain[edit | edit source]
Clinically, pain is the most common complaint in PHP, resulting in difficulty with weight-bearing activities such as walking and standing and negatively impacting occupational and recreational activities.[13] Pain under the heel is typically located on the anteromedial aspect of the plantar heel.[1] Clinicians commonly use thumb pressure when manually palpating the heel, in order to locate the exact site of pain and formulate a diagnosis.[13] Foot pressure has long been considered significant in the aetiology of PHP.[2]
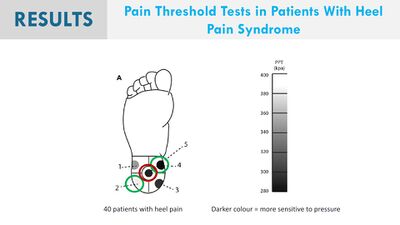
Saban and Masharawi [13] proposed the use of pressure pain thresholds (PPT) as a semi-objective method for quantifying the magnitude of mechanical pressure required to elicit pain.
- PPT is defined as “the minimal amount of pressure with which a sensation of pressure first changes to pain” [3] and easily tested with pressure algometry.[13]
- PPTs are generally higher in the normal weight-bearing parts of the foot, expressing a lower mechanical sensitivity. Thereby the heel has the highest PPT level of the plantar aspect of the foot, which is consistent with the loading pattern of the heel during gait.[3][13]
- To measure the PPT, Saban and Masharawi [13] had the patient lay supine with the feet over the edge of the bed and no pressure on the heel. The heel area was divided into 5 regions and PPT measurements were recorded at each of the sites using a hand-held computerised mechanical pressure algometer.
- In their study, Saban and Masharawi [13] found the anterior medial aspect of the heel to be the most sensitive area of the heel, consistent with the area commonly cited by patients, but it did not differentiate between individuals with PHP and controls.
Ríos-León et al [3] reported lower PPTs (higher pressure pain sensitivity) in the general plantar region of both feet in individuals with PHP. This pressure pain sensitivity was also associated with higher pain intensity at first step in the morning, as well as increased thickness of the plantar fascia at its origin, but not with disability or foot posture.[3] They reported a more generalised hyperalgesia on the affected foot in patients with PHP.[3]
Heel Pain[edit | edit source]
Presentation of pain[edit | edit source]
- Pain: usually burning, sharp, shooting, shock-like, electric, and occasionally described as a dull aching. Pain can be local or radiating proximally or distally. If the symptoms are caused by nerve entrapment, patients might experience night pain as a result of venostasis (slowing of venous outflow) and venous engorgement (local congestion an distension with blood).[15]
- Post-static dyskinesia: pain when a patient first stands after periods of rest. It is most commonly associated with nerve-related plantar heel pain. Patients report severe pain in the morning after rising from the bed. If the pain is due to neural compression it tends to ease with ambulation and movement. However, it tends to worsen if the pain is caused by plantar fasciitis.[15]
- Paraesthesiae and neurological changes such as numbness, sensory changes, pins and needles around the medial and plantar aspect of the heel.[15]
Behaviour of the Pain[edit | edit source]
Pain under the heel typically presents as pain on the anteromedial aspect of the plantar heel during weight-bearing. It is generally exacerbated by prolonged periods of walking and standing and can be particularly sharp when first stepping on the heel after long periods of rest (for example, first stepping out of bed in the morning, or getting up after long periods of sitting down).[1][3][16] This “first step pain” is also the most commonly described symptom in PHP.[4]
Additional Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, Landorf KB. Is ‘plantar heel pain’ a more appropriate term than ‘plantar fasciitis’? Time to move on. Br J Sports Med. 2017; 15(22):1576-1577. DOI:10.1136/bjsports-2017-097519
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Sullivan J, Pappas E, Burns J. Role of mechanical factors in the clinical presentation of plantar heel pain: implications for management. The Foot. 2020 Mar 1;42:101636. DOI:10.1016/j.foot.2019.08.007
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Ríos-León M, Ortega-Santiago R, Madeleine P, Fernández-de-Las-Peñas C, Plaza-Manzano G. Topographical pressure pain sensitivity maps of the feet reveal bilateral pain sensitivity in patients with unilateral plantar heel pain. Journal of Orthopaedic & Sports Physical Therapy. 2019 Sep;49(9):640-6. DOI: 10.2519/jospt.2019.8813
- ↑ 4.0 4.1 4.2 4.3 Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. Lived experience and attitudes of people with plantar heel pain: a qualitative exploration. Journal of foot and ankle research. 2020 Dec;13(1):1-9. DOI: 10.1186/s13047-020-0377-3
- ↑ Cichowitz A, Pan WR, Ashton M. The heel: anatomy, blood supply, and the pathophysiology of pressure ulcers. Annals of plastic surgery. 2009 Apr 1;62(4):423-9. DOI:10.1097/sap.0b013e3181851b55
- ↑ 6.0 6.1 6.2 6.3 Palastanga N, Soames R. Anatomy and Human Movement, Structure and Function. 6th ed. Churchill Livingstone: Elsevier. 2012.
- ↑ Gupton M, Terreberry RR. [https:/www.statpearls.com/kb/viewarticle/18764|Anatomy, bony pelvis and lower limb, calacaneous.] InStatPearls [Internet] 2018 Dec 6. StatPearls Publishing. Available from:[1] (last accessed 23.10.23)
- ↑ Palastanga N, Field D, Soames R. Anatomy and human movement. 4th edition. Oxford. Butterworth-Heinemann; 2002. p242.
- ↑ Luijkx T, Elthokapy M, Gregory L, et al. Calcaneus. Reference article, Radiopaedia.org. Available from https://radiopaedia.org/articles/calcaneus [last access 23 Oct 2023]
- ↑ Levangie PK, Norkin CC. Joint structure and function: a comprehensive analysis. 5th ed. Philadelphia, PA: FA Davis Company. 2011.
- ↑ 11.0 11.1 11.2 11.3 11.4 Thomas MJ, Whittle R, Menz HB, Rathod-Mistry T, Marshall M, Roddy E. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC musculoskeletal disorders. 2019 Dec;20(1):1-8. DOI:10.1186/s12891-019-2718-6
- ↑ 12.0 12.1 12.2 Rasenberg N, Bierma-Zeinstra SM, Bindels PJ, van der Lei J, van Middelkoop M. Incidence, prevalence, and management of plantar heel pain: a retrospective cohort study in Dutch primary care. British Journal of General Practice. 2019 Nov 1;69(688):e801-8. DOI:10.3399/bjgp19X706061
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Saban B, Masharawi Y. Pain threshold tests in patients with heel pain syndrome. Foot & ankle international. 2016 Jul;37(7):730-6. DOI:10.1177/1071100716642038
- ↑ Saban B, Masharawi Y. Pain threshold tests in patients with heel pain syndrome. Foot & ankle international. 2016 Jul;37(7):730-6. DOI:10.1177/1071100716642038
- ↑ 15.0 15.1 15.2 Alshami AM, Souvlis T, Coppieters MW. A review of plantar heel pain of neural origin: differential diagnosis and management. Manual therapy. 2008 Apr 1;13(2):103-11.
- ↑ Morrissey D, Cotchett M, J'Bari AS, Prior T, Griffiths IB, Rathleff MS, Gulle H, Vicenzino B, Barton CJ. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. British Journal of Sports Medicine. 2021 Mar 30. DOI:10.1136/bjsports-2019-101970