Iliopsoas Bursitis
Definition/Description[edit | edit source]
A Bursitis is an inflamed bursa. The inflammation can be a result of friction from the overlying tendons. A bursa is mostly flattened and is filled with a thin layer of synovial fluid. It appears for example at a junction of a tendon on the bone. The iliopsoas bursa separates the muscle or tendon from bone and facilitates movement by reducing friction between the anterior hip capsule and the iliopsoas.[1] The iliopsoas bursitis is one of the affections related to anterior hip pain.
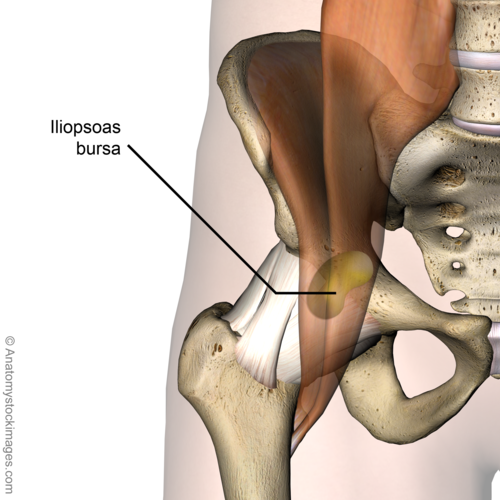
Clinically Relevant Anatomy[edit | edit source]
The iliopsoas bursa is the largest bursa of the human body and is bilaterally present in 98% of adults. This bursa is bounded by the musculotendinous junction of the M. iliopsoas (anteriorly) and by the fibrous capsule of the hip (posteriorly). It extends from the inguinal ligament superiorly to the lesser trochanter inferiorly and is flanked by the femoral vessels (medially) and the femoral nerve (laterally). [2]The bursa is always collapsed, when in healthy condition. In some situations the bursa is enlarged and contains fluid. When enlarged, it may cause a variety of symptoms such as pain, and immobility.[3][1]
Epidemiology /Etiology[edit | edit source]
Iliopsoas bursitis is mainly caused by certain types of arthritis such as rheumatoid arthritis and psoriatic arthritis[4], acute trauma and overuse injury. When an acute or chronic occupational trauma incurred during sport activities, a bursitis is likely the result of multiple mini-traumas caused by vigorous hip flexion and extension. Iliopsoas bursitis is commonly seen in individuals participating in strength training, rowing, uphill running and competitive track and field.
There are a few theories concerning the origin of symptoms of iliopsoas bursitis. One of them points that when the hip is in flexion, both the iliopsoas muscle and the anterior part of the bursa move away from the hip joint.[1] If the hip is to be hyperextended suddenly, there is a great tension that stretches the muscle and the bursa. This stretching traumatizes the bursa. Another theory hypothesizes that when a flexed, abducted and externally rotated hip, with iliopsoas bursitis, is brought in an extension, it causes an interruption of the lateral to medial movement of the iliopsoas tendon. This results in a painful snapping of the tendon over the femoral head, and over the anterior hip capsule.
Inevitably, iliopsoas bursitis and tendinitis are interrelated, where inflammation of the one will result in inflammation of the other because of their close proximity. In their presentation, etiology and treatment, the two conditions are almost identical. Together it is called the iliopsoas syndrome.[1]
Patients with rheumatoid arthritis can also suffer from iliopsoas bursitis. Joint synovium is the main target of rheumatoid arthritis, but sometimes, synovial tissues of tenosynovium and bursae, are also involved. This results from the inflammatory process in the hip joint, extending in the iliopsoas bursitis. This kind of bursitis mainly affects young adults. It occurs slightly more often in women than in men.[1] (Level of evidence: A1)
Characteristics/Clinical Presentation[edit | edit source]
- Pain is felt in the anteromedial aspect of the thigh
- Pain radiated into the knee, leg and lower back.
- Tenderness in the upper quads (M. Quadriceps).
- A snapping sensation at the front of the hip.
- Pain develops during walking or specific movements like crossing the legs.
- Pain on hip flexion, resisted as well as passive.
- Pain on internal rotation or passive hyperextension.
- Stiffness or pain after a rest or in the mornings.
- Pain is worse while performing activities.
- Rest can relieve the pain.
Differential Diagnosis[edit | edit source]
- Several joint diseases can cause distension[5]: Osteoarthritis, Rheumatoid arthritis, Avascular necrosis, Pigmente villonodular synovitis, Synovial chondromatosis, Gout, Chondrocalcinosis, Trauma, Lupus erythematodes, Pyogenic infection[2], Snapping hip.
- Differential diagnosis of anterior hip pain by anatomical structure[5]:
- Joint
o Osteoarthritis
o Inflammatory synovitis
o Loose bodies (chondral, osteochondral, ossified, non-ossified, fibrous, foreign)
o Infection (septic joint)
o Crystal-induced synovitis (gout)
o Labral tears
- Joint
- Bone
o Femur
• Stress fracture
• Avascular necrosis of femoral head
• Bone tumour
• Infection
o Femoroacetabular impingement (two types: cam impingement occurs from an abnormal head junction of the femur, pincer impingement is because of over coverage of the acetabulum)
o Pelvis
• Hip fracture
• Stress fracture
• Osteitis pubis - Muscle, tendon, bursa
o Iliopsoas bursitis and tendinitis
o Iliopsoas strain
o Rectus femoris strain
o Tight iliotibial band
o Gluteus medius en minimus problems
o Capsular laxity causing instability (due to traumatic dislocation or overuse) - Vasculature
o Aneurysm
o Arteriovenous malformation - Pelvic mass
o Gastrointestinal causes (e.g. hernia)
o Genitourinary causes (e.g. ureteral stone) - Nerve
o Obturator nerve entrapment
o Myalgia paraesthetica
o Referred from lumbar spine (L1, L2)
Diagnostic Procedures[edit | edit source]
Iliopsoas bursitis is often under-diagnosed due to its unspecific symptomatology. Careful and deep palpation in the femoral triangle medial or lateral to the femoral artery, with pressure applied on the bursa will result in pain. To elicit a patient’s hip pain, a clinical maneuver is commonly used. It involves the extension of their flexed, abducted and externally rotated hip where a tangible or audible ‘snap’ in the hip is almost always noted.[1] It is also possible that the inguinal region is painful when palpating it. A known or suspected osteoarthritis, snapping hip syndrome and a palpable inguinal or pelvic mass could raise the suspicion of an inflamed iliopsoas bursa and lead to further imaging examinations.[6]
To exclude other possible hip problems, and to get a more realistic idea about the size of the bursa, a 3D image is recommended, preferably an MRI-scan. The MRI-scan can distinguish the iliopsoas bursitis from other possible problems such as a tumor, a hernia, a hematoma and an aneurysm. However, a musculoskeletal ultrasound is the most cost-efficient way. Other frequently used options are to exclude problems of the bone are an X-ray and a bone scan. The computed tomography or CT-scan is also a commonly used instrument.[5][6]
An arthrography can determine instability and intra-articular pathology. A radiograph can also indicate an underlying problem of the hip, such as osteoarthritis and rheumatoid arthritis.[5] [6]
Outcome Measures[edit | edit source]
- International Hip Outcome Tool (iHOT)
- Hip disability and Osteoarthritis Outcome Score (HOOS)
- Lower Extremity Functional Scale (LEFS)
Examination[edit | edit source]
- Movement: The patient feels pain in the anteromedial aspect of the thigh when doing a hip flexion and internal rotation. There is a limitation in range of motion (ROM) according to a non-capsular pattern. Flexion is lightly painful at the end of ROM. Sometimes pain can be felt at the end of ROM when extension or adduction is performed. The most painful movement is adduction with the hip in flexion.
- Palpation: bursitis can be palpated as an oedematous mass in the groin region. A palpable and/or audible snap can be present.[1] (level of evidence: A1)Tenderness in femoral triangle.
- Positive Thomas test
- Active resisted testing of the iliopsoas.
- (Dynamic) Ultrasound.[7][8] (Level of evidence: 1B)]
Medical Management[edit | edit source]
The patient can take anti-inflammatory medications as it is traditionally indicated.[1] (Level of evidence: 1A) The treatment of iliopsoas bursitis is individualized for each patient according to the cause, pain severity and associated symptoms. [9] If the symptoms are severe ultrasound-guided aspiration could be performed. Ultrasound can be used to show the iliopsoas muscle flipping over the iliacus muscle to confirm the diagnosis of snapping iliopsoas, and in many cases an associated iliopsoas bursitis will also be visualized. A combination of local anesthetic and corticosteroid injection performed into the iliopsoas bursa can often provide symptomatic relief and avoid the need for surgery.[10] (Level of evidence: 1B)
A surgical intervention may be necessary with refractory iliopsoas bursitis, such as bursectomy to remove the bursa, capsulectomy to gain access to the iliopsoas bursitis, or synovectomy – the surgical removal of a part of the synovial membrane, possibly with iliopsoas tendon release.[1] [9]
Physical Therapy Management[edit | edit source]
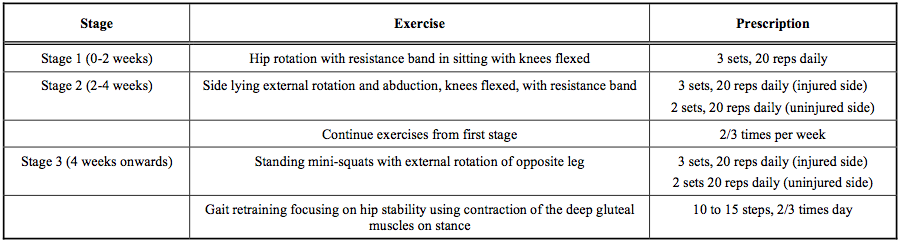
Traditionally the initial treatment of iliopsoas bursitis includes rest, stretching of the hip flexor muscles, strengthening exercises of the hip rotators and physical therapy. Generally successful stretching exercises to alleviate or ease the symptoms are the ones involving a hip extension, done for 6 to 8 weeks. The stretching program has to continue at least as long as the pain is present. The patients also have to avoid the aggravating activity of sports as much as possible during the initial treatment. [1][11](Level of Evidence: 1A).
The majority of the patients with iliopsoas bursitis have a considerable hip rotation muscle weakness. This has been shown with manual muscle testing as well as isokinetic evaluation. A reduction in symptoms can be achieved with an improvement in hip rotation strength.[1] Strengthening exercises for the hip rotators (both internal and external), hip flexors, buttocks, quadriceps and hamstrings are included in the treatment protocol and performed daily for as long as the symptoms persist.[1] [11]
During gait, the weakened gluteal muscles can cause for a decrease in hip stability. That is why the retraining of the gait is also very important and forms a final critical component of the treatment regime. During these exercises the patients have to maintain an appropriate hip stability by voluntarily contracting the deep gluteal muscles of the stance leg during the mid to late portion of the stance phase of the gait cycle.[1] [11] Before being able to reach the automaticity of contracting the gluteal muscles during gait, the patient has to do strengthening exercises. A good exercise for example is the pelvic drop you can find here.[12](Level of Evidence: 2C)]
The clinical practice of exercise therapy as a major component of rehabilitation for groin pain in athletes continues to be supported by the available evidence to date. Exercise, particularly strengthening exercises of the hip and abdominal muscles, could be an effective intervention for patients suffering from groin pain, thus iliopsoas bursitis or iliopsoas syndrome. Although literature provides foundational evidence that the exercises should be performed as static to functional, regarding the most effective intensity and frequency of exercise, there is no clear evidence due to lack of reporting.
Rehabilitation Programme for Iliopsoas Syndrome (adapted from Johnston et al. 1998) [1][13] (Level of evidence: 1A)
See more exercises on Therapy exercises for the hip
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Johnston, C.A.M., Wiley, J.P., Lindsay D.M., & Wisemand D.A. (1998, April). Iliopsoas bursitis and tendinitis: A review. Sports Med, 25(4), 271-283 (Level of evidence: 1A)
- ↑ 2.0 2.1 Van de Perre, S., Vanwambeke, K., Vanhoenacker, F.M., & De Schepper, A.M., (2005). Posttraumatic iliopsoas bursitis. Journal Belge de Radiologie – Belgisch Tijdschrift voor Radiologie, 88, 154-155.
- ↑ Matsumoto, T., Juji, T., & Mori, T. (2006, December). Enlarged psoas muscle and iliopsoas bursitis associated with a rapidly destructive hip in a patient with rheumatoid arthritis. Modern Rheumatology, 16(1), 52-54 (Level of evidence: 3A)
- ↑ Arromdee E, Matteson EL. Bursitis: common condition, uncommon challenge. The Journal of Musculoskeletal Medicine. 2001 Apr 1;18(4):213-224.
- ↑ 5.0 5.1 5.2 5.3 Tibor, L.M., & Sekiya, J.K. (2008). Differential diagnosis of pain around the hip joint. The Journal of Arthroscopic & Related Surgery, 24(12), pp. 1407-1421
- ↑ 6.0 6.1 6.2 Skiadas, V., Koutoulidis, V., & Plotas, A. (2009, October). An atypical case of noninfected iliopsoas bursitis: MRI findings. Journal of Radiology Case Reports. doi:10.3941/jrcr.v3i10.326
- ↑ Wyss, J., & Patel, A. (2013). Therapeutic programs for musculoskeletal disorders. New York, NY: Demos Medical Publishing.
- ↑ Noesberger B., & Eichenberger, AR. (1997). Overuse injuries of the hip and snapping hip syndrome. Operative Techniques in Sports Medicine, 5(3), 138-142 (Level of evidence 1B)
- ↑ 9.0 9.1 Gilliland, W.R., Murphey, M.D., Papadopoulos, P.J., & Zembrzuska, H. (2012, March). Iliopsoas Bursitis. The Journal of Musculoskeletal Medicine. Accessed through http://www.musculoskeletalnetwork.com
- ↑ Grainger, A.J., & Rowbotham, E.L. (2011, July) Ultrasound-guided intervention around the hip joint: Musculoskeleteal imaging – review. American Journal of Roentgenology, 197(1). doi:10.2214/AJR.10.6344 (Level of evidence: 1B)
- ↑ 11.0 11.1 11.2 Johnston, C.A.M., Lindsay, D.M., & Wiley, J.P. (1999). Treatment of iliopsoas syndrome with a hip rotation strengthening program: A retrospective case series. Journal of Orthopaedic & Sports Physical Therapy, 29(4), 218-224. (Level of evidence: 4)
- ↑ O’Sullivan, K., Smith, S.M., & Sainsbury, D. (2010). Electromyographic analysis of the three subdivisions of gluteus medius during weight-bearing exercises. BMC Sports Science, Medicine & Rehabilitation. doi:10.1186/1758-2555-2-17 (Level of evidence: 2C)
- ↑ Quinn., A. (2010). Hip and groin pain: Physiotherapy and rehabilitation issues. The Open Sports Medicine Journal, 4, 93-107