Hypoxic Ischemic Encephalopathy
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (18/06/2022)
Introduction[edit | edit source]
Hypoxic Ischemic Encephalopathy (HIE) is a condition in which injury to the brain of a neonate occurs following deprivation of oxygen supply to brain. [1]It is the common cause of neonate mortality and developmental psychomotor disorders in the pediatric worldwide.[2]This is one of the major cause for cerebral palsy.
Attributing neonatal encephalopathy to perinatal hypoxic–ischemic injury requires combinations of parameters indicative of metabolic acidosis in the first postnatal hours with low cord pH (<7.0), base deficit of over 12, and evidence of a need for respiratory support also starting in the first minutes, with low Apgar scores at and beyond 5 min.
Epidemiology[edit | edit source]
- The incidence of HIE is ~1–8 per 1,000 live births in technically advanced countries and is up to 10-20 per 1,000 live births in less developed countries.[2]
Etiology[edit | edit source]
Maternal factor
Fetal factor
Delivery condition
Mechanism of Injury / Pathological Process[edit | edit source]
Clinical Presentation/manifestation[edit | edit source]
Fetal asphysia:
Meconium stained liquor:
APGAR score
Seizure
tone
Classification of HIE[edit | edit source]
There are three classification system of HIE
Levene[edit | edit source]
Sarnat and Sarnat staging[edit | edit source]
Harvey B. Sarnat and Margaret S. Sarnat first published a study related to the Sarnat staging system with 21 neonates with encephalopathy attributed to a “well-defined episode of fetal distress or an Apgar score of ≤5 at 1 or 5 min after delivery.”. Their staging system for the sequential evolution of clinical signs and electroencephalogram (EEG) changes was intended to facilitate formulation of prognosis for neurologic outcome.
Later, modifications of the Sarnat Scoring System have been employed in the major trials of therapeutic hypothermia for neonatal hypoxic–ischemic encephalopathy (HIE) to identify neonates at highest risk for abnormal neurodevelopmental outcome.
Thompson scoring[edit | edit source]
In 1997, Thompson et al. tested a numeric scoring system with fewer clinical assessment-based items in 45 neonates with HIE. In contrast to the Sarnat scale, the Thompson score did not require categorization of severity of encephalopathy but rather relied on a simple numeric score to describe the peak severity of encephalopathy.
By design, the Thomspon score did not require specific training or depend on the availability of advanced technologies (e.g., magnetic resonance imaging, computed tomography, cerebral function monitoring).
The score consisted of clinical assessment of nine signs: tone, level of consciousness, seizures, posture, Moro, grasp, suck, respiratory pattern, and fontanelle findings. Each sign was scored from 0 to 3, making highest score of 27 and lowest score of 0.
It has performed daily until a score of 0 was achieved or the infant was discharged from the hospital.
Limitations:
- unclear inclusion criteria for infants (“if clinical signs of hypoxic–ischemic encephalopathy developed after birth”)
- a small sample size.
Complication[edit | edit source]
Outcome measures[edit | edit source]
Investigations[edit | edit source]
- EEG
- Cranial ultrasound
- CT scan
- MRI
Management / Interventions[edit | edit source]
Medical Management[edit | edit source]
- Therapeutic Cerebral Hypothermia
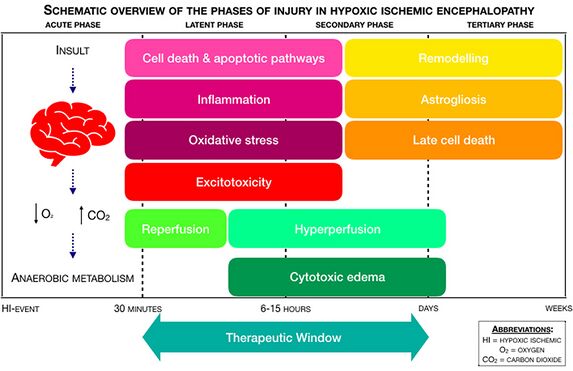
- Hypothermia is a proven effective treatment of HIE and can improve survival and long-term prognosis of children. It has been suggested that hypothermia treatment of HIE should start within 6 hours after hypoxia ischemia.
- Medications
Physiotherapy Management[edit | edit source]
Prognosis[edit | edit source]
Depending upon the severity of brain damage and medical treatment, usally:
Mild or moderate cases could be cured completely, but severe cases represent poor prognosis with high mortality or cerebral complications such as mental retardation and cerebral palsy.
Overall mortality: 20%
Overall incidence of sequel: 30%
Mild: 100% good prognosis
Moderate: 80% normal
Severe: 50 5 death , 50% sequel
Presence of seizure increases chance of cerebral palsy by 50-70 times
Prevention[edit | edit source]
- Better obstetric care
- Skilled resuscitation teams and neonatal facilities
Differential Diagnosis[edit | edit source]
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ Greco P, Nencini G, Piva I, Scioscia M, Volta CA, Spadaro S, Neri M, Bonaccorsi G, Greco F, Cocco I, Sorrentino F. Pathophysiology of hypoxic–ischemic encephalopathy: a review of the past and a view on the future. Acta Neurologica Belgica. 2020 Apr;120(2):277-88.
- ↑ 2.0 2.1 Kleuskens DG, Goncalves Costa F, Annink KV, van den Hoogen A, Alderliesten T, Groenendaal F, Benders MJ, Dudink J. Pathophysiology of cerebral hyperperfusion in term neonates with hypoxic-ischemic encephalopathy: A systematic review for future research. Frontiers in pediatrics. 2021:17.