Hip Anatomy
Original Editor - Tyler Shultz
Top Contributors - Tyler Shultz, Admin, Kim Jackson, Aarti Sareen, Samuel Adedigba, Lucinda hampton, Laura Ritchie, Leana Louw, Rachael Lowe, Scott Buxton, Joao Costa, Ewa Jaraczewska, Ahmed M Diab, WikiSysop, Kirenga Bamurange Liliane, Evan Thomas, George Prudden and Priyanka Chugh
Description[edit | edit source]
The hip articulation is true diarthroidal ball and-socket style joint, formed from the head of the femur as it articulates with the acetabulum of the pelvis. This joint serves as the main connection between the lower extremity and the trunk, and typically works in a closed kinematic chain.
Motions Available[edit | edit source]
- Flexion: forward and upward movement of the femur at the hip occurs in the sagittal plane about an medial-lateral axis.
- Extension: upward movement toward the rear of the body of the femur at the hip occuring in the sagittal plane.
- Abduction: movement of the femur on the hip in a direction away from the midline of the body in the frontal plane.
- Adduction: movement of the femur on the hip in a direction toward the midline of the body in the frontal plane.
- Internal Rotation: rotation of the femur toward the midline of the body in the transverse plane.
- External Rotation: rotation of the femur away from the midline of the body in the transverse plane.
Ligaments & Joint Capsule[edit | edit source]
- Ligamentum Teres[3]: This ligament is located entirely within the hip joint. It spans the hip running from the acetabular notch to the fovis capitis of the femur, attaching the femoral head to the inferior acetabular rim. This ligament is joined with nerves and vessels that pass to the femoral head. The vascular component of this structure is important during development, but is less significant in children. This ligament becomes taut during adduction, flexion, and external rotation, but only minimally contributes to joint stability.
- Ischiofemoral Ligament: Is the only ligament located on the posterior aspect of the hip. It attaches to the posterior surface of the acetabular rim and labrum. This ligament is said to "wind" around the joint and insert on the anterior aspect of the femur. The location and orientation of this ligament reinforces the joint capsule posteriorly and checks against excessive extension and internal rotation of the hip joint.
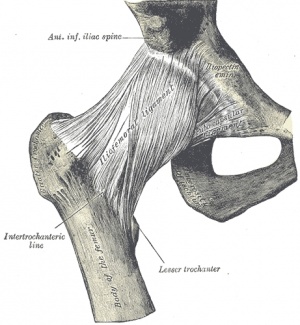
- Iliofemoral Ligament (Y Ligament of Bigelow): Attaches to the AIIS and then fans out to attach along the intertrochanteric line of the femur. The iliofemoral ligament is the strongest ligament in the body, and checks extension, adduction (superior fibers), and abduction (inferior fibers). In addition, because this ligament limits hip extension, it allows maintenance of the upright posture by reducing the need for muscle contractions.
- Pubofemoral Ligament: Is located on the anterior portion of the joint, arising from the anterior aspect of the pubic ramus and passing to the anterior surface of the intertrochanteric fossa. This ligament's main purpose is to check hip abduction and extension. This ligament may blend with the inferior fibers of the iliofemoral ligament.
Joint Capsule:
- The hip joint is extremely strong, due to its reinforcement by strong ligaments and musculature, providing a relatively stable joint. Unlike the weak articular capsule of the shoulder, the hip joint capsule is a substantial contributor to joint stability[2]. The capsule is thicker anterosuperiorly where the predominant stresses of weight bearing occur, and is thinner posteroinferiorly.
Labrum[edit | edit source]
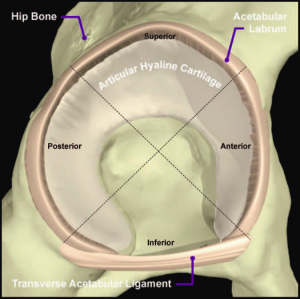
The labrum forms a fibrocartilagenous extension of the bony acetabulum, mostly composed of type 1 collagen that is typically between 2-3mm thick. It lines the acetabular socket and attaches to the bony rim of the acetabulum. It has an irregular shape, being wider and thinner anteriorly and thicker posteriorly.[4][5] On the anterior aspect, the labrum is triangular in the radial section. On the posterior aspect, the labrum is dimensionally square but with a rounded distal surface.[6][7]
The labrum has three surfaces:
- Internal articular surface - adjacent to the joint (avascular)
- External articular surface - contacting the joint capsule (vascular)
- Basal surface - attached to the acetabular bone and ligaments
The transverse ligaments surround the hip and help hold it in place while moving.
It is thought that the majority of the labrum is avascular with only the outer third being supplied by the obturator, superior gluteal and inferior gluteal arteries. There is controversy as to whether there is a potential for healing with the limited blood supply and this is an important clinical consideration. The superior and inferior portions are believed to be innervated, containing both free nerve endings and nerve sensory end organs (giving the senses of pain, pressure and deep sensation).[4][5]
The functions of the acetabular labrum are:[4]
- Joint stability - increases the containment of the femoral head, deepening the joint by 21%, increasing the surface area of the joint by 28%, thus allowing a wider area of force distribution and resisting lateral and vertical motion within the acetabulum
- Sensitive shock absorber
- Joint lubricator - sealing mechanism keep the synovial fluid in contact with the articular cartilage
- Pressure distributor - obstructs fluid flow in and out of the joint through a sealing action which is often referred to as a “suction effect” in view of the resistance generated to distraction of the head from the acetabular socket. This sealing function not only enhances joint stability, but is thought to more uniformly distribute compressive loads applied to the articular surfaces, thereby reducing peak cartilage stresses during weight-bearing.[8]
- Decreasing contact stress between the acetabular and the femoral cartilage[9][10]
Muscles[edit | edit source]
Flexors:
- Psoas Major
- Psoas Minor
- Iliacus
- Pectineus
- Rectus Femoris
Extensors:
Adductors:
- Adductor Magnus
- Adductor Longus
- Adductor Brevis
- Gracilis
- Pectineus
Abductors:
Internal Rotators:
External Rotators:
- Gluteus Maximus
- Gemellus Superior
- Gemellus Inferior
- Obturator Externus
- Obturator Internus
- Quadratus Femoris
- Piriformis
Closed Packed Position[edit | edit source]
Full extension of the hip joint is the closed packed postion because this position draws the strong ligaments of the joint tight, resulting in stability.
Open Packed Position[edit | edit source]
The hip joint is one of the only joints where the position of optimal articular contact (combined flexion, abduction, and external rotation) is the open-packed, rather than closed packed position, since flexion and external rotation tend to uncoil the ligaments and make them slack.[2]
Other Important Information[edit | edit source]
- Femoral Triangle: The femoral triangle is the region defined by the inguinal ligament superiorly, the adductor longus medially, and the sartorius laterally. This region is important because it contains numerous vascular and neural structures, including the femoral vein, artery, and nerve.
- Femoral Angle of Inclination: The angle of inclination is formed from the angle resulting from the intersection of a line down the long shaft of the femur and a line drawn threough the neck of the femur. Typically, the normal adult has an angle of inclination between 120 and 125 degrees, it usually is closer to 125 in the elderly. An increase in this angle, greater than 125 degrees, results in coxa valga, and a decrease is called coxa vara*.
- Femoral Angle of Torsion: The angle of torsion is formed by looking at the relationship between the axis of the femoral head and neck and the femoral condyles. The normal femur has an angle of torsion between 12 and 15 degrees. An increase in this angle is termed anteversion, while a decrease in this angle is termed retroversion*.
- It is important to note that both normal and abnormal angles of inclination and torsion are properties of the femur, and exist independently of the hip joint, however, abnormalities typically alter joint stability.[2]
Applied Anatomy[11][edit | edit source]
Trendlenberg's gait[edit | edit source]
When any of the features of lateral balance control fails, the supporting is upset. The pelvis tends to fall on the unsupported side when the individual stands on the affected limb. This is called Trendelenberg sign. The person walks with a characteristic lurching or waddling gait.
In A: Negative trendlenberg's test. The hip abductors are acting normally tilting the pelvis upwards when the opposite leg is raised from the ground.
In B: Positive Trendelenberg's test. The hip abductors are unable to control the dropping of the pelvis when the opposite leg is raised
Causes of such a condition include:
Paralysis of the gluteus minimus and medius
Dislocation of the hip joint
Fractures of the neck of the femur
Collapse of the head of the femur e.g. from avascular necrosis, slipped epiphysis, tuberculosis of head of femur
Severe arthritis of the hip joint
Sciatic nerve[edit | edit source]
Can be compressed at lower border of gluteus maximus by sitting on a bench with a sharp edge.
May be injured by misplaced deep intravascular injections. To prevent this, the injection is usually given in the superolateral quadrant.
May be injured in posterior dislocation of the hip joint.
Sciatic Hernia[edit | edit source]
Pelvic structures may protrude through the greater sciatic foramen. This is called sciatic hernia. It compresses the contents of the foramina and may present with pain, numbness and weakness in the lower limb if sciatic nerve is compressed.
Trochanteric bursitis[edit | edit source]
The extensive bursa between the great trochanter and the gluteal aponeurosis may be a site of infection. Patient complains of pain and swelling in the trachanteric region. Sometimes there may be a pus discharge.
Snapping hip[edit | edit source]
In this condition, a snap is heard and felt on certain hip movements. The snap is attributed to slipping of a tendinous aponeurosis- probably that of the gluteus maximus – over the greater trochanter. It is harmless and treatment is not required.
Slipped disc[edit | edit source]
Pain of a prolapsed or strained lumbar intervertebral disc if often referred to the gluteal region or lateral aspect of the thigh.
Weaver's bottom[edit | edit source]
Inflammation of the bursa over the ischial tuberosity.
Piriformis syndrome[edit | edit source]
When the sciatic nerve divides in the pelvis, the common peroneal nerve may exit either:
below Piriformis
pierce piriformis
pass above piriformis
When it pierces piriformis, it may be compressed by contractions of this muscle. This causes piriformis syndrome.
References[edit | edit source]
- ↑ Dutton M. Orthopaedic: Examination, evaluation, and intervention. 2nd ed. New York: The McGraw-Hill Companies, Inc; 2008.
- ↑ 2.0 2.1 2.2 2.3 Levangie P, Norkin C. Joint structure and function: A comprehensive analysis. 4th ed. Philadelphia: The F.A. Davis Company; 2005.
- ↑ Anerson L. The anatomy and biomechanics of the hip joint. J Back Musculoskeletal Rehabil. 1994;4(15):145-153.
- ↑ 4.0 4.1 4.2 Groh MM, Herrera J. A comprehensive review of hip labral tears. Curr Rev Musculoskeletal Med. 2009; 2:105 - 117.
- ↑ 5.0 5.1 Lewis C, Sahrmann S. Acetabular labral tears. Physical Therapy. 2006;86(1):110-121.
- ↑ Narvani AA, Tsiridis E, Tai CC, Thomas P. Acetabular labrum and its tears. Br J Sports Med 2003;37:207-211.
- ↑ Lovell G. The diagnosis of chronic groin pain in athletes; a review of 189 cases. Aust J Sci Med Sport 1995;27:76-9
- ↑ Crawford M, Dy C, Alexander J, et al. The 2007 Frank Stinchfield Award. The Biomechanics of the hip labrum and the stability of the hip. Clinical Orthopaedics and Related Research. 2007;465:16-22.
- ↑ Byrd JW. Labral lesions: an elusive source of hip pain case reports and literature review. Arthroscopy 1996;12:603–612.
- ↑ Martin RL, Enseki KR, Draovitch P, et al. Acetabular labral tears of the hip: examination and diagnostic challenges. J Orthop Sports Phys Ther 2006;36:503-15.
- ↑ OG Anatomy. Gluteal region and back of the thigh. Available from http://www.oganatomy.org/projanat/gross/5/clinicalanatomy.htm