Heart Failure
Original Editors - Students from Glasgow Caledonian University's Cardiorespiratory Therapeutics Project.
Top Contributors - Lucinda hampton, Jayati Mehta, Vidya Acharya, Doireann Church, Caoimhe Mackey, Kim Jackson, Areeba Raja, Admin, WikiSysop, 127.0.0.1, Evan Thomas, Michelle Lee, Karen Wilson and Aminat Abolade
Definition/Description[edit | edit source]
Heart failure is a complex clinical syndrome of symptoms and signs that suggest impairment of the heart as a pump supporting physiological circulation[1]. It occurs when the heart becomes less efficient at pumping blood around the body at the right pressure in order to sustain bodily functions to a high standard[1]. It commonly is a result of myocardial muscle dysfunction or loss, and is characterised by left ventricle dilation or hypertrophy, elevated cardiac filling pressure and/or inadequate peripheral oxygen delivery, at rest or during stress[2].
The condition can be acute, transient, or chronic:
- Acute is the first presentation of heart failure or a sudden onset of heart failure
- Transient is when heart failure is recurrent or episodic
- Chronic is heart failure that is persistent, worsening, or decompensate. It usually offset at first by compensatory mechanisms to maintain tissue perfusion, but eventually cardiac function declines and symptoms develop.[1]
Classification[edit | edit source]
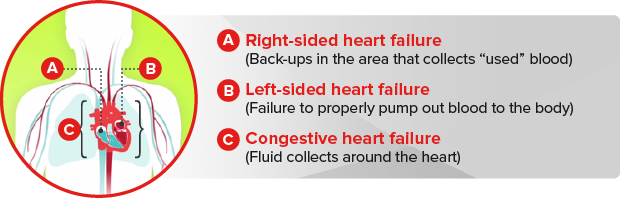
Heart failure can be classified into three different types:
Left Ventricular Failure (LVF):[edit | edit source]
This is the most common form of heart failure, gradually pushing up pressure in the left atrium and pulmonary vascular system. The resulting pulmonary hypertension may force fluid into the alveoli creating a pulmonary oedema. This can cause compensatory mechanisms[3]:
- Fast-acting neural systems increase sympathetic acting, raising heart rate and myocardial contractility
- The slower response of the renin-angiotensin mechanism promotes the retention of sodium and water by the kidney, increasing preload and encouraging myocardium to contract
The compensatory mechanisms raise the workload of the left ventricle further because angiotensin is an arterial vasoconstrictor and increases the afterload. Other factors that can increase the workload of the left ventricle are increased volume load as in aortic valve regurgitation, or increased resistance to flow such as with systemic hypertension.[2]
Right Ventricle Failure (RVF):[edit | edit source]
This generally occurs secondary to cardiopulmonary disorders such as pulmonary hypertension, right ventricle infarction, congenital heart disease, pulmonary embolism or COPD. It is usually irreversible unless the ventricles is under-loaded e.g. by lung transplant for pulmonary hypertension. Enlargement of the right ventricle that has resulted from lung disease is referred to as cor pulmonale and is caused by hypoxic vasoconstriction and pulmonary hypertension.[3]
Congestive Cardiac Failure (CCF): [edit | edit source]
The combination of LVF and RVF with congestion in the pulmonary and systemic circulations[3]
Helpful Terminology:
- Stroke volume: volume of blood ejected by the ventricle in one contraction, usually 70ml
- End diastolic volume: volume of blood in the ventricle at the end of filling, just before it contracts, usually 120ml
- Ejection fraction: stroke volume expressed as a percentage of end-diastolic volume, normally >55%
- Systolic heart failure: reduced or weakened pumping action of the heart, with ejection fraction <55%
- Diastolic heart failure: low compliance of myocardium, but with normal contraction and normal ejection fraction
- Preload: degree of stretch applied to the ventricle before contraction
- Afterload: the load that the ventricle must overcome to eject blood[3]
NYHA GRADING[4][edit | edit source]
| CLASS | PATIENT SYMPTOMS |
| I | No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea (shortness of breath |
| II | Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea (shortness of breath). |
| III | Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitation, or dyspnea |
| IV | Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases. |
Epidemiology[edit | edit source]
It is estimated that around 800,000 people in the UK suffer from heart failure, a number which will continue to rise due to an ageing population, improved survival rates following a heart attack, and more effective treatments.[2] The prevalence of heart failure doubles with each decade. The British Heart Foundation statistics estimate the incidence and prevalence of heart failure in the UK, using the Clinical Practice Research data, show that both rise steeply with age.[2] The British Heart Foundation reports that 0.9% of men and 0.7% of women in the UK suffer from heart failure, rising to 13.1% of men and 11.9% of women aged over 75 years old.[2]
Heart failure is the leading cause of hospitalisation in the elderly population and accounts for one million inpatient bed-days[1]. Survival rates for heart failure patients are variable, dependent on the age and severity of disease of the patient, and the quality of care they receive[1]. Outcomes are consistently poor for patients who receive suboptimal care, but input from heart failure specialists and prescription of evidence-based heart failure therapies have a significant impact on prognosis and life expectancy[2]. The National Heart Failure Audit has reported around one in ten patients dying in hospital, and of those who survive between one-quarter and one-third dying within the year of their admission[2]. However, these mortality rates are beginning to reduce, reflecting more consistent implementation of guidelines for recommended practice.[2]
Aetiology[edit | edit source]
It is rare for heart failure to be derived from one cause, it is normally multi-factorial. A number of health conditions increase your chances of developing heart failure but in general, it is caused by an excess workload placed on the heart[3]. The excess workload on the heart involves on or both ventricles and is thought to relate to oxidative stress and inflammation which leads to one or more of the following:[3]
- Impaired contractibility of the myocardium, e.g. after acute coronary syndromes
- Increased afterload e.g. with hypertension or aortic valve stenosis
- Increased preload e.g. with mitral or aortic valve regurgitation
In addition anaemia, overactive thyroid gland (hyperthyroidism), pulmonary hypertension, diabetes, chronic renal impairment, chronic obstructive pulmonary disease (COPD), and asthma are reported as potential causes of heart failure.[1]
Pathophysiology[edit | edit source]
In response to increased load, the left ventricular myocardium hypertrophies. The greater size and number of myocytes raise myocardial oxygen demand and increases diffusion distance for oxygen. Some muscle fibres become ischaemic, leading to patchy fibrosis, stiffness and reduced contractability[1]. The workload may cause the ventricle to stretch and dilate, leading to further force being required to maintain cardiac output[1]. Systolic failure is by reduced ejection fraction and diastolic failure is by reduced end-diastolic volume. Metabolic effects include loss of bone mineralisation, skeletal muscle and fat[3].
The stiffness and reduced contractibility push up end-diastolic pressure, which is transmitted back along the pulmonary veins to the pulmonary capillaries, which causes fluid to be forced into the interstitial spaces and, if severe, into the alveoli, causing pulmonary oedema. The increased pulmonary vascular pressure raises the afterload of the right ventricle, in the same way as chronic systemic hypertension raises the afterload of the left ventricle[2]. Hypertrophy, patchy fibrosis, stiffness and reduced contractibility of the right ventricular myocardium then ensues, as with left ventricle, and congestive cardiac failure develops[1].
Clinical Manifestations[edit | edit source]
Typical[edit | edit source]
- Breathlessness
- Ankle swelling
- Fatigue
- Orthopnea
- Reduced Exercise Tolerance
These are the typical signs and symptoms of heart failure. Research suggests abnormalities of the pulmonary system leads to the exertional dyspnea and exercise intolerance and treating the pulmonary symptoms yield positive results in patients with chronic heart failure[6]. Another study suggests that patients with heart failure and diabetes had lower levels of exercise tolerance, as compared with patients without complications, which was a result of the decrease of autonomic nervous activity[7]. However, heart failure may be hard to diagnose using only these characteristics, especially in women, elderly, pregnant or obese patients as they are fairly common and widespread symptoms found in many other diseases. Due to this, suspected heart failure and patients following this pattern should be assessed carefully and using different methods to get a full picture of the condition.
Fatigue is an essential symptom of heart failure. The cause of fatigue includes low cardiac output, peripheral hypoperfusion, and skeletal muscle deconditioning and is confounded by difficulties in quantifying this symptom. ☃☃Peripheral oedema, raised venous pressure, and hepatomegaly are the characteristic signs of congestion of systemic veins. Clinical signs of heart failure should be assessed in clinical examinations including palpation observation,and auscultation of the patient.
More Specific [edit | edit source]
- Elevated Jugular Venous Pressure
- Heptojugular Reflux
- Third Heart Sound (Gallop Rhythm)
- Laterally Displaced Apical Impulse
- Cardiac Mumur
Management[edit | edit source]
Physiotherapy[edit | edit source]
Effective treatment for heart failure should aim to:
- Strengthen the heart
- Improve symptoms
- Reduce the risk of a flare-up or worsening of symptoms
- Improve Quality of Life
- Offer longevity
With all patients, especially heart failure populations, the complex interactions between the multidisciplinary teams involved is imperative. The study suggested a positive outcome of exercise training on heart rate variability in patients with heart failure after percutaneous coronary intervention[8].
A physiotherapist's role is to be involved before an incident occurs as a preventative method (if possible) whilst also improving quality of life, continuing recovery immediately after surgery and providing education to leading a more balanced life. Research suggests that physical therapists, along with other health care members, enhance the physical activity, participation, and quality of life in individuals with heart failure and reduce the incidence of heart failure-related hospital re.-admissions[9]
Systematic review and meta-analysis show a significant effect of aerobic and resistance training on peak oxygen consumption, muscle strength, and health-related quality of life in patients with heart failure with a reduced left ventricular ejection fraction[10]
Likewise, a recent study published in the Journal of Cardiopulmonary Rehabilitation and Prevention 2020, comparing the effects of β-blockers and non-β-blockers on Heart Rate (HR) and Oxygen Uptake (VO2) during exercise and recovery in older patients with heart failure with a preserved ejection fraction (HFpEF) demonstrated no significant differences in values (HRpeak, HRresv, HRrecov, or VO2) between both the groups, along with significant correlation between HRresv and VO2peak, suggesting the efficacy of these measures in prognostic and functional assessment and clinical applications, including the prescription of exercise, in elderly HFpEF patients[11].
The study by Lan NSR et al. shows a contrasting effect of aerobic training and resistance training on some echocardiographic parameters in patients with heart failure with reduced ejection fraction. While aerobic training was associated with evidence of worsening myocardial diastolic function, this was not apparent after resistance training. Further studies are indicated to investigate the long-term clinical significance of these adaptations[12].
А single-blind, prospective randomized controlled trial suggests that modified group-based High-intensity aerobic interval training (HIAIT) intervention showed more considerable improvement as compared to moderate-intensity continuous training (MICT) in the rehabilitation of patients with chronic heart failure (CHF). Thus, encouraging physical and rehabilitation medicine (PRM) physicians to apply Group based Cardiac intervention in routine cardiac rehabilitation (CR) practice[13].
Multidisciplinary team members[edit | edit source]
The other members of the MDT are vast but include
Surgeons and consultants -[edit | edit source]
They operate if needed. Numerous operations are available and may be suitable for certain patients. For example, Heart Valve Surgery, Angioplasty or Bypass, Left Ventricular Assist Devices, Heart Transplant.
However, this is individual and would need to be discussed with the consultant in charge of the case.
Nutritionists -[edit | edit source]
They work out a diet plan to suit the individual needs of the patient. As diet is a risk factor for CHD this is an extremely important member of the MDT for further prevention.
Counselor -[edit | edit source]
As Heart failure is normally a lifelong condition the patient may have difficulty coming to terms with the impact this will have on their life. A counsellor will be available for sessions on coping with the disease.
Personal Trainer-[edit | edit source]
As with a Physiotherapist will help to provide a more balanced lifestyle and improve fitness levels. This is something that will not only give the patient goals to work towards but also important social interaction with someone who is seen as less of a medical figure and therefore adds more normality to the individuals day to day life.
Family and Friends-[edit | edit source]
This support network is an extremely important factor contributing to recover of a patient and should not be overlooked.
The list of people involved in this team is huge and is not exhaustive in this piece, however, Pharmacists, Social Groups, GP’s, Nurses and Podiatrists are all members of this MDT.
Recovery cannot occur without input and communication from every member of the team.
Prevention[edit | edit source]
There are many factors that increase the risk of developing heart failure. And with some lifestyle changes and sometimes drug intervention this risk could be dramatically reduced. Hypertension and smoking are major risks for heart failure.
Stop smoking[edit | edit source]
Quitting smoking is noted as the single best way to reduce risk of heart failure. Smoking has many physiological effects forcing the heart to walk harder.
Smoking increasing viscosity of the blood, slowing the blood and therefore increasing risk of thrombosis (blood clots). It also causes damage to the arterie lining leading to atherosclerosis and reduction in artery diameter.
Reduce blood pressure[edit | edit source]
High blood pressure increases the work demand put on the heart to transport blood around the body, this increased work causes a hypertrophic reaction of the heart muscle, eventually leading to a weakened or stiff heart.
Blood pressure medications and exercise can be used to modulate blood pressure.
Reduce Cholesterol Level[edit | edit source]
High levels of cholesterol can cause furring and narrowing of the arteries termed atherosclerosis and eventually heart failure.
Lose weight[edit | edit source]
Being overweight increases demand placed on the heart and increases risk of heart failure and attack.
Eat a healthy diet[edit | edit source]
A healthy diet can help reduce your risk of developing coronary heart disease and therefore heart failure.
Keep active
Regular physical activity will help keep the heart healthy and also maintain a healthy weight.
Reduce Alcohol intake[edit | edit source]
Drinking excess of the recommended amount of alcohol per week can increase your blood pressure.
Heavy drinking for long periods of time can cause damage to your heart muscle leading directly to heart failure.
Cut your salt intake[edit | edit source]
Excessive salt intake increases blood pressure and again, increases stress put on the heart.
Resources[edit | edit source]
- http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/What-is-Heart-Failure_UCM_002044_Article.jsp#.WEfn2rJ97IU
- http://www.heart.org/HEARTORG/Conditions/HeartFailure/WarningSignsforHeartFailure/Warning-Signs-of-Heart-Failure_UCM_002045_Article.jsp#.WEiD7LJ97IU
- https://youtu.be/2aiRpr5UCZs?list=PLbKSbFnKYVY2LhsYihIVUBpW6DJGMSSC4
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Dickstein, K.ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Journal of Heart Failure. 2008. Aug;10:933-989.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 British Society for Heart Failure. National Heart Failure Audit. London. November 2013.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Hough, A. Physiotherapy in Respiratory and Cardiac Care: An Evidence Based Approach. Hampshire. Cengage Learning EMEA; 2014.
- ↑ http://www.heart.org/HEARTORG/Conditions/HeartFailure/AboutHeartFailure/Classes-of-Heart-Failure_UCM_306328_Article.jsp#.WF1jIFN97IU
- ↑ classification system of heart failure
- ↑ Lalande S, Cross TJ, Keller-Ross ML, Morris NR, Johnson BD, Taylor BJ. Exercise Intolerance in Heart Failure: Central Role for the Pulmonary System. Exercise and sport sciences reviews. 2019 Aug.
- ↑ ISHIHARA K, MORISAWA T, KAWADA J, NAGARE Y, KOYAMA T, YAGI H, SUEOKA M, YOSHIDA T, TAMAKI A. Influence of Complications of Diabetes Mellitus on Exercise Tolerance of Patients with Heart Failure: Focusing on autonomic nervous activity and heart rate response during cardiopulmonary exercise tests. Physical Therapy Research. 2019 Dec 20;22(2):81-9.
- ↑ Stein PK, Ehsani AA, Domitrovich PP, Kleiger RE, Rottman JN. Effect of exercise training on heart rate variability in healthy older adults. American heart journal. 1999 Sep 1;138(3):567-76.
- ↑ Shoemaker MJ, Dias KJ, Lefebvre KM, Heick JD, Collins SM. Physical therapist clinical practice guideline for the management of individuals with heart failure. Physical Therapy. 2020 Jan 23;100(1):14-43.
- ↑ Neto MG, Durães AR, Conceição LS, Roever L, Silva CM, Alves IG, Ellingsen Ø, Carvalho VO. Effect of combined aerobic and resistance training on peak oxygen consumption, muscle strength and health-related quality of life in patients with heart failure with reduced left ventricular ejection fraction: a systematic review and meta-analysis. International Journal of Cardiology. 2019 Jun 24.
- ↑ Maldonado-Martín S, Brubaker PH, Ozemek C, Jayo-Montoya JA, Becton JT, Kitzman DW. Impact of β-Blockers on Heart Rate and Oxygen Uptake During Exercise and Recovery in Older Patients With Heart Failure With Preserved Ejection Fraction. Journal of Cardiopulmonary Rehabilitation and Prevention. 2020 Jan 2.
- ↑ Lan NS, Lam K, Naylor LH, Green DJ, Minaee NS, Dias P, Maiorana AJ. The Impact of Distinct Exercise Training Modalities on Echocardiographic Measurements in Patients with Heart Failure with Reduced Ejection Fraction. Journal of the American Society of Echocardiography. 2019 Dec 4.
- ↑ MEDICA EM. Group-based cardiac rehabilitation interventions. A challenge for physical and rehabilitation medicine physicians: a randomized controlled trial. European Journal of Physical and Rehabilitation Medicine. 2020 Jan 23.