Hallux Valgus: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Definition<br> == | == Definition<br> == | ||
Hallux valgus is a progressive foot deformity in which the first metatarsophalangeal (MTP) joint is affected and is often accompanied by significant functional disability and foot pain<ref name="Menz">Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)</ref><sup>,</sup><ref name="Nix">Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010, 3:21 (1B)</ref>. This joint is gradually subluxed (lateral deviation of the MTP joint) resulting in an resulting in an abduction of the first metatarsal while the phalanges adduct.<ref name="Menz">Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)</ref>,<ref name="H">Validity of self-assessment of hallux valgus using the Manchester scale, Menz H et al, Musculoskeletal Disorders 2010, 11:215 (1A)</ref>. This often leads to development of soft tissue and bony prominence on the medial side of what is called a bunion <ref name="Glasoe">Hallux Valgus and the First Metatarsal Arch Segment: A Theoretical Biomechanical Perspective. Glasoe W et al, Phys Ther. 2010;90:110–120. (3A)</ref> (exostosis on the dorsomedial aspect of the first metatarsal head <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref> ). At a late stage, these changes lead to pain and functional deficit: i.e. impaired gait (lateral and posterior weight shift, late heel rise, decreased single-limb balance, pronation deformity) <ref name="H">Validity of self-assessment of hallux valgus using the Manchester scale, Menz H et al, Musculoskeletal Disorders 2010, 11:215 (1A)</ref>. There is a high prevalence of hallux valgus in the overall population (23% in adults aged 18-65 years and 35.7% in elderly people aged over 65 years). It has a higher prevalence in women (females 30% - males 13%).and the elderly (35,7%) <ref name="Nix">Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010, 3:21 (1B)</ref>. [[Image:1757-1146-3-21-2.jpg|1x2px]][[Image:1757-1146-3-21-2.jpg|Hallux valgus prevalence in women compared to men]] | Hallux valgus is a progressive foot deformity in which the first metatarsophalangeal (MTP) joint is affected and is often accompanied by significant functional disability and foot pain<ref name="Menz">Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)</ref><sup>,</sup><ref name="Nix">Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010, 3:21 (1B)</ref>. This joint is gradually subluxed (lateral deviation of the MTP joint) resulting in an resulting in an abduction of the first metatarsal while the phalanges adduct.<ref name="Menz">Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)</ref>,<ref name="H">Validity of self-assessment of hallux valgus using the Manchester scale, Menz H et al, Musculoskeletal Disorders 2010, 11:215 (1A)</ref>. This often leads to development of soft tissue and bony prominence on the medial side of what is called a bunion <ref name="Glasoe">Hallux Valgus and the First Metatarsal Arch Segment: A Theoretical Biomechanical Perspective. Glasoe W et al, Phys Ther. 2010;90:110–120. (3A)</ref> (exostosis on the dorsomedial aspect of the first metatarsal head <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref> ). At a late stage, these changes lead to pain and functional deficit: i.e. impaired gait (lateral and posterior weight shift, late heel rise, decreased single-limb balance, pronation deformity) <ref name="H">Validity of self-assessment of hallux valgus using the Manchester scale, Menz H et al, Musculoskeletal Disorders 2010, 11:215 (1A)</ref>. There is a high prevalence of hallux valgus in the overall population (23% in adults aged 18-65 years and 35.7% in elderly people aged over 65 years). It has a higher prevalence in women (females 30% - males 13%).and the elderly (35,7%) <ref name="Nix">Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010, 3:21 (1B)</ref>. [[Image:1757-1146-3-21-2.jpg|1x2px]][[Image:1757-1146-3-21-2.jpg|Hallux valgus prevalence in women compared to men]] | ||
Figure 1: Hallux valgus prevalence in women and men.<ref>Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010 (1a).</ref><br> | Figure 1: Hallux valgus prevalence in women and men.<ref>Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010 (1a).</ref><br> | ||
<br> | <br> | ||
== Clinically Relevant Anatomy<br> == | == Clinically Relevant Anatomy<br> == | ||
The Hallux or first toe, is the medio-distal part of the foot. It is formed by the first metatarsal (articulates with two sesamoid bones), the first proximal phalanx and the first distal phalanx. So the hallux is formed by three bones instead of four, unlike the other toes who have an extra bone called the intermediate phalanx. | The Hallux or first toe, is the medio-distal part of the foot. It is formed by the first metatarsal (articulates with two sesamoid bones), the first proximal phalanx and the first distal phalanx. So the hallux is formed by three bones instead of four, unlike the other toes who have an extra bone called the intermediate phalanx. | ||
The first toe has three synovial joints. The first joint is the art. tarsometatarsae and is situated between the medial cuneïforme bone and the first metatarsal, it does not allow a lot of movement. The second joint, art. metatarsophalangae, connects the first metatarsal and the first proximal phalanx. The joint allows flexion and extension of the first toe and a small ab- and adduction towards the centre of the second toe. It is also reinforced by ligaments (lig. metatarsophalangae collateralia and lig. Metatarsophalangae plantaria). The last joint, art. Interphalangae, is the connection between the two phalanges of the first toe. This joint only allows flexion and extension and it is also reinforced by ligaments (lig. Interphalangae collateralia and lig. Interphalangae plantaris).<br>As mentioned earlier, there are two sesamoid bones that articulate with the first metatarsal bone. These sesamoid bones protect the tendons of the muscles who are attached to them. But their main function is helping those muscles generate more force by extending their levers. | The first toe has three synovial joints. The first joint is the art. tarsometatarsae and is situated between the medial cuneïforme bone and the first metatarsal, it does not allow a lot of movement. The second joint, art. metatarsophalangae, connects the first metatarsal and the first proximal phalanx. The joint allows flexion and extension of the first toe and a small ab- and adduction towards the centre of the second toe. It is also reinforced by ligaments (lig. metatarsophalangae collateralia and lig. Metatarsophalangae plantaria). The last joint, art. Interphalangae, is the connection between the two phalanges of the first toe. This joint only allows flexion and extension and it is also reinforced by ligaments (lig. Interphalangae collateralia and lig. Interphalangae plantaris).<br>As mentioned earlier, there are two sesamoid bones that articulate with the first metatarsal bone. These sesamoid bones protect the tendons of the muscles who are attached to them. But their main function is helping those muscles generate more force by extending their levers. | ||
Other structures: M. tibialis anterior, M. extensor hallucis longus, M. peroneus longus, M. flexor hallucis longus, M.extensor hallucis brevis, M. abductor hallucis, M. flexor hallucis brevis, M. adductor hallucis, M. interossei dorsales I, aponeurosis plantaris, …<ref>SCHÜNKE et al, Prometheus lernatlas der anatomie - allgemeine anatomie und bewegungssystem (tweede druk), Georg Thieme Verlag, Stuttgart, 2005, 600p</ref><ref>Internet, Bunion, (http://emedicine.medscape.com/article/1235796-overview#a11), 2016-11-11.</ref> | Other structures: M. tibialis anterior, M. extensor hallucis longus, M. peroneus longus, M. flexor hallucis longus, M.extensor hallucis brevis, M. abductor hallucis, M. flexor hallucis brevis, M. adductor hallucis, M. interossei dorsales I, aponeurosis plantaris, …<ref>SCHÜNKE et al, Prometheus lernatlas der anatomie - allgemeine anatomie und bewegungssystem (tweede druk), Georg Thieme Verlag, Stuttgart, 2005, 600p</ref><ref>Internet, Bunion, (http://emedicine.medscape.com/article/1235796-overview#a11), 2016-11-11.</ref> | ||
| Line 22: | Line 22: | ||
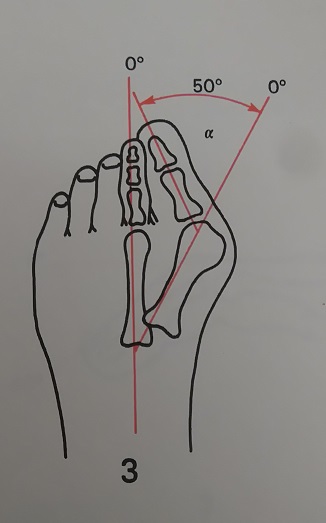
The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal is known as the hallux valgus angle. Less than 15 degrees is considered normal. Angles of 20 degrees and greater are considered abnormal. An angle >45-50 degrees is considered severe.<br> | The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal is known as the hallux valgus angle. Less than 15 degrees is considered normal. Angles of 20 degrees and greater are considered abnormal. An angle >45-50 degrees is considered severe.<br> | ||
== Epidemiology == | == Epidemiology == | ||
The exact etiology is not well established, however, certain factors have been considered to play a role in the development of hallux valgus. Gender(10x more frequent in women), shoewear (tight pointed shoes), congenital deformity or predisposition, chronic achilles tightness, severe flatfoot, hypermobility of the first metatarsocunieform joint, and systemic disease. | The exact etiology is not well established, however, certain factors have been considered to play a role in the development of hallux valgus. Gender(10x more frequent in women), shoewear (tight pointed shoes), congenital deformity or predisposition, chronic achilles tightness, severe flatfoot, hypermobility of the first metatarsocunieform joint, and systemic disease. | ||
Wearing tight shoes Between 20 and 39 years can be crucial for the development of hallux valgus in older people also wearing heels. It’s also possible that abnormal muscle insertions are a partly responsible for a hallux valgus. <br>Hallux valgus is also associated with hip and knee OA and is inversely associated with a higher BMI. <ref>Hannan MT, Menz HB, Jordan JM, Cupples LA, Cheng C-H, Hsu Y-H. Hallux Valgus and Lesser Toe Deformities are Highly Heritable in Adult Men and Women: the Framingham Foot Study. Arthritis care & research. 2013;65(9):1515-1521. doi:10.1002/acr.22040. (Levels of evidence: 2B)</ref><ref>Golightly YM, Hannan MT, Dufour AB, Renner JB, Jordan JM. Factors Associated with Hallux Valgus in a Community-Based Cross-Sectional Study of Adults with and without Osteoarthritis. Arthritis care & research. 2015;67(6):791-798. doi:10.1002/acr.22517. (Levels of evidence: 2A)</ref><ref>Barnish MS, Barnish J. High-heeled shoes and musculoskeletal injuries: a narrative systematic review. BMJ Open. 2016;6(1):e010053. doi:10.1136/bmjopen-2015-010053.</ref><ref>Menz HB, Roddy E, Marshall M, et al. Epidemiology of Shoe Wearing Patterns Over Time in Older Women: Associations With Foot Pain and Hallux Valgus. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2016;71(12):1682-1687. doi:10.1093/gerona/glw004. | Wearing tight shoes Between 20 and 39 years can be crucial for the development of hallux valgus in older people also wearing heels. It’s also possible that abnormal muscle insertions are a partly responsible for a hallux valgus. <br>Hallux valgus is also associated with hip and knee OA and is inversely associated with a higher BMI. <ref>Hannan MT, Menz HB, Jordan JM, Cupples LA, Cheng C-H, Hsu Y-H. Hallux Valgus and Lesser Toe Deformities are Highly Heritable in Adult Men and Women: the Framingham Foot Study. Arthritis care &amp; research. 2013;65(9):1515-1521. doi:10.1002/acr.22040. (Levels of evidence: 2B)</ref><ref>Golightly YM, Hannan MT, Dufour AB, Renner JB, Jordan JM. Factors Associated with Hallux Valgus in a Community-Based Cross-Sectional Study of Adults with and without Osteoarthritis. Arthritis care &amp; research. 2015;67(6):791-798. doi:10.1002/acr.22517. (Levels of evidence: 2A)</ref><ref>Barnish MS, Barnish J. High-heeled shoes and musculoskeletal injuries: a narrative systematic review. BMJ Open. 2016;6(1):e010053. doi:10.1136/bmjopen-2015-010053.</ref><ref>Menz HB, Roddy E, Marshall M, et al. Epidemiology of Shoe Wearing Patterns Over Time in Older Women: Associations With Foot Pain and Hallux Valgus. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2016;71(12):1682-1687. doi:10.1093/gerona/glw004.fckLR(Levels of evidence: 3)</ref><ref>MOL, W. et STRIKWERDA, R., Compendium orthopedie, De tijdstroom, Lochum, 1977, 343p. (p.232-234).</ref> | ||
(Levels of evidence: 3)</ref><ref>MOL, W. et STRIKWERDA, R., Compendium orthopedie, De tijdstroom, Lochum, 1977, 343p. (p.232-234).</ref> | |||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
| Line 35: | Line 34: | ||
== Clinical Presentation == | == Clinical Presentation == | ||
In this foot deformity, the medial eminence becomes prominent as the distal end of the first metatarsal drift medially and the proximal phalanx deviates laterally. The first MTP becomes subluxed, what leads to a lateral deviation of the hallux, medial displacement of the distal end of the first metatarsal and bony enlargement of the first metatarsal head <ref name="Menz">Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)</ref>. | In this foot deformity, the medial eminence becomes prominent as the distal end of the first metatarsal drift medially and the proximal phalanx deviates laterally. The first MTP becomes subluxed, what leads to a lateral deviation of the hallux, medial displacement of the distal end of the first metatarsal and bony enlargement of the first metatarsal head <ref name="Menz">Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)</ref>. | ||
The mechanism behind this hallux valgus formation starts with the stretching of the abductor hallucis muscle (for example as a result of wearing tight shoes). The base of the first proximal phalanx starts to lateralise and abducts. When we walk the forefoot is turned in a pronation, which stretches the medial collateral ligament and the capsular structures of the first MTP joint. As the first MTP joint consists of multiple bones, ligaments, sesamoid bones and has muscles nearby, structures influence other structures as they move or stretch. That way, once a threshold degree of valgus of the first PP is reached, the first metatarsal bone starts his way into a varus position. This way, the hallux is pushed into a valgus position. The capsule gets weaker and the abductor hallucis tendon turns into a flexor of the hallux. As it turns worse, multiple muscles tend to worsen the situation as their axis of pull is lateralized. <br>As a bunion appears, friction is raised when shoes are worn. There may be an irritation of the MCL ligament of the first MTP joint, which leads to inflammation and calcification of the joint. This worsens the pain and bunion size. [18] [19] [31] | The mechanism behind this hallux valgus formation starts with the stretching of the abductor hallucis muscle (for example as a result of wearing tight shoes). The base of the first proximal phalanx starts to lateralise and abducts. When we walk the forefoot is turned in a pronation, which stretches the medial collateral ligament and the capsular structures of the first MTP joint. As the first MTP joint consists of multiple bones, ligaments, sesamoid bones and has muscles nearby, structures influence other structures as they move or stretch. That way, once a threshold degree of valgus of the first PP is reached, the first metatarsal bone starts his way into a varus position. This way, the hallux is pushed into a valgus position. The capsule gets weaker and the abductor hallucis tendon turns into a flexor of the hallux. As it turns worse, multiple muscles tend to worsen the situation as their axis of pull is lateralized. <br>As a bunion appears, friction is raised when shoes are worn. There may be an irritation of the MCL ligament of the first MTP joint, which leads to inflammation and calcification of the joint. This worsens the pain and bunion size. [18] [19] [31] | ||
In an early stage, this leads to the tenderness of the bunion due to shoewear. The skin over the bunion is hard, warm and red. Later on the patient may have other complaints due to osteoarthritis. The bunion keeps moving medially and the pain gets worse.[33]<br><br> | In an early stage, this leads to the tenderness of the bunion due to shoewear. The skin over the bunion is hard, warm and red. Later on the patient may have other complaints due to osteoarthritis. The bunion keeps moving medially and the pain gets worse.[33]<br><br> | ||
| Line 59: | Line 58: | ||
*Pain (primary symptom) <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref> | *Pain (primary symptom) <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref> | ||
<br> | |||
<br>[[Image:Hallux valgus angle 2.jpg|center]] Figure 4: Hallux valgus angle 𝝰: between the axis of the os metatarsale I (MT I) and the proximal phalanx I (PP I).<ref>RUSSE, O., et al, Orthopedisch onderzoek, De tijdstroom, Lochem, 1977.</ref><br> | |||
<br>[[Image: | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
| Line 73: | Line 72: | ||
=== Non-operative treatment === | === Non-operative treatment === | ||
Prevention:<br>A hereditary factor or predisposition (for example as a result of a generalized ligamentous laxity) is not preventable, but other things are. For example wearing shoes that fit properly and are not too tight or high heels, can be an important factor in preventing hallux valgus.<ref>Coşkun G, Talu B, Bek N, et al. Effects of hallux valgus deformity on rear foot position, pain, function, and quality of life of women. J Phys Ther Sci 2016; 28:781–787. | Prevention:<br>A hereditary factor or predisposition (for example as a result of a generalized ligamentous laxity) is not preventable, but other things are. For example wearing shoes that fit properly and are not too tight or high heels, can be an important factor in preventing hallux valgus.<ref>Coşkun G, Talu B, Bek N, et al. Effects of hallux valgus deformity on rear foot position, pain, function, and quality of life of women. J Phys Ther Sci 2016; 28:781–787. fckLR(Levels of evidence: 2C)</ref> | ||
(Levels of evidence: 2C)</ref> | |||
The first treatment option is non operative care:<br> | The first treatment option is non operative care:<br> | ||
| Line 83: | Line 81: | ||
<br> | <br> | ||
<span style="line-height: 1.5em; font-size: 13.28px;"> </span>[[Image:Toe-splint-darco1.jpg|250x250px]]<span style="line-height: 1.5em; font-size: 13.28px;"> </span>[[Image:Hallux valgus1.jpg|250x250px]]<span style="line-height: 1.5em; font-size: 13.28px;"> </span><span style="line-height: 1.5em; font-size: 13.28px;"> </span><span style="line-height: 1.5em; font-size: 13.28px;"> '''Figure 5 & 6''': Examples of toe splints that are used for the treatment of patients with hallux valgus.</span> | <span style="line-height: 1.5em; font-size: 13.28px;"> </span>[[Image:Toe-splint-darco1.jpg|250x250px]]<span style="line-height: 1.5em; font-size: 13.28px;"> </span>[[Image:Hallux valgus1.jpg|250x250px]]<span style="line-height: 1.5em; font-size: 13.28px;"> </span><span style="line-height: 1.5em; font-size: 13.28px;"> </span><span style="line-height: 1.5em; font-size: 13.28px;"> '''Figure 5 & 6''': Examples of toe splints that are used for the treatment of patients with hallux valgus.</span> | ||
*Achilles tendon contracture may require stretching or even lengthening <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref> | *Achilles tendon contracture may require stretching or even lengthening <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref> | ||
This type of treatment can be applied in the early stage when the secondary contractures of the soft tissues and the alterations of the articular surfaces have not become permanent <ref name="Day">Hallux valgus. F. DAY, M.D., Canad. M. A. J. April 16, 1957, vol. 76 (5)</ref>. | This type of treatment can be applied in the early stage when the secondary contractures of the soft tissues and the alterations of the articular surfaces have not become permanent <ref name="Day">Hallux valgus. F. DAY, M.D., Canad. M. A. J. April 16, 1957, vol. 76 (5)</ref>. | ||
=== Operative treatment === | |||
If non-operative treatment fails surgery could be considered <ref name="T">Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)</ref>. <br>There are several surgical procedures that we can apply depending on the severity of the injury:<br> | |||
*For mild cases: distal soft tissue procedure | |||
*Hallux angle < 30 °: Chevron osteotomy | |||
*Hallux < 25 °: Akin procedure | |||
*Age > 65 year: Keller arthoplasty | |||
*Arhrodesis (the most common)<br> | |||
As a result of the gait disturbances (see non-operative treatment), objectives for physical therapy could be:<br> | |||
*Adjusted footwear with wider and deeper tip | |||
*Increase extension of MTP joint | |||
*Relieve weight-bearing stresses (orthosis) <ref name="Dimonte">Pathomechanics, Gait Deviations, and Treatment of the Rheumatoid Foot: a clinical report. Dimonte P et al. Physical therapy 1982: Vol 62(8): 1148 – 1156 (5)</ref> | |||
*<u>Sesamoid Mobilization</u>:*The physical therapist performs grade III joint mobilizations on the medial and lateral sesamoid of the affected first MPJ. He / she places 1 thumb on the proximal aspect of the sesamoid en applies a force from proximal to distal that causes the sesamoid to reach the end range of motion = distal glides. These are performed with large-amplitude rhythmic oscillations. No greater than 20° of movement of the MPJ is allowed during the technique.<sup><ref name="J">The effects of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. Shamus J, Shamus E, Gugel RN, et al. J Orthop Sports Phys Ther. 2004;80:769–780. 2B</ref></sup> | |||
*Strengthening of the M. Peroneus Longus <ref name="Schuh">Rehabilitation after hallux valgus surgery: importance of physical therapy to restore weight bearing of the first ray during the stance phase. Schuh R, Hofstaetter SG, Adams SB Jr, et al. Phys Ther. 2009;89:934–945. (2C)</ref> | |||
*Gait Training <ref name="J">The effects of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. Shamus J, Shamus E, Gugel RN, et al. J Orthop Sports Phys Ther. 2004;80:769–780. 2B</ref>. During gait training, we can train the different phases: | |||
= | #Stance phase: could be trained by performing a heel-strike in its physiological position at the lateral aspect of the heel. | ||
#Stance phase could be followed by weight bearing of the first metatarsal during midstance and terminal stance, with training of active push-off by the hallux flexors, the flexor digitorum longus and brevis muscles, and the lumbrical muscles <ref name="Schuh">Rehabilitation after hallux valgus surgery: importance of physical therapy to restore weight bearing of the first ray during the stance phase. Schuh R, Hofstaetter SG, Adams SB Jr, et al. Phys Ther. 2009;89:934–945. (2C)</ref><br>During gait training, verbal cues could be provided . | |||
These objectives should ensure that pain is reduced and function is restored. <ref name="J">The effects of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. Shamus J, Shamus E, Gugel RN, et al. J Orthop Sports Phys Ther. 2004;80:769–780. 2B</ref><br>Physiotherapists should contain an expanded program, including whirlpool, [http://www.physio-pedia.com/index.php?title=Ultrasound_therapy ultrasound], ice, [http://www.physio-pedia.com/index.php/Transcutaneous_Electrical_Nerve_Stimulation_(TENS) electrical stimulation,] MTJ mobilizations and exercises. This is more effective than a physical therapy alone. The combination will result in a increase in ROM MTP joint, strength and function and also a decrease in pain <ref name="J">The effects of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. Shamus J, Shamus E, Gugel RN, et al. J Orthop Sports Phys Ther. 2004;80:769–780. 2B</ref>. | |||
<div><br></div> | |||
=== Post operative physical therapy === | |||
Post -op Rehabiliatation Considerations <br>For all surgical procedures, the patient is allowed to ambulate in a post-operative shoe immedidately after surgery.<br>Patients come out of surgery needing to wear a post-op shoe and compressive dressings for 8 weeks<br>Long term follow up has shown equally positive outcomes after Chevron osteotomy for both patients both younger and older than 50. | |||
<br> | |||
== Physical therapy management == | == Physical therapy management == | ||
'''PHASE I - Pain Relief. Minimise Swelling & Injury Protection<ref name="1">http://physioworks.com.au/injuries-conditions-1/foot-bunion</ref>''' | '''PHASE I - Pain Relief. Minimise Swelling & Injury Protection<ref name="1">http://physioworks.com.au/injuries-conditions-1/foot-bunion</ref>''' | ||
| Line 111: | Line 133: | ||
As your pain and inflammation settles, your physiotherapist will turn their attention to restoring your normal toe and foot joint range of motion and muscle length. | As your pain and inflammation settles, your physiotherapist will turn their attention to restoring your normal toe and foot joint range of motion and muscle length. | ||
Treatment may include joint mobilisation (abduction and flexion)and alignment techniques (between the first and the second metatarsal), massage, muscle and joint stretches, taping, a bunion splint or orthotic. Bunion stretch and soft tissue release. (see reference for video)<ref>Internet, Youtube: Bunion stretch and soft tissue release; 2012-08-01, (https://www.youtube.com/watch?v=q5Ov6LMISvU)</ref> | Treatment may include joint mobilisation (abduction and flexion)and alignment techniques (between the first and the second metatarsal), massage, muscle and joint stretches, taping, a bunion splint or orthotic. Bunion stretch and soft tissue release. (see reference for video)<ref>Internet, Youtube: Bunion stretch and soft tissue release; 2012-08-01, (https://www.youtube.com/watch?v=q5Ov6LMISvU)</ref> | ||
'''PHASE III - Restore Normal Muscle Control & Strength<ref name="1">http://physioworks.com.au/injuries-conditions-1/foot-bunion</ref>''' | '''PHASE III - Restore Normal Muscle Control & Strength<ref name="1">http://physioworks.com.au/injuries-conditions-1/foot-bunion</ref>''' | ||
a Foot Posture Correction Program to assist you to regain your normal foot posture. | a Foot Posture Correction Program to assist you to regain your normal foot posture. | ||
| Line 121: | Line 143: | ||
'''Ankle Dorsiflexion with Band<ref name="2">http://www.everydayhealth.com/foot-health/8-foot-exercises-for-bunions.aspx</ref>''' | '''Ankle Dorsiflexion with Band<ref name="2">http://www.everydayhealth.com/foot-health/8-foot-exercises-for-bunions.aspx</ref>''' | ||
[[Image: | [[Image:Elastic band dorsiflexion.jpg|left]]The ankle dorsiflexion exercise strengthens the ankles and lower leg muscles.Sit on the floor with your legs straight to begin. Place your hands on the floor at your sides and use your arms to hold your back straight. Place the center of the band on the top of your forefoot with your toes slightly pointed. Have a friend sit on the floor in front of you and hold the ends of the band at floor level. Next, pull your toes away from your friend and the ends of the band. You should get resistance from the band if your workout partner is holding it tight. Point your toes slightly to complete an ankle dorsiflexion. | ||
<br> | |||
<br> | |||
'''Figure 7''': Ankle dorsiflexion with an elastic band<ref>(https://myhealth.alberta.ca/Health/aftercareinformation/_layouts/15/healthwise/media/medical/hw/h9991695_001_1_pi.jpg)</ref><br> | |||
'''Figure 7''': Ankle dorsiflexion with an elastic band<ref>(https://myhealth.alberta.ca/Health/aftercareinformation/_layouts/15/healthwise/media/medical/hw/h9991695_001_1_pi.jpg)</ref><br> | |||
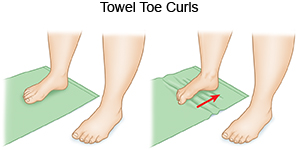
'''Towel curls.''' You can strengthen your toes by spreading out a small towel on the floor, curling your toes around it, and pulling it toward you. Repeat five times. Khan says that gripping objects with your toes like this can help keep your foot flexible.<ref>http://www.everydayhealth.com/foot-health/8-foot-exercises-for-bunions.aspx</ref> | '''Towel curls.''' You can strengthen your toes by spreading out a small towel on the floor, curling your toes around it, and pulling it toward you. Repeat five times. Khan says that gripping objects with your toes like this can help keep your foot flexible.<ref>http://www.everydayhealth.com/foot-health/8-foot-exercises-for-bunions.aspx</ref> | ||
[[Image: | [[Image:Towel toe curl.jpg|center]] | ||
'''Figure 8''': Toe curl exercise using a towel<ref>https://www.allinahealth.org/mdex/en3092088.jpg | '''Figure 8''': Toe curl exercise using a towel<ref>https://www.allinahealth.org/mdex/en3092088.jpg</ref> | ||
'''Toes spread out (TSO)'''. A possible causative factor of the hallux valgus is the muscle imbalance between the abductor hallucis and the adductor hallucis. Strengthening the abductor muscle can prevent a hallux valgus and can be helpful to correct the deformity in an early stage. The toes-spread-out (TSO) exercise is an efficient way to train your abductor hallucis. <ref>KIM, M; et al. Comparison of muscle activities of abductor hallucis and adductor hallucis between the short foot and toe-spread-out exercises in subjects with mild hallux valgus. Journal of Back &amp; Musculoskeletal Rehabilitation. 26, 2, 163-168, Apr. 2013 fckLR(levels of evidence: 1C)</ref> | |||
<br> | |||
'''PHASE IV - Restoring Full Function''' | '''PHASE IV - Restoring Full Function''' | ||
| Line 150: | Line 171: | ||
In addition to your muscle control, your physiotherapist will assess your foot biomechanics and may recommend either a temporary off-the shelf orthotic or refer you to a podiatrist for custom made orthotics. You should avoid wearing high heel shoes and shoes with tight or angular toe boxes. | In addition to your muscle control, your physiotherapist will assess your foot biomechanics and may recommend either a temporary off-the shelf orthotic or refer you to a podiatrist for custom made orthotics. You should avoid wearing high heel shoes and shoes with tight or angular toe boxes. | ||
<br> | |||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
| Line 180: | Line 177: | ||
Hallux valgus<br>Other forms of arthritis<br>Surgical or traumatic arthropathy<ref>http://patient.info/doctor/hallux-rigidus</ref><br> | Hallux valgus<br>Other forms of arthritis<br>Surgical or traumatic arthropathy<ref>http://patient.info/doctor/hallux-rigidus</ref><br> | ||
Hallux valgus can be confused with other diseases or injuries during diagnosis.<br>In an early stage the redness and pain that go with the early stage of hallux valgus can be confused with an inflammation, infection or gout of the hallux joints. More specifically the first MTP joint. (Phyiopedia “Gout” : https://www.physio-pedia.com/Gout )<br>Gout: pain as a symptom of gout can be confused with a hallux valgus. Difference between them is the fact that gout suddenly appears and Hallux valgus gradually appears. To make sure it is a gout, the semi uric acid level can be determined, as it is raises in patients with gout. <br>Other forms of arthritis and their consequences for example hallux rigidus can be confused with hallux valgus as well as being a result of the deformity. For example a septic arthritis joint also shows a red and swollen joint. (Physio-pedia page “Hallux rigidus”: http://www.physio-pedia.com/Hallux_Rigidus) <br>Turf toe: pain and swelling due to turf toe can be confused with a hallux valgus presence. <ref>SOBEL, E., Hallux valgus, assessment and conservative management and the role of faulty footwear, October 2001, (http://podiatrym.com/cme/oct01.pdf).</ref><ref>Internet, Gout, 2016-12-08, (http://www.webmd.com/arthritis/tc/gout-topic-overview#1)</ref><ref>Ashman CJ, Klecker RJ, Yu JS (2001) Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. Radiographies 21:1425–1440.</ref><ref>Jeremy J., McCormick, MD, Robert B. Anderson, MD -Turf Toe: Anatomy, Diagnosis, and Treatment, Clin Sports Med. 2010 Apr;29(2):313-23 | Hallux valgus can be confused with other diseases or injuries during diagnosis.<br>In an early stage the redness and pain that go with the early stage of hallux valgus can be confused with an inflammation, infection or gout of the hallux joints. More specifically the first MTP joint. (Phyiopedia “Gout” : https://www.physio-pedia.com/Gout )<br>Gout: pain as a symptom of gout can be confused with a hallux valgus. Difference between them is the fact that gout suddenly appears and Hallux valgus gradually appears. To make sure it is a gout, the semi uric acid level can be determined, as it is raises in patients with gout. <br>Other forms of arthritis and their consequences for example hallux rigidus can be confused with hallux valgus as well as being a result of the deformity. For example a septic arthritis joint also shows a red and swollen joint. (Physio-pedia page “Hallux rigidus”: http://www.physio-pedia.com/Hallux_Rigidus) <br>Turf toe: pain and swelling due to turf toe can be confused with a hallux valgus presence. <ref>SOBEL, E., Hallux valgus, assessment and conservative management and the role of faulty footwear, October 2001, (http://podiatrym.com/cme/oct01.pdf).</ref><ref>Internet, Gout, 2016-12-08, (http://www.webmd.com/arthritis/tc/gout-topic-overview#1)</ref><ref>Ashman CJ, Klecker RJ, Yu JS (2001) Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. Radiographies 21:1425–1440.</ref><ref>Jeremy J., McCormick, MD, Robert B. Anderson, MD -Turf Toe: Anatomy, Diagnosis, and Treatment, Clin Sports Med. 2010 Apr;29(2):313-23 fckLR(Levels of evidence : A)</ref><ref>MCRAE, R., Clinical Orthopaedic Examination, Churchill Livingstone, Edinburgh, 2010, 323p (p.236-238).</ref> | ||
(Levels of evidence : A)</ref><ref>MCRAE, R., Clinical Orthopaedic Examination, Churchill Livingstone, Edinburgh, 2010, 323p (p.236-238).</ref> | |||
== Key Evidence == | == Key Evidence == | ||
Revision as of 13:53, 23 December 2016
Original Editors - Bradley Svoboda
Top Contributors - Laura Ritchie, Van Horebeek Erika, Mariam Hashem, Ewa Jaraczewska, Lucinda hampton, Andeela Hafeez, Jolien Rottie, Rachael Lowe, Jess Bell, Bradley Svoboda, Kim Jackson, Admin, Morgane Michiels, 127.0.0.1, Kristin Zumo, Khloud Shreif, Tarina van der Stockt, WikiSysop, Tinne Tielemans, Wanda van Niekerk and Evan Thomas
Definition
[edit | edit source]
Hallux valgus is a progressive foot deformity in which the first metatarsophalangeal (MTP) joint is affected and is often accompanied by significant functional disability and foot pain[1],[2]. This joint is gradually subluxed (lateral deviation of the MTP joint) resulting in an resulting in an abduction of the first metatarsal while the phalanges adduct.[1],[3]. This often leads to development of soft tissue and bony prominence on the medial side of what is called a bunion [4] (exostosis on the dorsomedial aspect of the first metatarsal head [5] ). At a late stage, these changes lead to pain and functional deficit: i.e. impaired gait (lateral and posterior weight shift, late heel rise, decreased single-limb balance, pronation deformity) [3]. There is a high prevalence of hallux valgus in the overall population (23% in adults aged 18-65 years and 35.7% in elderly people aged over 65 years). It has a higher prevalence in women (females 30% - males 13%).and the elderly (35,7%) [2]. ![]()
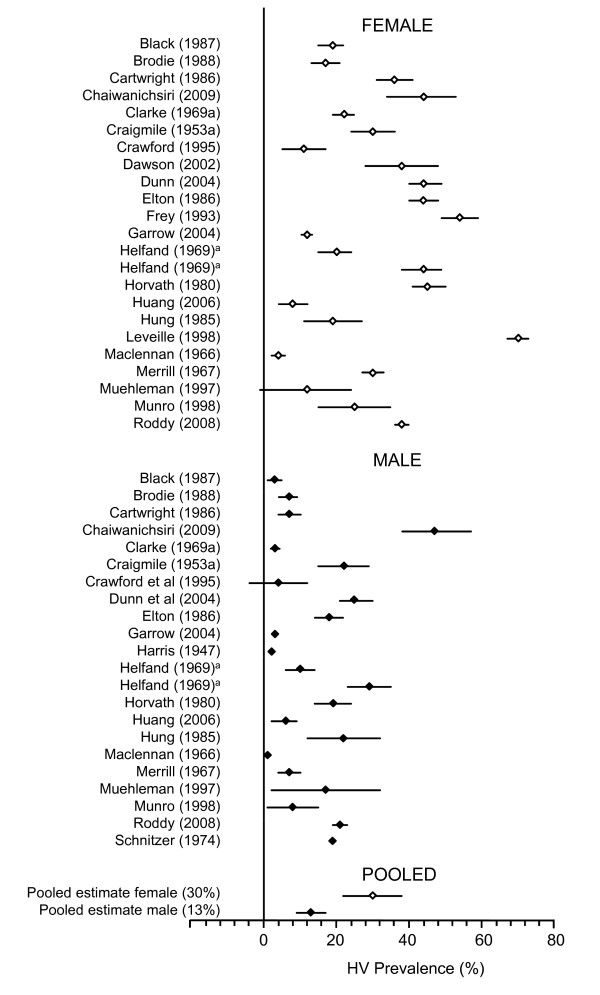
Figure 1: Hallux valgus prevalence in women and men.[6]
Clinically Relevant Anatomy
[edit | edit source]
The Hallux or first toe, is the medio-distal part of the foot. It is formed by the first metatarsal (articulates with two sesamoid bones), the first proximal phalanx and the first distal phalanx. So the hallux is formed by three bones instead of four, unlike the other toes who have an extra bone called the intermediate phalanx.
The first toe has three synovial joints. The first joint is the art. tarsometatarsae and is situated between the medial cuneïforme bone and the first metatarsal, it does not allow a lot of movement. The second joint, art. metatarsophalangae, connects the first metatarsal and the first proximal phalanx. The joint allows flexion and extension of the first toe and a small ab- and adduction towards the centre of the second toe. It is also reinforced by ligaments (lig. metatarsophalangae collateralia and lig. Metatarsophalangae plantaria). The last joint, art. Interphalangae, is the connection between the two phalanges of the first toe. This joint only allows flexion and extension and it is also reinforced by ligaments (lig. Interphalangae collateralia and lig. Interphalangae plantaris).
As mentioned earlier, there are two sesamoid bones that articulate with the first metatarsal bone. These sesamoid bones protect the tendons of the muscles who are attached to them. But their main function is helping those muscles generate more force by extending their levers.
Other structures: M. tibialis anterior, M. extensor hallucis longus, M. peroneus longus, M. flexor hallucis longus, M.extensor hallucis brevis, M. abductor hallucis, M. flexor hallucis brevis, M. adductor hallucis, M. interossei dorsales I, aponeurosis plantaris, …[7][8]
The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal is known as the hallux valgus angle. Less than 15 degrees is considered normal. Angles of 20 degrees and greater are considered abnormal. An angle >45-50 degrees is considered severe.
Epidemiology[edit | edit source]
The exact etiology is not well established, however, certain factors have been considered to play a role in the development of hallux valgus. Gender(10x more frequent in women), shoewear (tight pointed shoes), congenital deformity or predisposition, chronic achilles tightness, severe flatfoot, hypermobility of the first metatarsocunieform joint, and systemic disease.
Wearing tight shoes Between 20 and 39 years can be crucial for the development of hallux valgus in older people also wearing heels. It’s also possible that abnormal muscle insertions are a partly responsible for a hallux valgus.
Hallux valgus is also associated with hip and knee OA and is inversely associated with a higher BMI. [9][10][11][12][13]
Mechanism of Injury / Pathological Process
[edit | edit source]
The exact etiology is not well established, however, certain factors have been considered to play a role in the development of hallux valgus. Gender(10x more frequent in women), shoewear (tight pointed shoes), congenital deformity or predisposition, chronic achilles tightness, severe flatfoot, hypermobility of the first metatarsocunieform joint, and systemic disease.
Clinical Presentation[edit | edit source]
In this foot deformity, the medial eminence becomes prominent as the distal end of the first metatarsal drift medially and the proximal phalanx deviates laterally. The first MTP becomes subluxed, what leads to a lateral deviation of the hallux, medial displacement of the distal end of the first metatarsal and bony enlargement of the first metatarsal head [1].
The mechanism behind this hallux valgus formation starts with the stretching of the abductor hallucis muscle (for example as a result of wearing tight shoes). The base of the first proximal phalanx starts to lateralise and abducts. When we walk the forefoot is turned in a pronation, which stretches the medial collateral ligament and the capsular structures of the first MTP joint. As the first MTP joint consists of multiple bones, ligaments, sesamoid bones and has muscles nearby, structures influence other structures as they move or stretch. That way, once a threshold degree of valgus of the first PP is reached, the first metatarsal bone starts his way into a varus position. This way, the hallux is pushed into a valgus position. The capsule gets weaker and the abductor hallucis tendon turns into a flexor of the hallux. As it turns worse, multiple muscles tend to worsen the situation as their axis of pull is lateralized.
As a bunion appears, friction is raised when shoes are worn. There may be an irritation of the MCL ligament of the first MTP joint, which leads to inflammation and calcification of the joint. This worsens the pain and bunion size. [18] [19] [31]
In an early stage, this leads to the tenderness of the bunion due to shoewear. The skin over the bunion is hard, warm and red. Later on the patient may have other complaints due to osteoarthritis. The bunion keeps moving medially and the pain gets worse.[33]
Figure 3: Hallux valgus is a disruption of the normal alignment of the metatarsophalangeal joint. The hallux abducts while the first metatarsocuneiform segments adduct. The severity of the hallux deformity is measured by (A) hallux valgus angle and (B) intermetatarsal 1-2 angle [4]
A common problem in people with hallux valgus (pre-operative), is one or more disorders in their gait pattern due to the deformity of the first metatarsophalangeal joint. Dysfunctions that may be present:
- Gait deviations in the midstance (middle stage) and the propulsion phase (late stance). As the body weight moves forward on a foot on the ground, the patient will tend to keep his weight on the lateral border of the foot. This leads to a lateral and posterior weight shift
- Patient has also a pronation deformity
- Patient is unable to supinate his / her foot and will tend to keep his body weight on the lateral border of the foot which results in a late heel rise
- The period of single-limb support will be diminished [14]
When a physical examination is executed, the following indications could be present:
- Lateral deviation of the MTP joint
- Swelling of first MTP joint
- Shortening of flexor hallucis brevis muscle
- Tenderness of hallux
- Weakness of hallux abductor muscles [14]
- Pain (primary symptom) [5]
Figure 4: Hallux valgus angle 𝝰: between the axis of the os metatarsale I (MT I) and the proximal phalanx I (PP I).[15]
Diagnostic Procedures[edit | edit source]
One of the procedures to determine hallux valgus is the use of radiographs. Here we look at the hallux abductus angle. This is the angle formed between the longitudinal bisections of the first metatarsal and the proximal phalanx. When we have an angle less than 15°, there is no sign of hallux valgus. If the angle is greater than 15°, there is a sign of hallux valgus. An angle of 45-50 ° is considered serious. The degree of displacement of the sesamoids and the level of osteoarthritic change within the first MTP joint should be considered as well.[1]
It is not always possible or necessary to take radiographs to determine the severity of hallux valgus. Therefore, they developed a scale, called the Manchester scale [1].The Manchester scale consists of standardized photographs of four types of hallux valgus: none, mild, moderate and severe. Research has shown that this test is reliable in terms of both re-test and inter-tester reliability (kappa values of 0.77 and 0.86). In the study by Roddy et al (2007) [16], they have developed a tool that exists of 5 photographs, instead of 4 photographs which is the case in the Manchester scale. Each photograph had a hallux valgus angle increased with 15 °. This tool had a good retest reliability (kappa = 0.82) and is also a good tool to use to determine hallux valgus severity [16]. So we can use both scales (the four-level classification or dichotomised scale) to determine the severity of hallux valgus [3].
Physical examination should be performed with the patient both seated and standing. During weight bearing, the deformity is generally accentuated. During examination, the presence of pes planus and contracture of the Achilles tendon should be evaluated. The height of the longitudinal arch and hallux, with its relation to the lesser toes, are also examined [5].
Management / Interventions
[edit | edit source]
Non-operative treatment[edit | edit source]
Prevention:
A hereditary factor or predisposition (for example as a result of a generalized ligamentous laxity) is not preventable, but other things are. For example wearing shoes that fit properly and are not too tight or high heels, can be an important factor in preventing hallux valgus.[17]
The first treatment option is non operative care:
- Adjustment to footwear help in eliminating friction at the level of the medial eminence (bunion), e.g., patients should be provided of a shoe with a wider and deeper tip
- The condition of pes planus may be helped by an orthosis. A sever pes planus condition can lead to a recurrence of hallux valgus following surgery.

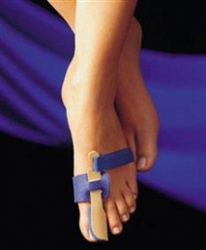 Figure 5 & 6: Examples of toe splints that are used for the treatment of patients with hallux valgus.
Figure 5 & 6: Examples of toe splints that are used for the treatment of patients with hallux valgus.
- Achilles tendon contracture may require stretching or even lengthening [5]
This type of treatment can be applied in the early stage when the secondary contractures of the soft tissues and the alterations of the articular surfaces have not become permanent [18].
Operative treatment[edit | edit source]
If non-operative treatment fails surgery could be considered [5].
There are several surgical procedures that we can apply depending on the severity of the injury:
- For mild cases: distal soft tissue procedure
- Hallux angle < 30 °: Chevron osteotomy
- Hallux < 25 °: Akin procedure
- Age > 65 year: Keller arthoplasty
- Arhrodesis (the most common)
As a result of the gait disturbances (see non-operative treatment), objectives for physical therapy could be:
- Adjusted footwear with wider and deeper tip
- Increase extension of MTP joint
- Relieve weight-bearing stresses (orthosis) [14]
- Sesamoid Mobilization:*The physical therapist performs grade III joint mobilizations on the medial and lateral sesamoid of the affected first MPJ. He / she places 1 thumb on the proximal aspect of the sesamoid en applies a force from proximal to distal that causes the sesamoid to reach the end range of motion = distal glides. These are performed with large-amplitude rhythmic oscillations. No greater than 20° of movement of the MPJ is allowed during the technique.[19]
- Strengthening of the M. Peroneus Longus [20]
- Gait Training [19]. During gait training, we can train the different phases:
- Stance phase: could be trained by performing a heel-strike in its physiological position at the lateral aspect of the heel.
- Stance phase could be followed by weight bearing of the first metatarsal during midstance and terminal stance, with training of active push-off by the hallux flexors, the flexor digitorum longus and brevis muscles, and the lumbrical muscles [20]
During gait training, verbal cues could be provided .
These objectives should ensure that pain is reduced and function is restored. [19]
Physiotherapists should contain an expanded program, including whirlpool, ultrasound, ice, electrical stimulation, MTJ mobilizations and exercises. This is more effective than a physical therapy alone. The combination will result in a increase in ROM MTP joint, strength and function and also a decrease in pain [19].
Post operative physical therapy[edit | edit source]
Post -op Rehabiliatation Considerations
For all surgical procedures, the patient is allowed to ambulate in a post-operative shoe immedidately after surgery.
Patients come out of surgery needing to wear a post-op shoe and compressive dressings for 8 weeks
Long term follow up has shown equally positive outcomes after Chevron osteotomy for both patients both younger and older than 50.
Physical therapy management[edit | edit source]
PHASE I - Pain Relief. Minimise Swelling & Injury ProtectionCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Pain is the main reason that you seek treatment for bunion. Analgesics may help.
Inflammation it best eased via ice therapy and techniques or exercises that deload the inflammed structures. Anti-inflammatory medications may help.
Your physiotherapist will use an array of treatment tools to reduce your pain and inflammation.
These include: ice, electrotherapy, acupuncture, deloading taping techniques, soft tissue massage and orthotics to off-load the bunion.
PHASE II - Restoring Normal ROM & PostureCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
As your pain and inflammation settles, your physiotherapist will turn their attention to restoring your normal toe and foot joint range of motion and muscle length.
Treatment may include joint mobilisation (abduction and flexion)and alignment techniques (between the first and the second metatarsal), massage, muscle and joint stretches, taping, a bunion splint or orthotic. Bunion stretch and soft tissue release. (see reference for video)[21]
PHASE III - Restore Normal Muscle Control & StrengthCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
a Foot Posture Correction Program to assist you to regain your normal foot posture.
Strengthing exercise:
Ankle Dorsiflexion with BandCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
The ankle dorsiflexion exercise strengthens the ankles and lower leg muscles.Sit on the floor with your legs straight to begin. Place your hands on the floor at your sides and use your arms to hold your back straight. Place the center of the band on the top of your forefoot with your toes slightly pointed. Have a friend sit on the floor in front of you and hold the ends of the band at floor level. Next, pull your toes away from your friend and the ends of the band. You should get resistance from the band if your workout partner is holding it tight. Point your toes slightly to complete an ankle dorsiflexion.
Figure 7: Ankle dorsiflexion with an elastic band[22]
Towel curls. You can strengthen your toes by spreading out a small towel on the floor, curling your toes around it, and pulling it toward you. Repeat five times. Khan says that gripping objects with your toes like this can help keep your foot flexible.[23]
Figure 8: Toe curl exercise using a towel[24]
Toes spread out (TSO). A possible causative factor of the hallux valgus is the muscle imbalance between the abductor hallucis and the adductor hallucis. Strengthening the abductor muscle can prevent a hallux valgus and can be helpful to correct the deformity in an early stage. The toes-spread-out (TSO) exercise is an efficient way to train your abductor hallucis. [25]
PHASE IV - Restoring Full Function
During this stage of your rehabilitation is aimed at returning you to your desired activities. Everyone has different demands for their feet that will determine what specific treatment goals you need to achieve. For some it be simply to walk around the block. Others may wish to run a marathon or return to a labour-intensive activity.
PHASE V - Preventing a Recurrence
Bunions will deform further with no attention. Plus, the bunion pain associated does have a tendency to return. The main reason is biomechanical.
In addition to your muscle control, your physiotherapist will assess your foot biomechanics and may recommend either a temporary off-the shelf orthotic or refer you to a podiatrist for custom made orthotics. You should avoid wearing high heel shoes and shoes with tight or angular toe boxes.
Differential Diagnosis
[edit | edit source]
Hallux valgus
Other forms of arthritis
Surgical or traumatic arthropathy[26]
Hallux valgus can be confused with other diseases or injuries during diagnosis.
In an early stage the redness and pain that go with the early stage of hallux valgus can be confused with an inflammation, infection or gout of the hallux joints. More specifically the first MTP joint. (Phyiopedia “Gout” : https://www.physio-pedia.com/Gout )
Gout: pain as a symptom of gout can be confused with a hallux valgus. Difference between them is the fact that gout suddenly appears and Hallux valgus gradually appears. To make sure it is a gout, the semi uric acid level can be determined, as it is raises in patients with gout.
Other forms of arthritis and their consequences for example hallux rigidus can be confused with hallux valgus as well as being a result of the deformity. For example a septic arthritis joint also shows a red and swollen joint. (Physio-pedia page “Hallux rigidus”: http://www.physio-pedia.com/Hallux_Rigidus)
Turf toe: pain and swelling due to turf toe can be confused with a hallux valgus presence. [27][28][29][30][31]
Key Evidence[edit | edit source]
Connor et al showed a statistically significant limitation in ROM ffor the physical therapy group alone compared to the group that also had CPM. No differences in groups likelihood of developing complications. CPM group discontinued oral analgesics more quickly as well as returned to wearing conventional shoewear in a significantly shorter time period.
Torkki et al compared surgery, orthoses, and watchful waiting. They found surgical interventions was superior to those obtained with orthosis or watchful waiting., although the use of orthosis did provide some short-term relief.
Recent Related Research (from Pubmed)[edit | edit source]
Resources
[edit | edit source]
Ferrari J, Higgins JPT, Prior TD. Interventions for treating hallux valgus(abductovalgus) and bunions(Review). Cochrane Database of Systematic Reviews 2004, issue 1. Art. No: CD 000964. DOI: 10.1002/14651858.CD000964.pub.2.
Torkki M, malvivaara A, Seitsalo S, Hoikka V, laippala P, Paavolainen P. Surgery v. orthosis vs. watchful waiting for hallux valgus. JAMA. 2001;285(19);2474-2480.
References
[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Radiographic validation of the Manchester scale for the classification of hallux valgus deformity, Menz HB et al, Rheumatology 2005;44:1061–1066 (1B)
- ↑ 2.0 2.1 Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010, 3:21 (1B)
- ↑ 3.0 3.1 3.2 Validity of self-assessment of hallux valgus using the Manchester scale, Menz H et al, Musculoskeletal Disorders 2010, 11:215 (1A)
- ↑ 4.0 4.1 Hallux Valgus and the First Metatarsal Arch Segment: A Theoretical Biomechanical Perspective. Glasoe W et al, Phys Ther. 2010;90:110–120. (3A)
- ↑ 5.0 5.1 5.2 5.3 5.4 Decision Making in the Treatment of Hallux Valgus, Joseph T, Mroczek K. Bulletin of the NYU Hospital for Joint Diseases 2007;65(1):19-23 19 (4)
- ↑ Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. Nix S., Smith M., Vicenzino B. Journal of Foot and Ankle Research 2010 (1a).
- ↑ SCHÜNKE et al, Prometheus lernatlas der anatomie - allgemeine anatomie und bewegungssystem (tweede druk), Georg Thieme Verlag, Stuttgart, 2005, 600p
- ↑ Internet, Bunion, (http://emedicine.medscape.com/article/1235796-overview#a11), 2016-11-11.
- ↑ Hannan MT, Menz HB, Jordan JM, Cupples LA, Cheng C-H, Hsu Y-H. Hallux Valgus and Lesser Toe Deformities are Highly Heritable in Adult Men and Women: the Framingham Foot Study. Arthritis care & research. 2013;65(9):1515-1521. doi:10.1002/acr.22040. (Levels of evidence: 2B)
- ↑ Golightly YM, Hannan MT, Dufour AB, Renner JB, Jordan JM. Factors Associated with Hallux Valgus in a Community-Based Cross-Sectional Study of Adults with and without Osteoarthritis. Arthritis care & research. 2015;67(6):791-798. doi:10.1002/acr.22517. (Levels of evidence: 2A)
- ↑ Barnish MS, Barnish J. High-heeled shoes and musculoskeletal injuries: a narrative systematic review. BMJ Open. 2016;6(1):e010053. doi:10.1136/bmjopen-2015-010053.
- ↑ Menz HB, Roddy E, Marshall M, et al. Epidemiology of Shoe Wearing Patterns Over Time in Older Women: Associations With Foot Pain and Hallux Valgus. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2016;71(12):1682-1687. doi:10.1093/gerona/glw004.fckLR(Levels of evidence: 3)
- ↑ MOL, W. et STRIKWERDA, R., Compendium orthopedie, De tijdstroom, Lochum, 1977, 343p. (p.232-234).
- ↑ 14.0 14.1 14.2 Pathomechanics, Gait Deviations, and Treatment of the Rheumatoid Foot: a clinical report. Dimonte P et al. Physical therapy 1982: Vol 62(8): 1148 – 1156 (5)
- ↑ RUSSE, O., et al, Orthopedisch onderzoek, De tijdstroom, Lochem, 1977.
- ↑ 16.0 16.1 Validation of a self-report instrument for assessment of hallux valgus. Roddy E et al. Osteoarthritis Cartilage 2007, 15:1008-1012. (2B)
- ↑ Coşkun G, Talu B, Bek N, et al. Effects of hallux valgus deformity on rear foot position, pain, function, and quality of life of women. J Phys Ther Sci 2016; 28:781–787. fckLR(Levels of evidence: 2C)
- ↑ Hallux valgus. F. DAY, M.D., Canad. M. A. J. April 16, 1957, vol. 76 (5)
- ↑ 19.0 19.1 19.2 19.3 The effects of sesamoid mobilization, flexor hallucis strengthening, and gait training on reducing pain and restoring function in individuals with hallux limitus: a clinical trial. Shamus J, Shamus E, Gugel RN, et al. J Orthop Sports Phys Ther. 2004;80:769–780. 2B
- ↑ 20.0 20.1 Rehabilitation after hallux valgus surgery: importance of physical therapy to restore weight bearing of the first ray during the stance phase. Schuh R, Hofstaetter SG, Adams SB Jr, et al. Phys Ther. 2009;89:934–945. (2C)
- ↑ Internet, Youtube: Bunion stretch and soft tissue release; 2012-08-01, (https://www.youtube.com/watch?v=q5Ov6LMISvU)
- ↑ (https://myhealth.alberta.ca/Health/aftercareinformation/_layouts/15/healthwise/media/medical/hw/h9991695_001_1_pi.jpg)
- ↑ http://www.everydayhealth.com/foot-health/8-foot-exercises-for-bunions.aspx
- ↑ https://www.allinahealth.org/mdex/en3092088.jpg
- ↑ KIM, M; et al. Comparison of muscle activities of abductor hallucis and adductor hallucis between the short foot and toe-spread-out exercises in subjects with mild hallux valgus. Journal of Back & Musculoskeletal Rehabilitation. 26, 2, 163-168, Apr. 2013 fckLR(levels of evidence: 1C)
- ↑ http://patient.info/doctor/hallux-rigidus
- ↑ SOBEL, E., Hallux valgus, assessment and conservative management and the role of faulty footwear, October 2001, (http://podiatrym.com/cme/oct01.pdf).
- ↑ Internet, Gout, 2016-12-08, (http://www.webmd.com/arthritis/tc/gout-topic-overview#1)
- ↑ Ashman CJ, Klecker RJ, Yu JS (2001) Forefoot pain involving the metatarsal region: differential diagnosis with MR imaging. Radiographies 21:1425–1440.
- ↑ Jeremy J., McCormick, MD, Robert B. Anderson, MD -Turf Toe: Anatomy, Diagnosis, and Treatment, Clin Sports Med. 2010 Apr;29(2):313-23 fckLR(Levels of evidence : A)
- ↑ MCRAE, R., Clinical Orthopaedic Examination, Churchill Livingstone, Edinburgh, 2010, 323p (p.236-238).