Gait
Original Editors - Karsten De Koster Top Contributors - Lucinda hampton, Kim Jackson, Nikhil Benhur Abburi, Alexandra Kopelovich, Admin, Rishika Babburu, Vidya Acharya, Shaimaa Eldib, Khloud Shreif, Maarten Cnudde, Simisola Ajeyalemi, Rucha Gadgil, Ayesha Arabi, Tolulope Adeniji and WikiSysop
Introduction[edit | edit source]
Bipedal walking is an important characteristic of humans.[1] This page presents information about the different phases of the gait cycle, important functions of the foot while walking and gait analysis which is a key skill for physiotherapists.
Definitions[edit | edit source]
Sandra J. Shultz describes gait as[3]: “...someone’s manner of ambulation or locomotion, involves the total body. Gait speed determines the contribution of each body segment. Normal walking speed primarily involves the lower extremities, with the arms and trunk providing stability and balance. The faster the speed, the more the body depends on the upper extremities and trunk for propulsion as well as balance and stability. The legs continue to do the most work as the joints produce greater ranges of motion trough greater muscle responses. In the bipedal system, the three major joints of the lower body and pelvis work with each other as muscles and momentum move the body forward. The degree to which the body’s centre of gravity moves during forward translation defines efficiency. The body’s centre moves both side to side and up and down during gait.”
The gait cycle is a repetitive pattern involving steps and strides[4]. A step is one single step, a stride is a whole gait cycle. The step time is the time between heel strike of one leg and heel strike of the contra-lateral leg[4]. Step width can be described as the mediolateral space between the two feet[4].
There are some differences between the gait and run cycle - the gait cycle is one third longer in time, the ground reaction force is smaller in the gait cycle (so the load is lower), and the velocity is much higher[5]. In running, there is also just one stance phase while in stepping there are two. Shock absorption is also much larger in comparison to walking.[5] This explains why runners have more overload injuries.[5]
The Gait Cycle[edit | edit source]
The sequences for walking that occur may be summarised as follows:[1]
- Registration and activation of the gait command within the central nervous system.
- Transmission of the gait systems to the peripheral nervous system.
- Contraction of muscles.
- Generation of several forces.
- Regulation of joint forces and moments across synovial joints and skeletal segments.
- Generation of ground reaction forces.
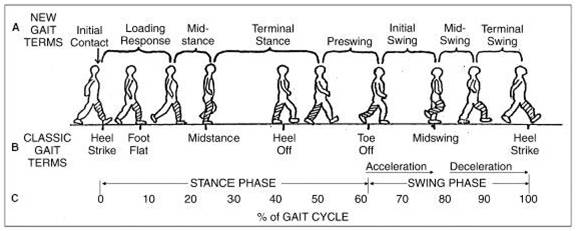
Classification of the gait cycle involves two main phases: the stance phase and the swing phase. The stance phase occupies 60% of the gait cycle while the swing phase occupies only 40% of it.[4] Gait involves a combination of open and close chain activities.[3] A more detailed classification of gait recognises six phases:[3][4]
- Heel Strike
- Foot Flat
- Mid-Stance
- Heel-Off
- Toe-Off
- Mid-Swing
Figure 1: Snijders CJ et al, Het Gaan, (https://eduweb.hhs.nl/~bergwandelen/onderzoek.htm), 1995.
An alternative classification of gait involves the following eight phases:[4][6]
- Initial Contact
- Loading Response
- Midstance
- Terminal Stance
- Pre swing
- Initial Swing
- Mid Swing
- Late Swing
Figure 2: Demos, Gait analysis, (http://www.ncbi.nlm.nih.gov/books/NBK27235/), 2004.
- Stance phase begins with the heel strike - this is the moment when the heel begins to touch the ground but the toes do not yet touch.[3] In the midstance phase, we can see settlement of the foot at the lateral border. During the change from mid-stance to toe-off stance, the 5 metacarpophalanges contract.[6] The toe-off phase is also named the propulsive phase.
- Swing phase begins, when the stance phase ends, This phase is the phase between the toe-off phase and the heel strike phase. In the swing-phase we can recognise two extra phases - acceleration and declaration[6] The acceleration phase goes from toe-off to midswing, while deceleration goes from midswing to heel strike. In the acceleration phase, the swing leg makes an accelerated forward movement with the goal of propelling the bodyweight forward. The declaration phase brakes the velocity of this forward body movement in order to place your foot down with control. Between these two phases, the mid-swing phase occurs. In this phase, both feet are under the body, with the heel next to each other.[7]
Phases of the Gait Cycle[edit | edit source]
Heel Strike[edit | edit source]
Also known as initial contact, is a short period which begins the moment the foot touches the ground and is the first phase of double support.[3] 30° flexion of the hip and full extension in the knee is observed. The ankle moves from a neutral (supinated 5°) position into plantar flexion.[3][4] After this, knee flexion (5°) begins and increases, just as the plantar flexion of the heel increased.[4] The plantar flexion is allowed by eccentric contraction of the tibialis anterior, extension of the knee is caused by a contraction of the quadriceps, flexion is caused by a contraction of the hamstrings, and the flexion of the hip is caused by the contraction of the rectus femoris.[4]
Foot Flat[edit | edit source]
In foot flat, or loading response phase, the body absorbs the impact of the foot by rolling in pronation.[3] The hip moves slowly into extension, caused by a contraction of the adductor magnus and gluteus maximus muscles. The knee flexes to 15° to 20° of flexion. [4]Ankle plantarflexion increases to 10-15°.[3][4]
Midstance[edit | edit source]
In midstance the hip moves from 10° of flexion to extension by contraction of the gluteus medius muscle.[4] The knee reaches maximal flexion and then begins to extend. The ankle becomes supinated[3] and dorsiflexed (5°), which is caused by some contraction of the triceps surae muscles.[3] During this phase, the body is supported by one single leg. At this moment the body begins to move from force absorption at impact to force propulsion forward.[3]
Heel Off[edit | edit source]
Heel off begins when the heel leaves the floor. In this phase, the bodyweight is divided over the metatarsal heads.[3] Here can we see 10-13° of hip hyperextension, which then goes into flexion. The knee becomes flexed (0-5°)[4] and the ankle supinates and plantar flexes.[4]
Toe Off[edit | edit source]
In the toe-off/pre-swing phase, the hip becomes less extended. The knee is flexed 35-40° and plantar flexion of the ankle increases to 20°.[3][4] In toe-off, like the name says, the toes leave the ground.[4]
Early Swing[edit | edit source]
In the early swing phase the hip extends to 10° and then flexes due to contraction of the iliopsoas muscle[4] 20° with lateral rotation.[3][4] The knee flexes to 40-60°, and the ankle goes from 20° of plantar flexion to dorsiflexion, to end in a neutral position.[3]
Mid Swing[edit | edit source]
In the midswing phase the hip flexes to 30° (by contraction of the adductors) and the ankle becomes dorsiflexed due to a contraction of the tibialis anterior muscle.[4] The knee flexes 60° but then extends approximately 30° due to the contraction of the sartorius muscle.[3][4] This extension is caused by the quadriceps muscles.[3][4]
Late Swing[edit | edit source]
The late swing/declaration phase begins with hip flexion of 25-30°, a locked extension of the knee and a neutral position of the ankle.[3]
Anatomical Considerations[edit | edit source]
The gait cycle involves movement in each part of the leg (and the body).
In the pelvic region, there is an anterior-posterior displacement, which alternates from left to right. This displacement facilitates anterior movement of the leg. At each side, there is an anterior-posterior displacement of 4-5°.[3][4][6]
In the frontal plane, varus movement is observed in the foot between heel-strike and foot-flat and between heel-off and toe-off. Some valgus movement is also observed between foot-flat and heel off in the feet. In the hip, some varus movement is observed in lateral movements. When the abductors are too weak, a Trendelenburg gait can be observed.[3][6]
It is important to recognize that the entire body moves while walking. A disorder in any segment of the body can have consequences on the individual's gait pattern, like a reduced knee flexion range in patients with a reconstructed ACL.[8]
Pathological Gait [edit | edit source]
Pathological gait is an altered gait pattern due to deformities, weakness or other impairments, for example, loss of motor control or pain. Alterations can broadly be divided into neurological or musculoskeletal causes[9].
Musculoskeletal Causes:[edit | edit source]
Pathological gait patterns resulting from musculoskeletal are often caused by soft tissue imbalance, joint alignment or bony abnormalities. Infliction of these on one joint often then impacts on other joints, affecting the gait pattern as a result[9]. The common deviation can be categorised broadly as[9]:
- Hip Pathology
- Knee pathology
- Foot and ankle pathology
- Leg length discrepancy
- Pain
Hip Pathology[edit | edit source]
Arthritis is a common cause of pathological gait. An arthritic hip has reduced range of movement during swing phase which causes an exaggeration of movement in the opposite limb ‘hip hiking[9].
Excessive Hip Flexion can significantly alter gait pattern most commonly due to; • Hip flexion contractures • IT band contractures, • Hip flexor spasticity, • Compensation for excessive knee flexion and ankle DF, • Hip pain • Compensation for excess ankle plantar flexion in mid swing. The deviation of stance phase will occur mainly on the affected side. The result is forward tilt of the trunk and increased demand on the hip extensors or increased lordosis of the spine with anterior pelvic tilt. A person with reduced spinal mobility will adopt a forward flexion position in order to alter their centre of gravity permanently during gait.
Hip Abductor Weakness. The abductor muscles stabilise the pelvis to allow the opposite leg to lift during the swing phase. Weak abductor muscles will cause the hip to drop towards the side of the leg swinging forward. This is also known as Trendelenburg gait[10]
Hip Adductor Contracture. During swing phase the leg crosses midline due to the weak adductor muscles, this is known as ‘scissor gait’[10]
Weak Hip Extensors will cause a person to take a smaller step to lessen the hip flexion required for initial contact, resulting in a lesser force of contraction required from the extensors. Overall gait will be slower to allow time for limb stabilisation. Compensation is increased posterior trunk positioning to maintain alignment of the pelvis in relation to the trunk[10]
Hip Flexor Weakness results in a smaller step length due to the weakness of the muscle to create the forward motion. Gait will likely be slower and may result in decreased floor clearance of the toes and create a drag
Knee Pathologies[edit | edit source]
Weak Quadriceps. The quadriceps role is to eccentrically control the knee during flexion through the stance phase. If these muscles are weak the hip extensors will compensate by bringing the limb back into a more extended position, reducing the amount of flexion at the knee during stance phase. Alternatively heel strike will occur earlier increasing the ankle of plantar flexion at the ankle, preventing the forward movement of the tibia, to help stabilise the knee joint[10].
Severe Quadriceps Weakness or instability at the knee joint will present in hyperextension during the initial contact to stance phase. The knee joint will ‘snap’ back into hyperextension as the bodyweight moves forwards over the limb[10]
Knee Flexion Contraction will cause a limping type gait pattern. The knee is restricted in extension, meaning heel strike is limited and step length reduced. To compensate the person is likely to ‘toe walk’ during stance phase. Knee flexion contractures of more than 30 degrees will be obvious during normal paced gait. Contractures less then this will be more evident with increased speeds[9][10].
Ankle Pathologies[edit | edit source]
Ankle Dorsiflexion Weakness results in a lack of heel strike and decreased floor clearance. This leads to an increased step height and prolonged swing phase[10].
Calf Tightening or Contractures due to a period of immobilisation or trauma will cause reduced heel strike due to restricted dorsiflexion. The compensated gait result will be ‘toe walking’ on stance phase, reduced step length and excessive knee and hip flexion during swing phase to ensure floor clearance[9].
Foot Pathologies[edit | edit source]
Hallux Rigidus results in a lack of dorsiflexion of the great toe. The MPJ uses the windlass effect to raise the arch and stiffen the foot during dorsiflexion of the hallux. This stiffness increases the efficiency of the propulsion portion of the gait cycle. To be efficient in creating stiffness, the hallux should be able to dorsiflex at least 65 degrees.
Leg Length Discrepancy[edit | edit source]
Leg length discrepancy can be as a result of an asymmetrical pelvic, tibia or femur length or for other reasons such as a scoliosis or contractures. The gait pattern will present as a pelvic dip to the shortened side during stance phase with possible ‘toe walking’ on that limb. The opposite leg is likely to increase its knee and hip flexion to reduce its length[9].
Antalgic Gait[edit | edit source]
Antalgic gait due to knee pain presents with decreased weight bearing on the affected side. The knee remains in flexion and possible toe weight-bearing occurs during stance phase[9]
Antalgic gait due to ankle pain may present with a reduced stride length and decreased weight bearing on the affected limb. If the problem is pain in the forefoot then toe-off will be avoided and heel weight-bearing used. If the pain is more in the heel, toe weight-bearing is more likely. General ankle pain may result in weight-bearing on the lateral border[9][10].
Antalgic gait due to hip pain results in reduced stance phase on that side. The trunk is propelled quickly forwards with the opposite shoulder lifted in an attempt to even the weight distribution over the limb and reduce weight-bearing. Swing phase is also reduced[9].
Common Neurological Causes of Pathological Gait[edit | edit source]
Hemiplegic Gait, often seen as a result of a stroke. The upper limb is in a flexed position, adducted and internally rotated at the shoulder. The lower limb is internally rotated, knee extended and the ankle inverted and plantarflexed. The gait is likely to be slow with circumduction or hip hitching of the affected limb to aid floor clearance[11][9].
Diplegic Gait. Spasticity is normally associated with both lower limbs. Contractures of the adductor muscles can create a ‘scissor’ type gait with a narrowed base of support. Spasticity in the lower half of the legs results in plantarflexed ankles presenting in ‘tiptoe’ walking and often toe dragging. Excessive hip and knee flexion is required to overcome this[11][9].
Parkinsonian Gait often seen in Parkinson’s disease or associated with conditions that cause parkinsonisms. Rigidity of joints results in reduced arm swing for balance. A stooped posture and flexed knees are a common presentation. Bradykinesia causes small steps that are shuffling in presentation. There may be occurrences of freezing or short rapid bursts of steps known as ‘festination’ and turning can be difficult[11][9].
Ataxic Gait is seen as uncoordinated steps with a wide base of support and staggering/variable foot placement. This gait is associated with cerebellar disturbances and can be seen in patients with longstanding alcohol dependency[11][9]
People with 'Sensory'Disturbances may present with a sensory ataxic gait. Presentation is a wide base of support, high steps, and slapping of feet on the floor in order to gain some sensory feedback. They may also need to rely on observation of foot placement and will often look at the floor during mobility due to a lack of proprioception[11][9].
Myopathic Gait. Due to hip muscular dystrophy, if it is bilateral the presentation will be a ‘waddling gait’, unilaterally will present as a Trendelenburg Gait[11].
Neuropathic Gaits. High stepping gait to gain floor clearance often due to foot drop[11]
Below are links to videos demonstrating normal gait and various gait abnormalities:
| [12] | [13] |
Gait Analysis[edit | edit source]
The analysis of the gait cycle is important in the biomechanical mobility examination to gain information about lower limb dysfunction in dynamic movement and loading.[14] When analysing the gait cycle, it is best to examine one joint at a time.[3] Objective and subjective methods can be used.[15][16]
Subjective[edit | edit source]
Our observation of gait is a subjective measure that we can use. We might ask the individual to walk normally, on insides and outsides of feet, in a straight line, running. All the time looking to compare sides and understanding of "normal".
Objective[edit | edit source]
An objective approach is quantitative and parameters like time, distance, and muscle activity will be measured. Other objective methods to assess the gait cycle that use equipment include:[17][16]
- Video Analysis and Treadmill
- Electronic and Computerized Apparatus
- Electronic Pedometers
- Satellite Positioning System[15]
Qualitative methods to assess and analyse gait include: [16]
- Rancho Los Amigos Hospital Rating List[18]
- Ten Meter Walking Test[19]
- 6 Minute Walk Test
- 2 Minute Walk Test
- Dynamic Gait Index
- Emory Functional Ambulation Profile[20]
- Timed Up and Go Test[21] This test is statistically associated with falling in men, but not in women.
- Functional Ambulation Categories[22]
- Tinetti-Test[23]
Clinical Bottom Line[edit | edit source]
Good knowledge of anatomy and biomechanics is important to understand the different phases of the gait cycle. When you know the normal pattern, you can see what’s going wrong!
References[edit | edit source]
- ↑ 1.0 1.1 Vaughan CL. Theories of bipedal walking: an odyssey. J Biomech 2001;36(2003):513-523.Available fromhttp://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.468.2414&rep=rep1&type=pdf
- ↑ Nicole Comninellis The Gait Cycle Animation Available from https://www.youtube.com/watch?time_continue=35&v=DP5-um6SvQI
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 Shultz SJ et al. Examination of musculoskeletal injuries. 2nd ed, North Carolina: Human Kinetics, 2005. p55-60.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 Loudon J, et al. The clinical orthopedic assessment guide. 2nd ed. Kansas: Human Kinetics, 2008. p.395-408.
- ↑ 5.0 5.1 5.2 Subotnick S. Sports medicine of the lower extremity. Harcourt (USA):Churchill Livingstone, 1999.
- ↑ 6.0 6.1 6.2 6.3 6.4 Demos, Gait analysis, (http://www.ncbi.nlm.nih.gov/books/NBK27235/), 2004.
- ↑ Berger W, et al. Corrective reactions to stumbling in man: neuronal co-ordination of bilateral leg activity during gait. J Physiol 1984;357: 109-125.
- ↑ Shi D, et al. Effect of anterior cruciate ligament reconstruction on biomechanical features of knee level in walking: a meta analysis. Chin Med J 2010;123(21):3137-3142.
- ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 9.13 9.14 Malanga G and Delisa J.A. Section One: Clinical Observation. Office of rehabilitation Research and Development No Date. http://www.rehab.research.va.gov/mono/gait/malanga.pdf (accessed 6 February 2010)
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 University of Washington. Pathologic Gait: Musculoskeletal http://courses.washington.edu/anatomy/KinesiologySyllabus/PathGait1Ortho.pdf (accessed 5 February 2015)
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Standford School of medicine #2 Gait Abnormalities http://stanfordmedicine25.stanford.edu/the25/gait.html (Accessed 5 February 2012)
- ↑ onlinemedicalvideoAbnormal Gait Exam : Myopathic Gait Demonstration. Available fromhttps://www.youtube.com/watch?time_continue=5&v=b5rIEx9SsCo
- ↑ scfpta gait deviation published final 001.wmvAvailable fromhttps://www.youtube.com/watch?time_continue=5&v=b5rIEx9SsCo
- ↑ Langer PS, et al. A practical manual of clinical electrodynography. 2nd ed. Deer Park: The Langer Foundation for Biomechanics and Sports Medicine Research, 1989.
- ↑ 15.0 15.1 Terrier P, Schutz Y. How useful is satellite positioning system (GPS) to track gait parameters? A review. J Neuro Eng Rehab 2005;2:28.
- ↑ 16.0 16.1 16.2 Deckers JHM, et al. Ganganalyse en looptraining voor de paramedicus, Houten, Bohnfleu van Lonhum, 1996.
- ↑ Frigo C, et al. Functionally oriented and clinically feasible quantitative gait analysis method. Med Biol Eng Comput 1998;36:179-185.
- ↑ Shumway-Cook A, Woollacott MH. Motor control: translating research into clinical practice. Lippincott Williams and Wilkins, 2007. p.408.
- ↑ Van Peppen RPS, KNGF-richtlijn Beroerte, 2004, Nederlands Tijdschrift voor Fysiotherapie.
- ↑ Baer RH, Wolf SL. Modified emory functional ambulation profile: an outcome measure for the rehabilitation of post stroke gait dysfunction. Stroke 2001;32(4):973-979.
- ↑ Potsiadlo D, Richardson S. The timed “Up and Go”: a test of functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39(2):142-148.
- ↑ Shephard RJ, Taunton JE. Foot and ankle in sport and exercise, Toronto:Karger, 1987. p30-38.
- ↑ Bautmans I, et al. The feasibility of whole body vibration in institutionalised elderly persons and its influence on muscle performance, balance and mobility: a randomised controlled trial. BMC Geriatr 2005;5:17.