Foot and Ankle Assessment
Original Editor - Ewa Jaraczewska
Top Contributors - Ewa Jaraczewska, Jess Bell, Kim Jackson, Lucinda hampton, Aminat Abolade, Nupur Smit Shah, Robin Leigh Tacchetti and Robin Tacchetti
Assessment Goal[edit | edit source]
The goal of the assessment is to :
- determine the extent of the injury
- identify what has been injured
- establish a framework that can be negotiated with the patient regarding:
- timeline
- further referral
- treatment plan
- treatment strategy
Subjective[edit | edit source]
Patient Intake[edit | edit source]
Gathering information during the history provides the clinician with clues as to what structure is likely affected, further guiding the physical examination. For example, the mechanism of injury is important as it provides information on what forces went through what structure, and in what direction. This will further provide information on what tissues and/or structures are likely stretched or damaged.
Example: a valgus force may indicate a deltoid ligament sprain, whereas a varus force may be suggestive of injury to the anterior talofibular ligament (ATFL) and/or calcaneofibular ligament (CFL).
The patient's history should include questions related to:
- the time of the injury (acute vs subacute vs chronic)
- the mechanism of the injury and forces involved in the injury (loose vs locked position)
- the activity that leads to the injury (an athletic event vs recreational activity vs activity of daily living)
- contributing factors (shoes, terrain, medical history, medications, general health)
- training history
- previous treatment (successes vs failures)
The results from the interview should assist with establishing risk factors and precautions during objective assessment.
At the end of the patient's interview, the physiotherapist must have a good idea of what needs to be examined objectively. The clinician must later determine if the results of the assessment match the subjective signs and symptoms the patient complained about. Helene Simpson
Special Questions[edit | edit source]
Red flags are signs and symptoms found in the patient history and clinical examination that may be suggestive of serious pathology. If serious pathology is suspected, immediate referral to a medical doctor is indicated and the physiotherapist's concerns should be noted.
Red Flags specific to foot and ankle assessment
- Unable to bear weight: rule out fracture (Ottawa Rule)
- Bilateral pins and needles or numbness in the lower limb
- Bowel and bladder dysfunction (i.e., the patient is unable to feel themselves while going to the toilet)
- Incontinence
- Paraesthesia in the groin region
- Loss of pulses in the lower leg (vascular compromise)
- Obvious deformity
- Joint dislocation
- Positive Babinski sign
- Unable to calf raise: rule out Achilles tendon rupture
Yellow Flags specific to foot and ankle assessment
- Severity of symptoms do not match the subjective information→More tests
- Pain preventing objective assessment→Detailed assessment delayed
Objective[edit | edit source]
Observation[edit | edit source]
- Observation
- perform with the patient in supine, sitting or standing
- watch for the presence of swelling
- assess skin colour
- check skin temperature
- watch for signs of muscle wasting
- notice foot and toes deformities: bunions, hammertoes, claw toes, calluses
- Posture Assessment
- If the patient is able to stand: observe in quiet stance and assess weight-bearing distribution; pay attention to foot arches; observe walking with or without assistive device: watch for back deformity: scoliosis, lordosis, kyphosis; observe gait pathology, eg., Trendelenburg; notice any changes in the lower leg alignment: knee valgus or varus, foot pronation or supination; observe gait cycle: heel strike, toe-off.
- If the patient is unable to stand: observe in sitting, feet flat on the floor, assess the weight-bearing distribution and the patient's ability to take a load while preparing for sit to stand transition
Functional Tests[edit | edit source]
The choice of functional tests is based on the patient's signs and symptoms and the physiotherapist's initial list of suspected pathologies. It may include:
- Sit to stand
- Squat: defines the integrity of the syndesmosis joint
- Deep squat
- Tandem stance
- Lounge position
- Step forward and backwards: weight transfer
- Single leg stance: assess postural and balance control
- Step-up
- Step down + step overs
- Knee to wall test / Knee extended might relate more to a range of motion dorsiflexion in gait: helps to assess ankle dorsiflexion range of motion
- Squeeze Test: helps to diagnose the syndesmotic ankle sprain
- External Rotation Test: assess the integrity of the syndesmotic ligaments
- Anterior drawer test: defines ankle mechanical instability
For a high-level performance, additional tests may include a jump or a hop.
Additional details can be found on the Foot and Ankle Assessment-Investigations and Tests page.
Balance Assessment[edit | edit source]
The results of the balance assessment in the foot and ankle injury help to develop a sensory targeted rehabilitation program that stimulates sensory receptors.[2] The following are the examples of balance tests:
- Static postural control :
- Balance Error Scoring System (BESS)
- Airplane balance test
- Dynamic postural control
Palpation[edit | edit source]
During palpation exam which can be performed in supine, prone and or seated position clinician checks for points of tenderness:
- On the medial, lateral, posterior and anterior part of the lower leg and around calcaneus.
- Along joint lines
- At the attachments of the medial and lateral ligaments
- At the Achilles tendon, peronei and other extrinsic muscles
Neurologic Assessment[edit | edit source]
The neurologic exam can assist the clinician with identifying a potential neurological aetiology for the observed ankle or foot pathology. It includes peripheral neuropathy or central nervous system impairment.[5]
The complete neurological examination should include:
- Inspection
- Reflex testing
- Achilles Tendon (S1)
- Patella Ligament (L3/L4)
- Muscle tone assessment
- Sensory testing (proprioception, light touch, sharp/dull)
- Plantar response (also known as the Babinski response)
- Clonus
This video demonstrates peripheral neurological examination performed when pathology or referral from the lumbar spine is suspected:
Vascular Assessment[edit | edit source]
If compromised circulation is suspected, the clinician should palpate to assess pulses of the dorsalis pedis artery. The state of the vascular system can also be assessed by the response of symptoms to positions of dependence and elevation of the lower limbs.
Movement Testing[edit | edit source]
- Active Range of Motion (AROM) and Passive Range of Motion (PROM) testing:
- plantarflexion(PF)/ dorsiflexion (DF)
- toe extension/ flexion
- pronation/supination
- big toe extension/ flexion
This video demonstrates a complete foot and ankle ROM assessment:
- Joint mobility: test each individual joint with a glide and compare to the contralateral side and to normal values
These videos demonstrate specific joint mobility assessment:
- Muscle Strength: Specific active muscle tests (isometric and through range): Gastrocnemius, Soleus, Tibialis posterior, Tibialis anterior, Extensor Hallucis Longus and Brevis/Flexor Hallucis Brevis, Intrinsics (toe purchase test/paper pull out test[13])
This video demonstrates an ankle and foot muscles isometric strength tests:
Biomechanical Evaluation[edit | edit source]
A foot assessment can be used to classify foot type as well as to identify possible etiological factors relating to injury in order to properly prescribe therapeutic interventions.
Details can be found on the Biomechanical Assessment of the Foot and Ankle page.
Additional Testing[edit | edit source]
Patient-Reported Outcomes (PROs)[edit | edit source]
Patient-reported outcome measures allow clinicians to prioritise the outcomes most important to patients. In the foot and ankle assessment, it was determined that physical performance and pain interference were at the top of the patients' priorities when assessing their satisfaction with treatment.[15][16]
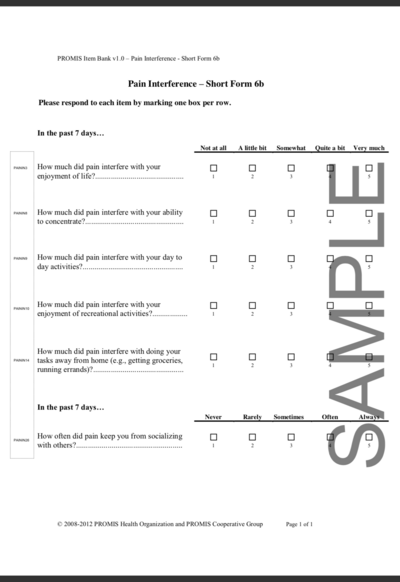
Patient-Reported Outcomes Measurement Information System Pain Interference (PROMIS PI)[edit | edit source]
One of the PROs tools is the Patient-Reported Outcomes Measurement Information System(PROMIS) which takes information from multiple domains to assess patient-reported outcomes. [17] The pain interfering with function is defined as the heavily weighted domain assessing each patient's satisfaction with treatment (PROMIS PI). When compared with the standard patient-reported pain scale (VAS), PROMIS PI detects pain at lower levels than the Visual Analogue Scale. [15]
Visual Analogue Scale (VAS)[edit | edit source]
The Visual Analogue Scale (VAS) is a generic patient-reported pain scale that is used to assess the patient's perception of pain only. The scale may not be reliable in the assessment of the elderly population presenting with mild cognitive deficits or showing difficulties in understanding the instruction. [18]
Foot and Ankle Ability Measure (FAAM)[edit | edit source]
The Foot and Ankle Ability Measure (FAAM) is a self-report outcome instrument developed to assess physical function for individuals with foot and ankle related impairments. This self-report outcome instrument is available in English, German, French and Persian. The Foot and Ankle Ability Measure is a 29-item questionnaire divided into two subscales: the Foot and Ankle Ability Measure, 21-item Activities of Daily Living Subscale and the Foot and Ankle Ability Measure, 8-item Sports Subscale.
Detailed information you will find on Foot and Ankle Ability Measure page.
Conclusion[edit | edit source]
What→ so what→ now what[edit | edit source]
What?[edit | edit source]
At the end of the examination, the clinician should return to the initial list of potential problems/suspected diagnoses and choose the three most likely diagnoses.
The foot and ankle assessment is completed when the clinician is able to provide a response to question # 1:
- What has happened?
So What?[edit | edit source]
The foot and ankle assessment is completed when the clinician is able to provide a response to question # 2:
- What were the consequences of the incident?
Now What?[edit | edit source]
The foot and ankle assessment is completed when the clinician is able to provide a response to question # 3:
- How the consequences of the incident are going to be treated?
- What is the treatment plan?
- What is the treatment strategy?
- What are the short and long term goal?
- What is the timeline for goal completion?
Virtual Foot and Ankle Assessment[edit | edit source]
Telehealth is a well-established alternative to in-person visits as a response to the COVID pandemic and beyond.[19] Development of the objective assessment tools for the telehealth needs is a priority in order to demonstrate the outcome of the treatment provided via telehealth.
Virtual assessment for foot and ankle pathology has been developed and tested.[19] The following is the guideline for the virtual examination.
Pre-Visit[edit | edit source]
Prior to the virtual visit, the patient should obtain a pre-visit form and information regarding wardrobe expectations and the camera set up during the examination. The pre-visit form needs to be completed by the patient or the caregiver and it consists of the questions regarding:[19]
- Patient's chief complaint and reason for the visit
- Patient's past and present medical and surgical history
- Medication and allergies
- Social history.
Additional information may include biometrics (height and weight) and vital signs (HR, blood pressure, body temperature).
Virtual Assessment[edit | edit source]
The foot and ankle examination includes:
- Inspection
- Patient in standing and seated
- Camera set up to provide front, side and back view of the foot and ankle
- The elements of inspection are as follow: alignment, muscle atrophy, joint deformity, incisions, scarring, rash, swelling, ecchymosis, erythema. In addition, the plantar aspect of the foot must be examined for ulcers, abrasions, and skin breakdown.
- Palpation
- Patient uses one finger to point to the area of maximal pain or discomfort
- Range of motion testing
- Use web-based goniometer[20]
- Performed actively (patient's own muscle power) and passively (family member manipulates the joint)
- Strength testing
- Assisted by the family member
- Exam performed on both sides at the same time and differences reported
- Functional assessment
- Gait observation
- Neurovascular assessment.
- Patient touches the skin on both sides and reports differences, however sensory feedback from the patient’s own fingers touching the skin is a limitation.
Additional tests for flatfoot, cavovarus foot, hallux rigidus, and Achilles rupture may be added if the pathology is suspected.[19]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Complete Musculoskeletal Exam of the Foot and Ankle. 2013. Available from: https://www.youtube.com/watch?v=QnX5J-j79qQ [last accessed 4/01/2022]
- ↑ 2.0 2.1 Wikstrom EA, McKeon PO. Predicting balance improvements following STARS treatments in chronic ankle instability participants. J Sci Med Sport. 2017 Apr;20(4):356-361. doi: 10.1016/j.jsams.2016.09.003. Epub 2016 Sep 20.
- ↑ Doctors of Physical Therapy. Airplane Test. 2019. Available from: https://www.youtube.com/watch?v=WysXgJNVOnk [last accessed 18/01/2022]
- ↑ Ascension Via Christi. Musculoskeletal Physical Exam: Ankle. 2011. Available from: https://www.youtube.com/watch?v=QiSm8rz2cmo&t=270 [last accessed 4/01/2022]
- ↑ Akoh CC, Phisitkul P. Clinical examination and radiographic assessment of the cavus foot. Foot Ankle Clin. 2019 Jun 1;24(2):183-93.
- ↑ Dermatomes Lower Limb | Peripheral Neurological Examination. 2017. Available from: https://www.youtube.com/watch?v=SzAyUsA25MQ [last accessed 5/01/2022]
- ↑ Vascular assessment of the lower limb and clinical diagnostics. 2011. Available from: https://www.youtube.com/watch?v=nhmBL3N_igg&t=136s [last accessed 5/01/2022]
- ↑ Foot & Ankle: Overview of ROM Assessment. 2020. Available from: https://www.youtube.com/watch?v=XkZp15vYNT0 [last accessed 5/01/2022]
- ↑ Kris Porter DPT.Ankle Exam and Manual Therapy. 2016. https://www.youtube.com/watch?v=VN55vtFJOgc[last accessed 7/01/2022]
- ↑ Kris Porter DPT. Sub-Talar Exam and Manual Therapy. 2016. Available from:https://www.youtube.com/watch?v=_cRTUWlX-Tk [last accessed 7/01/2022]
- ↑ Kris Porter DPT.Mid-Foot (mid-tarsal) Examination. 2016. Available from: https://www.youtube.com/watch?v=qv62Qhn7DN8 [last accessed 7/01/2022]
- ↑ Kris Porter DPT. Hallux (Great Toe) Examination (1st MTP). 2016. Available from: https://www.youtube.com/watch?v=tH5gZ3My5Q0 [last accessed 7/01/2022]
- ↑ Nery C, Raduan FC, Catena F, Mann TS, de Andrade MA, Baumfeld D. Plantar plate radiofrequency and Weil osteotomy for subtle metatarsophalangeal joint instablity. J Orthop Surg Res. 2015 Nov 19;10:180. doi: 10.1186/s13018-015-0318-1.
- ↑ Resisted Isometric Testing (Ankle/Foot). 2015. Available from: https://www.youtube.com/watch?v=MBseUN2KcJ8 [last accessed 5/01/2022]
- ↑ 15.0 15.1 Bernstein DN, Kelly M, Houck JR, Ketz JP, Flemister AS, DiGiovanni BF, Baumhauer JF, Oh I. PROMIS pain interference is superior vs numeric pain rating scale for pain assessment in foot and ankle patients. Foot & ankle international. 2019 Feb;40(2):139-44.
- ↑ Promis. Northwestern University 2022. Health Measures (Internet). Available fromhttps://www.healthmeasures.net/explore-measurement-systems/promis. Last access 6/01/2022
- ↑ Kendall R, Wagner B, Brodke D, Bounsanga J, Voss M, MS, Gu Y, Spiker R, Lawrence B, Hung M. The Relationship of PROMIS Pain Interference and Physical Function Scales. Pain Medicine 2018 Sep; 19(9):1720–1724.
- ↑ Shazadeh Safavi P, Janney C, Jupiter D, Kunzler D, Bui R, Panchbhavi VK. A systematic review of the outcome evaluation tools for the foot and ankle. Foot & ankle specialist. 2019 Oct;12(5):461-70.
- ↑ 19.0 19.1 19.2 19.3 Eble SK, Hansen OB, Ellis SJ, Drakos MC. The Virtual Foot and Ankle Physical Examination. Foot & Ankle International. 2020;41(8):1017-1026.
- ↑ Ravi B, Kapoor M, Player D. Feasibility and reliability of a web-based smartphone application for joint position measurement. J Rehabil Med. 2021 May 10;53(5):jrm00188.