Foot Orthotics Assessment
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Lucinda hampton, Ewa Jaraczewska and Tarina van der Stockt
Introduction[edit | edit source]
Orthotics is a branch of medicine dealing with the making and fitting of orthotic devices. There are many interchangeable terms for this, a few being foot orthotic/orthosis/insole/shoe insert.
Three Main Types of Foot Orthoses[edit | edit source]
- Off the shelf (OTS) Insoles
- Functional Foot Orthoses (FFO)
- Custom Molded Total Contact Insoles (TCI)
What do foot orthoses do?[edit | edit source]
A foot orthosis is generally referred to as an externally applied apparatus that can be inserted into footwear to support or improve the function of the foot and ankle. The two main goals are the reduction of pressure across an area or to accommodate congenital or acquired deformities. The ultimate outcome would be near-neutral subtalar joint alignment through the gait cycle or the individuals highest functional level. [1]
- Support
- Correct, if mobile
- Accommodate if not
- Shock absorption
- Re-distribute pressure
Basic Foot Anatomy[edit | edit source]
- 28 Bones
- 33 Joints
- Ligaments
- Tendons
- Muscles
- Joints
- Plantar Fascia
Plantar Fascia[edit | edit source]
- The plantar fascia is not a nerve, tendon or muscle, but a strong fibrous tissue. This stiff and relatively impermeable covering helps to protect the muscles of the sole of the foot.[2]
- This tissue originates deep within the plantar surface of the calcaneus fanning out across the met heads, it divides and attaches to the base of the phalanges of each toe.
- During walking, as the toes dorsiflex at push off the plantar fascia wraps around the metatarsal heads and tightens. This pulls the calcaneus towards the metatarsal heads and in turn maintains the shape of the longitudinal arch and supports the foot to enable propulsion. This is a phenomenon known as the windlass mechanism.[3]
Windlass Mechanism[edit | edit source]
Hicks first described the windlass mechanism in 1954 as a one-to-one coupling between metatarsal joint dorsiflexion and medial longitudinal arch rise. Based on an engineering concept of lifting weights via a pulley system. He proposed that dorsiflexion of the toes tightens the plantar aponeurosis and pulls the metatarsal heads towards the calcaneus thereby increasing the structural height of the longitudinal arch. This action occurs naturally at push off in gait cycle as toes dorsiflex and the foot becomes stiffer to aid propulsion. During loading and mid stance the arch will stretch. The human foot is flexible by its nature of many articulations and requires to be flexible at times and rigid at other times to promote normal gait. Important to remember that the plantar fascia will stretch and recoil at different stages of the gait cycle.[4]
Important Joints with regards to Foot Orthosis for ROM in the Foot/Ankle[edit | edit source]
- Hindfoot
- Talocrural Joint
- Sub Talar joint
- Mid Foot
- Tarsometatarsal Joint
- Calcaneocuboid Joint
- Talonavicular Joint
- Fore Foot
- 1st Metatarsal Phalangeal Joint
Terminology used in Orthotics[edit | edit source]
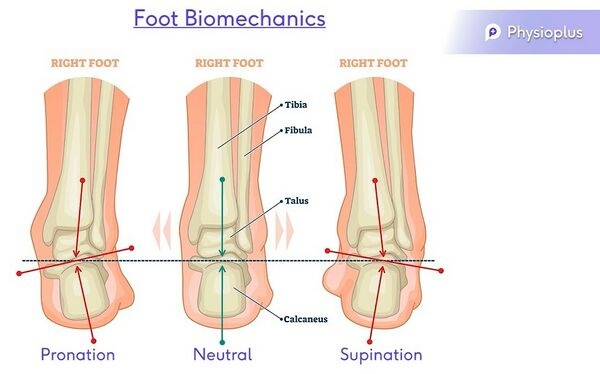
Neutral
Varus = Inverted
Pronation – Eversion, abduction, dorsiflexion & medially rotated subtalar joint
Supination- Inversion, adduction, plantarflexion & laterally rotated subtalar joint.
Purpose of human foot[edit | edit source]
“[The human foot] enables propulsion through space, adaptation to uneven terrain, absorption of shock, and support of body weight.”[5]
The human foot is a complex mechanism with a number of theories of biomechanics. The structure, function and position leave the foot exposed to risk of injury. When understanding the foot biomechanics, it is key to assess in non weight bearing, weight bearing and during gait.
Orthotic Foot Ankle Assessment[edit | edit source]
- Patient History
- ROM
- Muscle Power
- Sensation/Pain
- Proprioception
- Biomechanical Analysis
- Leg length
1. Patient History[edit | edit source]
- Gait pattern and biomechanical analysis on entrance
- Type of shoes[6]
- Assistive devices
- History of underlying conditions, foot problems and the primary problem affecting the individual on consultation.
2. Range of Motion[edit | edit source]
When testing range of motion to create a foot orthosis, the following testing should be carried out
- Active
- Passive
- Weightbearing
- Non weightbearing
Active and Passive Movements in the Foot and Ankle[7]
- Dorsiflexion/ Plantarflexion - Quick test for the Ankle Joint
- Pronation/ Supination – Quick test for the Subtalar joint
- Eversion/ Inversion
- Abduction/ Adduction
- Toe flexion/ extension – Quick test for the Metatarsal Phalangeal joints
Non weight bearing assessment[7]
- Windlass Test - can be effective in examining dysfunction of the plantar fascia although specificity has not been proved.
- Passively extend hallux at MTP joint
- Plantar aponeurosis should tighten and reduces dist between calcaneus and Metatarsals.
- Note angle of extension to initiate arch, can vary
- Increase MLA
- Positive Test = A positive test is considered if passive extension is continued to end range or until the patient's pain is reproduced in Plantarfascitis
- Passively extend hallux at MTP joint
- Pain in medial calcaneus and plantarfascia on palpation
- Hallux Limitus/rigidus
- Both affect the windlass mechanism and gait pattern and normal functioning of the foot.
- Hallux Rigidus[8]
- Very limited dorsiflexion mobility or no mvt. there is crepitation with joint mobilization and pain associated with any movement of the first MTP joint.
- Hallux Limitus[9] (FnHL)
- Reduced dorsiflexion movement, resulting in reduced range of dorsiflexion of the first MTP joint.
- In gait, loss of metatarsophalangeal joint extension during the second half of the single-support phase, when the weightbearing foot is in maximal dorsiflexion.
- Hallux Rigidus[8]
3. Muscles of the Foot and Ankle[edit | edit source]
There are four muscle compartments in the lower leg. These muscles are all tested using the standardized Oxford Scale.
Action: Plantarflexion
Muscles: Gastrocnemius, Soleus and Plantaris
Action: Plantarflexion, Adduction and Inversion
Muscles: Tibialis Posterior, Flexor Hallicus Longus and Flexor Digitorum Longus
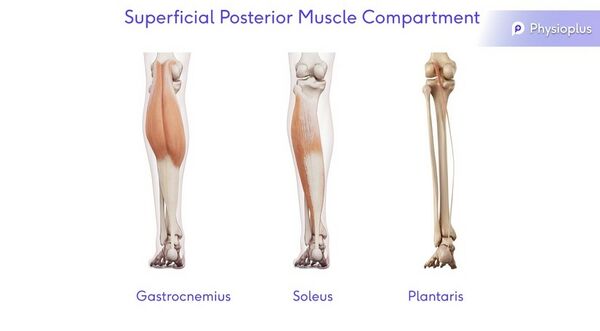
Superficial Posterior Muscle Compartment
Action: Plantarflexion
Muscles: Gastrocnemius, Soleus and Plantaris
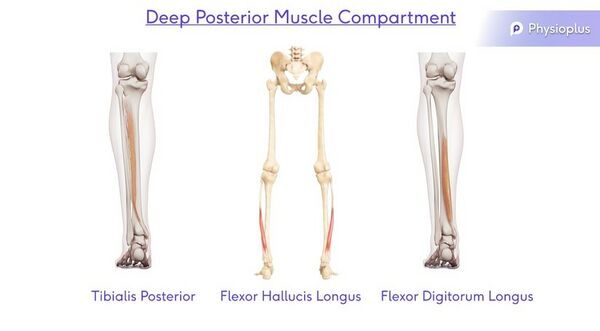
Deep Posterior Muscle Compartment
Action: Plantarflexion, Adduction and Inversion
Muscles: Tibialis Posterior, Flexor Hallicus Longus and Flexor Digitorum Longus
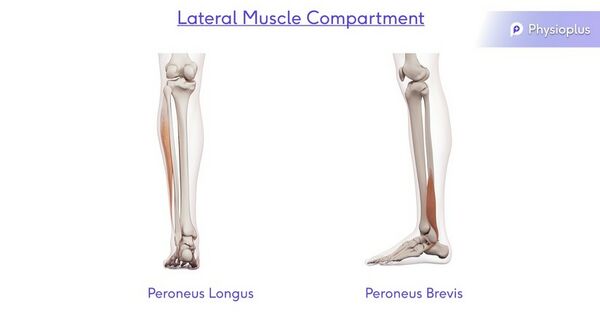
Lateral Muscle Compartment
Action: Dorsiflexion, Abduction and Eversion
Muscles: Peroneus Longus and Peroneus Brevis
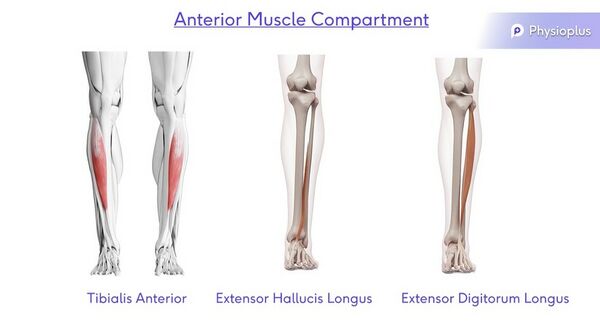
Anterior Muscle Compartment
Action: Dorsiflexion, Abduction and Inversion
Muscles: Tibialis Anterior, Extensor Hallicus Longus and Extensor Digitorum Longus
See the following pages for more information on the muscle testing of:
4. Sensation/Pain[edit | edit source]
Please see page on Sensation, Sensory Examination
5. Proprioception[edit | edit source]
Please see page on Proprioception, Assessing Proprioception
6. Biomechanical Analysis[edit | edit source]
Static
- Too many toes/ Too few toes
- Jacks Test
- Windlass test
- Rear foot and forefoot alignment
- Normal/ideal foot alignment occurs when:
- Distal 1/3 of leg is vertical
- Calcaneus is vertical to the supporting surface
- Plantar forefoot is parallel to the plantar rearfoot
- Variations from this “normal’ foot alignment (‘intrinsic foot deformities’) lead to abnormal foot function
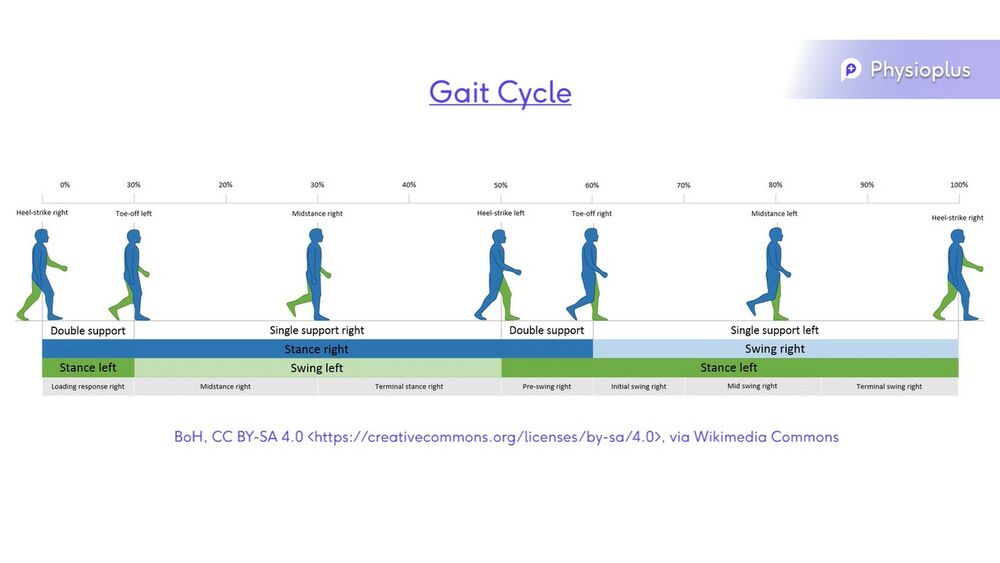
Dynamic Normal Walking[7]
- Phases of Normal Walking
- Heel strike
- Mid stance
- Terminal stance
- Pre swing
- Swing Phase
- Ground clearance is important in Swing phase
- Proprioception and balance is important for approximately 40% of the gait pattern where an individual is standing on one leg.
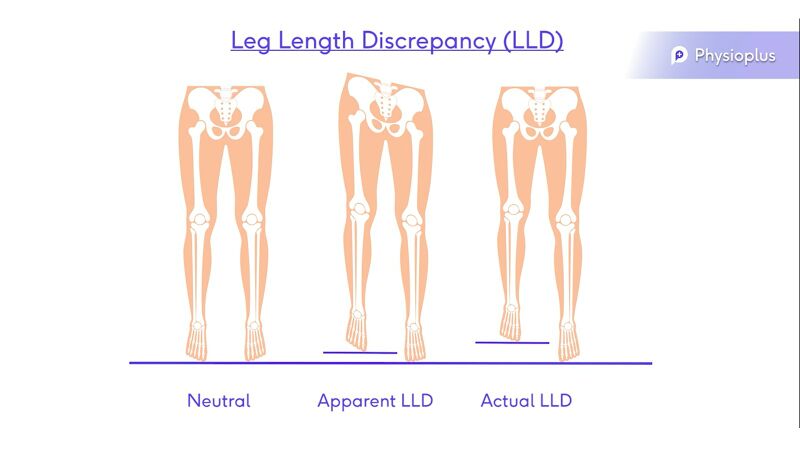
7. Leg Length Discrepancy (LLD)[edit | edit source]
- Dipping
- Pelvic Obliquity
- Retraction
- Scoliosis
- Apparent leg length
- Actual leg length[10]
References[edit | edit source]
- ↑ Elattar O, Smith T, Ferguson A, Farber D, Wapner K. Uses of braces and orthotics for conservative management of foot and ankle disorders. Foot & Ankle Orthopaedics. 2018 Aug 3;3(3):2473011418780700.
- ↑ Welte L, Kelly LA, Kessler SE, Lieberman DE, D'Andrea SE, Lichtwark GA, Rainbow MJ. The extensibility of the plantar fascia influences the windlass mechanism during human running. Proceedings of the Royal Society B. 2021 Jan 27;288(1943):20202095.
- ↑ Sichting F, Holowka NB, Ebrecht F, Lieberman DE. Evolutionary anatomy of the plantar aponeurosis in primates, including humans. Journal of anatomy. 2020 Jul;237(1):85-104.
- ↑ Sichting F, Ebrecht F. The rise of the longitudinal arch when sitting, standing, and walking: Contributions of the windlass mechanism. PloS one. 2021 Apr 8;16(4):e0249965.
- ↑ Bolgla LA, Malone TR. Plantar fasciitis and the windlass mechanism: a biomechanical link to clinical practice. Journal of athletic training. 2004 Jan;39(1):77.
- ↑ Gegen ME, Plummer T, Darr N. An Exploratory Study of The Perceptions of Footwear for Individuals who use Lower Limb Orthotics. Internet Journal of Allied Health Sciences and Practice. 2020;18(4):8.
- ↑ 7.0 7.1 7.2 Alazzawi S, Sukeik M, King D, Vemulapalli K. Foot and ankle history and clinical examination: A guide to everyday practice. World journal of orthopedics. 2017 Jan 18;8(1):21.
- ↑ Colò G, Fusini F, Samaila EM, Rava A, Felli L, Alessio-Mazzola M, Magnan B. The efficacy of shoe modifications and foot orthoses in treating patients with hallux rigidus: a comprehensive review of literature. Acta Bio Medica: Atenei Parmensis. 2020;91(Suppl 14).
- ↑ Graydon M. Hallux Limitus/Rigidus. Clinical Practice Guidelines. 2018:140.
- ↑ Menez C, L'Hermette M, Coquart J. Orthotic insoles improve gait symmetry and reduce immediate pain in subjects with mild leg length discrepancy. Frontiers in sports and active living. 2020;2.