Foot Orthoses
Original Editor - Mariam Hashem
Top Contributors - Mariam Hashem, Kim Jackson, Jess Bell, Naomi O'Reilly, Matthew Chin, Admin, Tarina van der Stockt and Lucinda hampton
Definition and Mechanics[edit | edit source]
According to the Atlas of Orthoses and Assistive Devicesfoot orthoses (FO) are like the tires on an automobile. They provide a critical, biomechanical contact point for the human body, and they can be helpful to correct problems in the foot, knee, hip, and spine''[1].- An orthosis is a single device, a group of them are referred to as orthoses.
- We can use the term orthotic devices but not orthotics as they refer to braces and splints[2]
Foot orthoses were historically believed to work by correcting mechanical abnormalities as seen visually such as when correcting a perceived ‘over-pronated foot’. However, more current understanding leans toward the therapeutic benefit being achieved from the internal kinetic changes.
Applying the tissue stress principals, altering the internal demands on the overloaded tissue by the use of proper orthoses can explain pain reduction and improvement in function in foot conditions [3].
There is also room for applying biopsychosocial modelling to foot orthoses.
- Understanding the patient's condition clearly and communicating effectively with them could have positive effects on the success of the use of orthoses.
- Asking questions on how the patient feels about orthoses if they have positive feelings then using the orthoses could promote the therapeutic benefit. If they feel otherwise, then having an effective conversation can help determine the best route of treatment.[3]
Clinical Uses[edit | edit source]
The uses of orthoses vary from pain relief, comfort and enhancement of performance.
They are widely used in the treatment of different foot conditions:
Plantar Heel Pain[edit | edit source]
The use of foot orthoses is recommended by
- The Journal of Orthopedic Sports and Physical Therapy to support the medial longitudinal arch and cushion the heel in individuals with heel pain/plantar fasciitis. To reduce pain and improve function, they are advised for short- (2 weeks) to long term (1 year) periods, especially in those who respond positively to anti pronation taping techniques[4].
- Wittaker and Colleagues reviewed 19 clinical trials and reported moderate-quality evidence supporting the use of foot orthoses as an effective intervention at reducing pain in the medium term of plantar heel pain[5].
- A study investiging the effect of wearing custom foot orthoses on: first-step pain; average 24-h pain; and plantar fascia thickness in people with unilateral plantar fasciopathy over 12 weeks - Found improvement in first-step pain and reduced plantar fascia thickness over a period of 12 weeks compared to new shoes alone or a sham intervention[6].
- Rasenberg et al reviewed twenty studies investigating the effects of eight different types of foot orthoses on pain, function and self-reported recovery with plantar heel pain compared with other conservative interventions. Their findings suggested there isn't enough evidence to support the use of foot orthoses for plantar heel pain[7].
Patellofemoral Pain Syndrome[edit | edit source]
The Journal of Orthopaedic & Sports Physical Therapy 2019 guidelines recommended clinicians to prescribe prefabricated foot orthoses for patients with greater than normal pronation to reduce pain, but only for a short term (up to 6 weeks). The use of foot orthoses should be combined with other interventions[8].
The applied use of foot orthoses on PFPS as suggested clinically and in literature is the use of single leg squat or double leg squat.
- If reproduced pain in the patellofemoral area then the clinician asks the patient to repeat the test wearing a foot orthosis.
- If this reduces pain, this patient might benefit from a foot orthosis [9].
Another test that was developed to identify patients with Patellofemoral Pain who are likely to benefit from foot orthoses by
- Measuring the width of the patient's foot from a non-weight bearing position then compares it to standing mid-foot width
- If there was a great increase in midfoot width, then foot orthoses might help[10].
However - a study by Matthews and Colleagues reported that the test is not reliable[11]
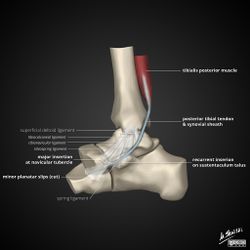
Tibialis Posterior Tendon Dysfunction[edit | edit source]
Tibialis posterior is a powerful foot inverter. See image R
- In case of dysfunction, the use of an orthosis to apply some external supinatory support and external inversion
- Theoretically, decrease the load on the tibialis posterior muscle[3].
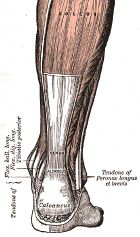
Peroneal Tendon Dysfunction[edit | edit source]
- Opposite to the use in tibialis posterior tendon pain,
- Can use an orthosis to provide an external eversion or pronatory force to the foot and therefore hopefully get some therapeutic benefits[3].
Midfoot Osteoarthritis[edit | edit source]
A carbon fibre type shell orthosis can reduce the amount of bending stress through the midfoot.
Achilles Tendinopathy[edit | edit source]
- Wearing custom fit semirigid insoles for 4 weeks in combination with exercises was found to reduce pain in AT patients[12].
- Also, the use of higher heels footwear and possibly orthoses were found to have less load on Achilles tendon compared to lower heel and conventional footwear in runners[13].
- Theoretically, we could also apply that to children with Sever's disease to assist in reducing the tensile pull around that growing calcaneum[3].
MTP Joint Pathologies[edit | edit source]
MTP joint pathologies such as sesamoid problems, arthritic joints, hyper extensive injuries that are common in rugby and American football players.
- Depending on the pathology, foot orthoses can offload the area in case of sesamoiditis or offer support and reduce bending in case of capsular injuries[3].
Plantar Plate Injury, Metatarsalgia and Freiberg Disease[edit | edit source]
- A metatarsal dome can be used to shift the load away from the area of pain.
- The plantar plate could be used to reduce the reverse windlass phase time, therefore, reducing the tensile pull on the plantar fascia[3].
Prescribing Foot Orthoses[edit | edit source]
Time-frame[edit | edit source]
The fear of dependency and overuse is often associated with prescribing orthoses. In some conditions, foot orthoses are recommended for long term or for the lifetime of the patient such as in tibialis posterior dysfunction. However, in other conditions, it should only be used for the short term. for example, the patellofemoral pain guidelines recommended the use of foot orthoses for six weeks only[8].
Prefabricated vs Customized[edit | edit source]
Prefabricated or off-the-shelf, often bought on the internet or at pharmacies. They come in various types and shapes such as full length, forefoot cut-outs and carbon polymer shells, There are various models and designs which allow the clinician and patient to choose freely depending on the desired therapeutic effect.
Prefabricated are recommended first before trying customized as you can always apply adaptations and test the results[3]. A clinical adaptation to individualizing orthoses is tuning the dosage up or down to meet the demands and the patient's feedback[3], for example, lowering or increasing the heel height[6].
Several randomized controlled trials have shown prefabricated orthoses to have similar efficacy to customized orthoses in the management of plantar fasciitis[3]. A study found prefabricated orthoses better in comparison with customized orthoses in the treatment of plantar fasciitis pain[14]. Another study found no difference between the two types of orthoses for the same condition[15].
The Patellofemoral Pain 2019 guidelines reported insufficient evidence to recommend customized over prefabricated foot orthoses[8].
Regardless of the type of orthoses, there are considerations to put in mind when choosing the type and design of the orthoses:
- Bodyweight
- Patient's beliefs
- Current footwear
- Activities [3]
Also, good clinical reasoning, detailed history taking, shared decision and communication play an integral role in the success of foot orthoses. Depending on the condition, orthoses should be combined with other interventions with considerations to the time-frame to avoid dependency and overuse[3].
Why Do Some Clinicians Hesitate to Prescribe Foot Orthoses?[edit | edit source]
Some Healthcare professionals might be against the use of orthoses for the treatment of foot conditions. This might come from the fact that orthoses might have been overused over time and the common belief that orthoses contribute to weakening the muscles. However, if they're prescribed properly, tailored to the individual's needs and their condition they can be a useful tool combined with other interventions.[3]
An important point to consider is the difference between the use of orthoses in research and clinical practice, In some mechanical studies, customized orthoses are standardized and fabricated using scanning or casting method. Unlike in clinical practice, prescribing orthoses depends on the applied assessment of foot mechanics in the clinic, linking those findings to the presentation and applying corrections then testing their efficacy. [3]
In regards with muscle weakness, Jung et al [16] reported an increase in cross-sectional area of abductor hallucis and flexor hallucis muscles in subjects with Pes Planus with a combined foot orthosis and short-foot exercises for 8 weeks. Contrary, a 2017 study by Protopapas investigated the effect of a 12-week custom-made foot orthotic intervention on the intrinsic muscles of the foot and dynamic stability and found a significant reduction in the cross-sectional area of Flexor Digitorum Brevis, Abductor Digiti Minimi and Abductor Hallucis. The changes in the muscle size didn't affect the gait parameters and the dynamic stability which might indicate adaptations of these structures when off-loaded.[17]
References[edit | edit source]
- ↑ Fox JR, Lovegreen W. Lower Limb Orthoses. InAtlas of Orthoses and Assistive Devices 2019 Jan 1 (pp. 239-246). Content Repository Only!.
- ↑ Merriam Webster Dictionary. orthotic definition. Available from: https://www.merriam-webster.com/dictionary/orthotic (accessed 28 May 2020)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 Bruce K. Foot Orthoses: When, What and Why? course. Physioplus 2020.
- ↑ Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, McDonough CM, Altman RD, Beattie P, Cornwall M, Davis I. Heel pain—plantar fasciitis: revision 2014. Journal of Orthopaedic & Sports Physical Therapy. 2014 Nov;44(11):A1-33.
- ↑ Whittaker GA, Munteanu SE, Menz HB, Tan JM, Rabusin CL, Landorf KB. Foot orthoses for plantar heel pain: a systematic review and meta-analysis. Br J Sports Med. 2018 Mar 1;52(5):322-8.
- ↑ 6.0 6.1 Bishop C, Thewlis D, Hillier S. Custom foot orthoses improve first-step pain in individuals with unilateral plantar fasciopathy: a pragmatic randomised controlled trial. BMC musculoskeletal disorders. 2018 Dec 1;19(1):222.
- ↑ Rasenberg N, Riel H, Rathleff MS, Bierma-Zeinstra SM, van Middelkoop M. Efficacy of foot orthoses for the treatment of plantar heel pain: a systematic review and meta-analysis. British journal of sports medicine. 2018 Aug 1;52(16):1040-6.
- ↑ 8.0 8.1 8.2 Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM, Altman R, Beattie P. Patellofemoral pain: Clinical practice guidelines linked to the international classification of functioning, disability and health from the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. Journal of Orthopaedic & Sports Physical Therapy. 2019 Sep;49(9):CPG1-95.
- ↑ Vicenzino B, Collins N, Crossley K, Beller E, Darnell R, McPoil T. Foot orthoses and physiotherapy in the treatment of patellofemoral pain syndrome: a randomised clinical trial. BMC musculoskeletal disorders. 2008 Dec;9(1):27.
- ↑ Vicenzino B, Collins N, Cleland J, McPoil T. A clinical prediction rule for identifying patients with patellofemoral pain who are likely to benefit from foot orthoses: a preliminary determination. British journal of sports medicine. 2010 Sep 1;44(12):862-6.
- ↑ Matthews M, Rathleff MS, Claus A, McPoil T, Nee R, Crossley KM, Kasza J, Vicenzino BT. Does foot mobility affect the outcome in the management of patellofemoral pain with foot orthoses versus hip exercises? A randomised clinical trial. British Journal of Sports Medicine. 2020 Mar 25.
- ↑ Mayer F, Hirschmüller A, Müller S, Schuberth M, Baur H. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. British journal of sports medicine. 2007 Jul 1;41(7):e6-.
- ↑ Sinclair J, Richards J, Shore H. Effects of minimalist and maximalist footwear on Achilles tendon load in recreational runners. Comparative Exercise Physiology. 2015 Dec 7;11(4):239-44.
- ↑ Pfeffer G, Bacchetti P, Deland J, Lewis AI, Anderson R, Davis W, Alvarez R, Brodsky J, Cooper P, Frey C, Herhck R. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot & Ankle International. 1999 Apr;20(4):214-21.
- ↑ Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Archives of internal medicine. 2006 Jun 26;166(12):1305-10.
- ↑ Jung DY, Koh EK, Kwon OY. Effect of foot orthoses and short-foot exercise on the cross-sectional area of the abductor hallucis muscle in subjects with pes planus: a randomized controlled trial 1. Journal of back and musculoskeletal rehabilitation. 2011 Jan 1;24(4):225-31.
- ↑ Protopapas K. The Effects of a 12-Week Custom Foot Orthotic Intervention on the Intrinsic Muscles of the Foot, and Dynamic Stability During Unexpected Gait Termination in Healthy Young Adults.