Femoral stress fracture
Original Editors - Matthias Verstraelen as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Matthias Verstraelen, Lucinda hampton, Kim Jackson, Redisha Jakibanjar, Admin, Daniele Barilla, Adam Vallely Farrell, Wanda van Niekerk, Daphne Jackson, Laura Ritchie, Evan Thomas, Naomi O'Reilly, WikiSysop, Elise Audiens and Claire Knott
Definition/Description[edit | edit source]
The femur, as the largest bone in the body, has dozens of muscle origins and insertions, making it prone to stress injury at several locations. Stress injury denotes gradual structural compromise due to training overload. Stress fractures may be incomplete or complete, and either non-displaced or displaced. Femoral neck stress fractures are considered high-risk for complications, particularly displacement; whereas, femoral shaft stress fractures are low-risk.[1]
Stress fractures occur in bones that undergo mechanical fatigue.[2] They are a consequence of exceeding repetitive submaximal loads, which creates an imbalance between bone resorption and bone formation.[3]The fractures usually begin in locations of great stress; this is called “crack initiation”.[3] If this microscopic crack is not able to heal and is subjected to further loading, the microdamage will increase and the crack will enlarge. This increase in damage can cause the bone to break on a macroscopic level.[3]
The video below gives a good summary of femoral stress fracture diagnosis and treatment.
Stress fractures were first described in Prussian soldiers by Breithaupt in 1855. They were named “march fractures” and their characteristics were confirmed 40 years later with the advent of radiography.In 1958, Devas made the first report on stress fractures in athletes.[5]
Stress fractures are injuries that occur when repetitive and excessive stress on a bone is combined with limited rest. This leads to muscle weakness and a lower shock absorbing capacity of the leg[6][7][8][9][10].
Epidemiology[edit | edit source]
Femoral neck stress fractures make up approximately 11% of stress injuries in athletes. The patient complains of hip or groin pain which is worse with weight bearing and range of motion especially internal rotation. There are 2 types of femoral neck stress fractures: tension-type (or distraction) fractures and compression-type fractures. Tension-type femoral neck stress fractures involve the superior-lateral aspect of the neck and are at highest risk for complete fracture; thus, these should be detected early. Compression-type fractures are seen in younger athletes and involve the inferior-medial femoral neck. A trial of non-surgical management can be attempted for patients without a visible fracture line on radiographs in compression type injuries. This injury is common in runners.
Stress fractures of the femoral shaft are well documented in the literature, and in one study among military recruits, they represented 22.5% of all stress fractures. Patients typically complain of poorly localised, insidious leg pain often mistaken for muscle injury. An exam is often non-focal, although the “fulcrum test” test can be used by providers to localise the affected pain and suggest the diagnosis. If there is no evidence of a cortical break on imaging, a non-surgical approach can be attempted.[11]
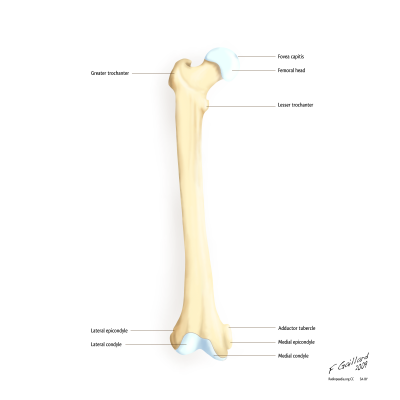
Clinically Relevant Anatomy[edit | edit source]
Stress fractures of the femur can occur in the whole bone like the neck, shaft and the condyles.Femoral stress fractures mainly develop on the medial compression side of the femoral shaft, within the proximal and middle thirds of the bone. [12]The highest incidence is seen at the femoral neck.
When the patient doesn’t adapt his or her training, certain stress fractures could lead to complications, even to the point of complete femoral fractures of the head or shaft [13][14].
Risk Factors[edit | edit source]
The risk factors are as follows: [15][6][7][16]
- High-intensity training
- Recreational runners
- Track and field, basketball, soccer, dance
- Women
- Poor nutrition and lifestyle activities
- Lower 25-hydroxyvitamin D
- Female athlete triad
- (history of) smoking
- < 3 times exercising/week
- > 10 alcoholic drinks/week
- Genetic factors [17]
- Change of surfaces (indoor track, frozen field)
- Biomechanical imbalance (leg length, foot arch, forefoot varus, stance of foot and ankle)
Signs and Symptoms[edit | edit source]
- Local pain and oedema
- Point tenderness on palpation
- Local swelling
- Antalgic gait
- Painful and limited passive and active ROM of hip and/or knee (flexion, internal rotation, extension)
- Pain increases during activity
- Groin pain
- Bone marrow oedema
Outcome Measures[edit | edit source]
The hop test and tuning fork test could be used as diagnostic test but there is a lack of recent evidence for their validity. Another test is the “fist” test, the therapist create a bilateral pressure on the anterior side of the femur starting at the distal part and moving to the proximal one. The most valid test for the diagnosis is the fulcrum-test, while the therapist pushes to the dorsum of the knee [18].
Differential Diagnosis[edit | edit source]
- muscle strain (quadriceps )
- illiopsoas tendinopathy, see relevant section in link [19].
Diagnostic Procedures[edit | edit source]
We can use 4 modalities, these techniques can be used in different phases of diagnosis and treatment [15][17]
- plain radiography,
- bone scan
- MRI (has the highest sensitivity and specificity [15]
- ultrasonography
Physical Therapy Management[edit | edit source]
Conservative Treatment (NOF stress fracture)
If conservative management is chosen, then the patient should be limited weight-bearing with crutches until they are completely free of pain. This normally takes between 6 to 8 weeks but can be up to 14 weeks. During this time, weight-bearing through the injured side can be gradually increased from non-weight-bearing to toe-touch weight bearing to partial weight-bearing, as pain allows.[20]
Upper limb conditioning can be initiated. Hydrotherapy can be undertaken, wearing an inflatable jacket for support. Lower-limb athletic activity should be commenced only when there is clear evidence of fracture union, both radiologically and clinically . Activity is normally commenced in a graduated manner, around 12 weeks, specifically focussing on strengthening and range-of-motion exercises around the hip. Patient should begin with a gentle running programme, which should be increased in intensity over 6 to 8 weeks, ensuring the patient remains pain-free throughout. Return to full sport can normally be achieved between 3 and 6 months after injury, though this can require up to a year if not longer.
Surgical intervention
If NOF surgery was required post-operatively, the patient should remain non- to toe-touch weight-bearing with crutches for 6 weeks, followed by partial weight-bearing with crutches for a further 6 weeks . After this, weight-bearing is permitted as tolerated. Rehabilitation can then follow the above guideline for conservative management.
Ivkovic et al. designed a new treatment algorithm for femoral shaft stress injuries. Four phases have to be fulfilled to start normal training and each phase is evaluated by a hop or fulcrum test. The first phase is called symptomatic, where the patient has to walk with crutches. The second phase is the asymptomatic one where patient are allowed to walk normally and to start swimming and exercises the upper extremity. During the third ‘basic’ phase the patient can perform exercises of lower and upper extremities. During the last ‘resuming phase’, the athlete is allowed to gradually start normal training [18]. No recurrence of injury after treatment and follow-up for 48-96 months [18].The treatment algorithm is free available in the article from Ivkovic et al.: "Stress fractures of the femoral shaft in athletes: a new treatment algorithm."
A triple-phase bone scan is recommended for an early diagnosis. It is very important to perform an adequate evaluation, patient history, and have a high index of suspicion. This will enable the practitioner to justify having a bone scan performed and thereby decrease the incidence of undiagnosed asymptomatic femoral shaft stress fractures. [21]
An early diagnosis is needed. Often, x-rays are not going to detect these injuries. Therefore, we must go through the appropriate referral channels to have a triple-phase bone scan ordered. One needs to maintain a high level of suspicion, especially if the athlete is experiencing persistent pain that shows no improvement with treatment.[21]
Prevention[edit | edit source]
To prevent femoral stress fractures, people could modify their training schedules and wear shock-absorbing shoe inserts. Insoles lowers the incidence because the improves biomechanics, less fatigue and limit the impact on the ground. The size of these insoles can range in different types to support the forefoot and/or the toes [7][22]. Also calcium and vitamin D supplementation could play a role in the prevention but their data are controversial [22]. Leg muscle stretching during warm-up has no significant effect on prevention for femoral stress fractures[15].
References[edit | edit source]
- ↑ Jackson J, Asplund CA. Femoral stress fractures in adults. Available from: https://www.uptodate.com/contents/femoral-stress-fractures-in-adults (last accessed 2.12.2019)
- ↑ Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of running speed on a probabilistic stress fracture model. Clinical Biomechanics. 2010;25:372-377.
- ↑ 3.0 3.1 3.2 Maffulli N, Longo UG, Denaro V. Femoral Neck Stress Fractures. Operative Techniques in Sports Medicine. 2009;17:90-93.
- ↑ UC San Diego Health Sports related stress fractures Available from: https://www.youtube.com/watch?v=Eev1LxCNepM (last accessed 2.12.2019)
- ↑ Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini AD, Ejnisman B. Stress fractures: definition, diagnosis and treatment. Revista brasileira de ortopedia. 2016 Feb;51(1):3-10.
- ↑ 6.0 6.1 Stress Fractures, information from your family doctor. Americain Family Physician Jan. 2011. Level of evidence: 5
- ↑ 7.0 7.1 7.2 Zadpoor A, Nikooyan A. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical Biomechanics 2011; 26: 23 -28. (level of evidence 3A)
- ↑ 8.0 8.1 Niva M, Mattila V, Kiuru M, Pihlajamäki H. Bone stress Injuries are common in female military trainees. Clin Orthop Relat Res (2009) 467: 2962-2969. Level of evidence: 3A
- ↑ 9.0 9.1 Schultz, Houglum, Perrin. Third edition, examination of musculoskeletal injuries p.401. Human Kinetics. Level of evidence: 5
- ↑ Houglum P. Second edition, therapeutic exercise for musculoskeletal injuries p.80-81, p. 811-812. Human Kinetics. Level of evidence: 5
- ↑ Kiel J, Kaiser K. Stress reaction and fractures. InStatPearls [Internet] 2019 Jun 4. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507835/ (last accessed 2.12.2019)
- ↑ Robertson GA, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World journal of orthopedics. 2017 Mar 18;8(3):242.
- ↑ Patel D, Roth M, Kapil N. Stress fractures: diagnosis, treatment and prevention. American Family Physician Jan. 2011; 83: 39-46. Level of evidence: 1A
- ↑ Zadpoor A, Nikooyan A. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical Biomechanics 2011; 26: 23 -28. Level of evidence: 1B
- ↑ 15.0 15.1 15.2 15.3 Patel D, Roth M, Kapil N. Stress fractures: diagnosis, treatment and prevention. American Family Physician Jan. 2011; 83: 39-46. (Level of evidence 1A)
- ↑ 16.0 16.1 Anand A, Raviraj A, Kodikal G. Subchondral stress fractures of femoral head in healthy adult. Indian J Orthop. 2010 Oct-Dec; 44(4): 458-460. Level of evidence: 3B
- ↑ 17.0 17.1 Korvala J, Hartikka H, Pihlajamäki H, Solovieva S, Ruohola J-P, Sahi T, Barral S, Ott J, Ala-Kokko L, Männikkö M. Genetic predisposition for femoral neck stress fractures in military conscripts. BMC Genetics 2010, 11: 95. Level of evidence: 2B
- ↑ 18.0 18.1 18.2 18.3 Ivkovic A, Bojanic I, Pecina M. Stress fractures of the femoral shaft in athletes: a new treatment algorithm. Br J Sports Med 2006; 40: 518-520. (Level of evidence 2A)
- ↑ Nguyen J, Peterson J, Biswal S, Beaulieu C, Fredericson M. Stress-related injuries around the lesser trochanter in long-distance runners. AJR 2008; 190: 1616-1620. Level of evidence: 3B
- ↑ Robertson GA, Wood AM. Femoral neck stress fractures in sport: a current concepts review. Sports medicine international open. 2017 Feb;1(02):E58-68. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226070/ (last accessed 2.12.2019)
- ↑ 21.0 21.1 Mark Casterline, M. A. (March 1996). Femoral Stress Fracture. Journal Of Athletic Training, 55-56 (level of evidence 4).
- ↑ 22.0 22.1 Snyder R, De Angelis J, Koester M., Spindler K, Dunn W. Does shoe insole modification prevent stress fractures? A systematic review. HSSJ (2009) 5: 92-98. (Level of evidence 2B)