Femoral stress fracture
Original Editors - Matthias Verstraelen as part of the Vrije Universiteit Brussel's Evidence-based Practice project
Top Contributors - Matthias Verstraelen, Lucinda hampton, Kim Jackson, Redisha Jakibanjar, Daniele Barilla, Adam Vallely Farrell, Admin, Daphne Jackson, Wanda van Niekerk, WikiSysop, Elise Audiens, Claire Knott, Laura Ritchie, Evan Thomas and Naomi O'Reilly
Definition/Description[edit | edit source]
Stress fractures occur in bones that undergo mechanical fatigue.[1] They are a consequence of exceeding repetitive submaximal loads, which creates an imbalance between bone resorption and bone formation.[2]The fractures usually begin in locations of great stress; this is called “crack initiation”.[2] If this microscopic crack is not able to heal and is subjected to further loading, the microdamage will increase and the crack will enlarge. This increase in damage can cause the bone to break on a macroscopic level.[2]
Stress fractures may be due to multiple factors including activity level, bone quality, anti-inflammatory drugs, radiation, nutritional status, osteoporosis, imbalanced hormones, sleep deprivation, and collagen anomalies. The frequency of stress fractures is dependent upon the composition of bone, adjacent muscle attachments, the vasculature, systemic factors, and the mode of athletic activity.[2] Other possible risks include age, sex, footwear, and training regimen.[3] High level female athletes who are inclined to the athlete triad (amenorrhea, eating disorders, and osteoporosis) and male endurance athletes who have unusually low levels of sex hormones are also at risk for stress fractures.[2]
Stress fractures were first described in Prussian soldiers by Breithaupt in 1855. They were named “march fractures” and their characteristics were confirmed 40 years later with the advent of radiography.In 1958, Devas made the first report on stress fractures in athletes.[4]
Stress fractures are injuries that occur when repetitive and excessive stress on a bone is combined with limited rest. This leads to muscle weakness and a lower shock absorbing capacity of the leg[5][6][7][8][9].
Epidemiology[edit | edit source]
Femoral stress fractures are relatively uncommon. They comprise of between 1 and 25% of all stress fractures.[10][11][12][13] The overall incidence is not widely known, observational studies have reported a higher incidence in athletes participating in distance running. While smaller studies have identified that femoral stress fractures are more common in military trainees than athletes.[14][15] Femoral neck injuries are more common than femoral shaft stress fractures, although this finding has not been consistent[16][17].
Overuse Femoral stress fractures have been diagnosed in patients from age five to physically active adults in their 50s and 60s.[18][19] The large majority of studies have involved athletes and military recruits in their late teens and early 20's, and the majority of subjects are male.[20]
Femoral stress fractures are most commonly associated with running.[19] A systematic review of the risk of femoral stress fractures identified two major risk factors: female gender and a previous history of stress fracture.[21] Female athletes and female military recruits are thought to be at the highest risk of femoral stress fractures due to a lower body mass and a lower bone mineral density than their male counterparts. Those with amenorrhea or poor aerobic baseline fitness prior to starting military training are at particular higher risk. Femoral stress fractures also occur in those that are overweight with limited participation in sport.
Clinically Relevant Anatomy[edit | edit source]
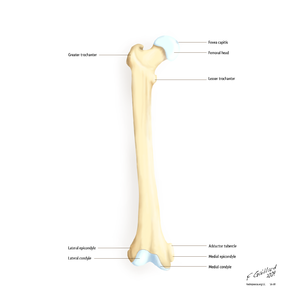
The femur is the most proximal bone of the leg. The femur consists of a head, greater and lesser trochanter, shaft, and lateral and medial condyles with the patellar surface in between. The head of the femur articulates with the acetabulum in the pelvic bone forming the hip joint while the distal part of the femur articulates with the tibia and kneecap forming the knee joint. By most measures the femur is the strongest bone in the body. The femur is also the longest bone in the body. [11]
The femur is the only bone in the thigh, it serves as an attachment point for all the muscles that exert their force over the hip and knee joints. Some bi-articular muscles, which cross two joints, like the gastrocnemius and plantaris muscles, also originate from the femur.[22]
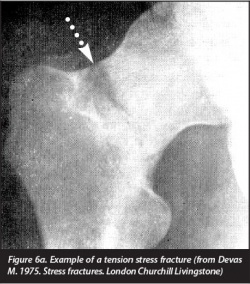
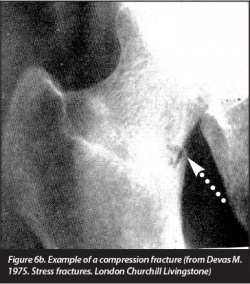
Stress fractures of the femur can occur in the whole bone like the neck, shaft and the condyles.Femoral stress fractures mainly develop on the medial compression side of the femoral shaft, within the proximal and middle thirds of the bone. [23]The highest incidence is seen at the femoral neck. When the patient doesn’t adapt his or her training, certain stress fractures could lead to complications, even to the point of complete femoral fractures of the head or shaft [24][25].
Characteristics/Clinical Presentation[edit | edit source]
The risk factors are as follows: [26][5][6][27]
- High-intensity training
- Recreational runners
- Track and field, basketball, soccer, dance
- Women
- Poor nutrition and lifestyle activities
- Lower 25-hydroxyvitamin D
- Female athlete triad
- (history of) smoking
- < 3 times exercising/week
- > 10 alcoholic drinks/week
- Genetic factors [28]
- Change of surfaces (indoor track, frozen field)
- Biomechanical imbalance (leg length, foot arch, forefoot varus, stance of foot and ankle)
There is a trend to significance for energy expenditure (kcal/day) with lower limb stress fractures (p=0.06). This effect could be explained as a sequence that more active people have also a higher expenditure level [29].
No significant effect is found of the ground reaction force on the incidence of lower-limb stress fractures (p>0.05) [6].
The incidence of femoral stress fractures is reduced with 14% (p=0.013) when a semi rigid insole is used [30].
Alana et al. concluded that there’s no effect on lower limb stress fractures and calcium intake (p=0.55) or bone density [29].
There is a trend to significance for energy expenditure (kcal/day) with lower limb stress fractures (p=0.06). This effect could be explained as a sequence that more active people have also a higher expenditure level [29].
Diagnostic Procedures[edit | edit source]
First of all we describe the possible symptoms: [27][7][31][8]
- Local pain and edema
- Point tenderness on palpation
- Local swelling
- Antalgic gait
- Painful and limited passive and active ROM of hip and/or knee (flexion, internal rotation, extension)
- Pain increases during activity
- Groin pain
- Bone marrow edema
The hop test and tuning fork test could be used as diagnostic test but there is a lack of recent evidence for their validity. Another test is the “fist” test, the therapist create a bilateral pressure on the anterior side of the femur starting at the distal part and moving to the proximal one. The most valid test for the diagnosis is the fulcrum-test, while the therapist pushes to the dorsum of the knee [31].
Fulcrum test
Therapists have to pay attention to misdiagnose a femoral stress fracture as muscle strain of the quadriceps or illiopsoas tendinopathy because of the similar symptoms [33].
To present femoral stress fractures on images. We can use 4 modalities: plain radiography, bone scintigrapy, MRI and ultrasonography with the highest sensitivity and specificity for MRI [26]. These techniques can be used in different phases of diagnosis and treatment [26][28].
Classification of lower limb stress fracture [4][34][edit | edit source]
| Arendt scale (MRI based) | Federicson scale (MRI based) | Saxen classification | Torg classification (radiographic based) | |
|---|---|---|---|---|
| Location of use | Generic | Generic | Navicular | 5th Metatarsal base |
| Grade 1 | STIR signal change | Periosteal edema - bone marrow normal | Dorsal cortex involved | Acute fracture line, no intramedullary sclerosis or periosteal reaction |
| Grade 2 | STIR and T2 change | Periosteal and bone marrowedema - T2 change only | Dorsal cortex and body involved | Widened fracture line with intramedullary sclerosis and periosteal reaction |
| Grade 3 | STIR, T1 and T2 change - no fracture line present | Periosteal and bone marrow edema - T1 and t2 change - no fracture line | Dorsal and volar cortices uninvolved | Widened fracture line with complete intramedullary sclerosis and periosteal reaction |
| Grade 4 | STIR, T1 and T2 change - fracture line present | Periosteal and bone marrow edema - STIR, T1 and T2 change - fracture line | - | - |
*MRI: Magnetic resonance imaging; CT: Computed tomography; STIR: Short tau inversion recovery.
Examination[35]
The hop test and tuning fork test could be used as diagnostic test but there is a lack of recent evidence for their validity. Another test is the “fist” test, the therapist create a bilateral pressure on the anterior side of the femur starting at the distal part and moving to the proximal one. The most valid test for the diagnosis is the fulcrum-test, while the therapist pushes to the dorsum of the knee [31].
Physical Therapy Management[edit | edit source]
Initial treatment is based on the reduction of activities to a pain-free level. During this “relative rest”-period of 4 to 12 weeks, the patient can use pneumatic compression walking boots to reduce his pain level. Also, physical therapy and cross-training which contains of flexibility, strength and cardiovascular training is permitted for example swimming and biking. After that restriction period, the activities can be increased in a slow, graduated way [30].
Ivkovic et al. designed a new treatment algorithm for femoral shaft stress injuries. Four phases have to be fulfilled to start normal training and each phase is evaluated by a hop or fulcrum test. The first phase is called symptomatic, where the patient has to walk with crutches. The second phase is the asymptomatic one where patient are allowed to walk normally and to start swimming and exercises the upper extremity. During the third ‘basic’ phase the patient can perform exercises of lower and upper extremities. During the last ‘resuming phase’, the athlete is allowed to gradually start normal training [31]. No recurrence of injury after treatment and follow-up for 48-96 months [31].The treatment algorithm is free available in the article from Ivkovic et al.: "Stress fractures of the femoral shaft in athletes: a new treatment algorithm."
A triple-phase bone scan is recommended for an early diagnosis. It is very important to perform an adequate evaluation, patient history, and have a high index of suspicion. This will enable the practitioner to justify having a bone scan performed and thereby decrease the incidence of undiagnosed asymptomatic femoral shaft stress fractures. [37]
An early diagnosis is needed. Often, x-rays are not going to detect these injuries. Therefore, we must go through the appropriate referral channels to have a triple-phase bone scan ordered. One needs to maintain a high level of suspicion, especially if the athlete is experiencing persistent pain that shows no improvement with treatment.[37]
To prevent femoral stress fractures, people could modify their training schedules and wear shock-absorbing shoe inserts. Insoles lowers the incidence because the improves biomechanics, less fatigue and limit the impact on the ground. The size of these insoles can range in different types to support the forefoot and/or the toes [6][30]. Also calcium and vitamin D supplementation could play a role in the prevention but their data are controversial [30]. Leg muscle stretching during warm-up has no significant effect on prevention for femoral stress fractures[26].
References[edit | edit source]
- ↑ Edwards WB, Taylor D, Rudolphi TJ, Gillette JC, Derrick TR. Effects of running speed on a probabilistic stress fracture model. Clinical Biomechanics. 2010;25:372-377.
- ↑ 2.0 2.1 2.2 2.3 2.4 Maffulli N, Longo UG, Denaro V. Femoral Neck Stress Fractures. Operative Techniques in Sports Medicine. 2009;17:90-93.
- ↑ Korpelainen R, Orava S, Karpakka J, Siira P, Hulkko A. Risk Factors for Recurrent Stress Fractures in Athletes. American Orthopaedic Society for Sports Medicine. 2001;29(3):304-310.
- ↑ 4.0 4.1 Astur DC, Zanatta F, Arliani GG, Moraes ER, Pochini AD, Ejnisman B. Stress fractures: definition, diagnosis and treatment. Revista brasileira de ortopedia. 2016 Feb;51(1):3-10.
- ↑ 5.0 5.1 Stress Fractures, information from your family doctor. Americain Family Physician Jan. 2011. Level of evidence: 5
- ↑ 6.0 6.1 6.2 6.3 Zadpoor A, Nikooyan A. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical Biomechanics 2011; 26: 23 -28. (level of evidence 3A)
- ↑ 7.0 7.1 Niva M, Mattila V, Kiuru M, Pihlajamäki H. Bone stress Injuries are common in female military trainees. Clin Orthop Relat Res (2009) 467: 2962-2969. Level of evidence: 3A
- ↑ 8.0 8.1 Schultz, Houglum, Perrin. Third edition, examination of musculoskeletal injuries p.401. Human Kinetics. Level of evidence: 5
- ↑ Houglum P. Second edition, therapeutic exercise for musculoskeletal injuries p.80-81, p. 811-812. Human Kinetics. Level of evidence: 5
- ↑ Matheson GO, Clement DB, McKenzie DC, et al. Stress fractures in athletes. A study of 320 cases. Am J Sports Med 1987; 15:46.
- ↑ Brukner P, Bradshaw C, Khan KM, et al. Stress fractures: a review of 180 cases. Clin J Sport Med 1996; 6:85.
- ↑ Johnson AW, Weiss CB Jr, Wheeler DL. Stress fractures of the femoral shaft in athletes--more common than expected. A new clinical test. Am J Sports Med 1994; 22:248.
- ↑ Volpin G, Hoerer D, Groisman G, et al. Stress fractures of the femoral neck following strenuous activity. J Orthop Trauma 1990; 4:394.
- ↑ Niva MH, Kiuru MJ, Haataja R, Pihlajamäki HK. Fatigue injuries of the femur. J Bone Joint Surg Br 2005; 87:1385.
- ↑ DeFranco MJ, Recht M, Schils J, Parker RD. Stress fractures of the femur in athletes. Clin Sports Med 2006; 25:89.
- ↑ Changstrom BG, Brou L, Khodaee M, et al. Epidemiology of stress fracture injuries among US high school athletes, 2005-2006 through 2012-2013. Am J Sports Med 2015; 43:26.
- ↑ Clement DB, Ammann W, Taunton JE, et al. Exercise-induced stress injuries to the femur. Int J Sports Med 1993; 14:347.
- ↑ Clough TM. Femoral neck stress fracture: the importance of clinical suspicion and early review. Br J Sports Med 2002; 36:308.
- ↑ 19.0 19.1 Matheson GO, Clement DB, McKenzie DC, et al. Stress fractures in athletes. A study of 320 cases. Am J Sports Med 1987; 15:46.
- ↑ Jacobs JM, Cameron KL, Bojescul JA. Lower extremity stress fractures in the military. Clin Sports Med 2014; 33:591.
- ↑ Wright AA, Taylor JB, Ford KR, et al. Risk factors associated with lower extremity stress fractures in runners: a systematic review with meta-analysis. Br J Sports Med 2015; 0:1.
- ↑ Aukerman DF. Femur injuries and fractures. http://emedicine.medscape.com/article/90779-overview
- ↑ Robertson GA, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World journal of orthopedics. 2017 Mar 18;8(3):242.
- ↑ Patel D, Roth M, Kapil N. Stress fractures: diagnosis, treatment and prevention. American Family Physician Jan. 2011; 83: 39-46. Level of evidence: 1A
- ↑ Zadpoor A, Nikooyan A. The relationship between lower-extremity stress fractures and the ground reaction force: a systematic review. Clinical Biomechanics 2011; 26: 23 -28. Level of evidence: 1B
- ↑ 26.0 26.1 26.2 26.3 Patel D, Roth M, Kapil N. Stress fractures: diagnosis, treatment and prevention. American Family Physician Jan. 2011; 83: 39-46. (Level of evidence 1A)
- ↑ 27.0 27.1 Anand A, Raviraj A, Kodikal G. Subchondral stress fractures of femoral head in healthy adult. Indian J Orthop. 2010 Oct-Dec; 44(4): 458-460. Level of evidence: 3B
- ↑ 28.0 28.1 Korvala J, Hartikka H, Pihlajamäki H, Solovieva S, Ruohola J-P, Sahi T, Barral S, Ott J, Ala-Kokko L, Männikkö M. Genetic predisposition for femoral neck stress fractures in military conscripts. BMC Genetics 2010, 11: 95. Level of evidence: 2B
- ↑ 29.0 29.1 29.2 Cline A, Jansen R, Melby C. Stress fractures in female army recruits: implications of bone density, calcium intake and exercise. Journal of the American College of Nutrition, Vol. 17; No. 2: 128-135 (1998). Level of evidence: 3A
- ↑ 30.0 30.1 30.2 30.3 Snyder R, De Angelis J, Koester M., Spindler K, Dunn W. Does shoe insole modification prevent stress fractures? A systematic review. HSSJ (2009) 5: 92-98. (Level of evidence 2B)
- ↑ 31.0 31.1 31.2 31.3 31.4 Ivkovic A, Bojanic I, Pecina M. Stress fractures of the femoral shaft in athletes: a new treatment algorithm. Br J Sports Med 2006; 40: 518-520. (Level of evidence 2A)
- ↑ Fulcrum Test | Femoral Stress Fractures Available from: https://www.youtube.com/watch?v=k2vDNa7hW2c
- ↑ Nguyen J, Peterson J, Biswal S, Beaulieu C, Fredericson M. Stress-related injuries around the lesser trochanter in long-distance runners. AJR 2008; 190: 1616-1620. Level of evidence: 3B
- ↑ Robertson GA, Wood AM. Lower limb stress fractures in sport: Optimising their management and outcome. World journal of orthopedics. 2017 Mar 18;8(3):242.
- ↑ Casterline M, Osowski S, Ulrich G. Femoral stress fracture. Journal of Athletic Training March 1996; 31: 53-56. Level of evidence: 4
- ↑ BJSM Videos. Stress fracture (fulcrum) test, with Mike Reiman. Available from: http://www.youtube.com/watch?v=8Dw3fNd5Szc [last accessed 25/01/14]
- ↑ 37.0 37.1 Mark Casterline, M. A. (March 1996). Femoral Stress Fracture. Journal Of Athletic Training, 55-56 (level of evidence 4).