Femoral Fractures
Top Contributors - Margaux Jacobs, Kim Jackson, Vanderpooten Willem, Lucinda hampton, Admin, Vidya Acharya, Nupur Smit Shah, Jentel Van De Gucht, Rachael Lowe, Alex Palmer, Daphne Jackson, Margaux Jacobs, Jason Coldwell, Aminat Abolade, WikiSysop, Lauren Lopez, 127.0.0.1 and Evan Thomas
Definition/Description[edit | edit source]
A femoral fracture is a fracture of the thigh bone. A femoral shaft fracture is defined as a fracture of the diaphysis occurring between 5 cm distal to the lesser trochanter and 5 cm proximal to the adductor tubercleIt occurs by chronic, repetitive activity that is common to runners and military. These injuries must be differentiated from insufficiency fractures, which, though similar in appearance and presentation, result from an entirely different pathophysiology and occur in a different population.[1]The femur is the largest and strongest bone in the body and has a good blood supply, so it requires a large or high impact force to break this bone.There are 4 types of fracture:
• Type 1: stress fracture
• Type 2: severe impaction fractures
• Type 3: partial fracture
• Type 4: completed displaced fracture
This classification is for the severity of the fracture.
Type 1: stress fracture
A stress fracture is a small crack in the bone. Stress fractures often develop from overuse, such as from high-impact sports. Most stress fractures occur in the weight-bearing bones. A stress fracture is an overuse injury. When muscles are overtired, they are no longer able to lessen the shock of repeated impacts. When this happens, the muscles transfer the stress to the bones. This can create small cracks or fractures. [2]
Type 2: Severe impaction fractures
An impacted fracture is a fracture in which the bone breaks into multiple fragments, which are driven into each other. It is a closed fracture that occurs when pressure is applied to both ends of the bone, causing it to split into two fragments that jam into each other. [3]

Source: Houston Spine and Joint
Type 3: partial fracture
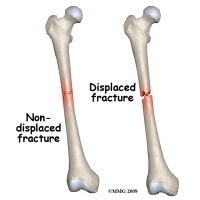
A partial fracture is an incomplete break of a bone. This type of fracture refers to the way the bone breaks. In an incomplete fracture the bone cracks but doesn’t break all the way through. In contrast there is the complete fracture, where the bone snaps into two or more parts.[4][5]

Source: Houston Spine and Joint
Type 4: completed displaced fracture
A bone has a displaced fracture when it breaks in two or more pieces and is no longer correctly aligned. Displacement of fractures is defined in terms of the abnormal position of the distal fracture fragment in relation to the proximal bone. [6]
Source: Radiology Masterclass
Femoral fractures can be located at three different places:
Femoral head fracture:
Femoral head stress fractures are a common cause of hip pain in select populations. Chronic, repetitive activity that is common to runners and military recruits, predisposes these populations to femoral neck stress fractures. [7]
Source: Journal of the American Academy of Orthopaedic Surgeons
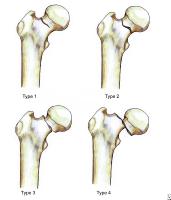
Head fractures: The Pipkin classification.
A: Type I, femoral head fracture inferior to the fovea centralis
B: Type II, fracture extended superior to the fovea centralis
C: Type III, any femoral head fracture with an associated femoral neck fracture
D: Type IV, any femoral head fracture with an associated acetabular fracture
Femoral shaft fracture:
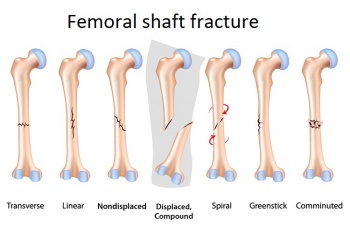
A femoral shaft fracture is defined as a fracture of the diaphysis occurring between 5 cm distal to the lesser trochanter and 5 cm proximal to the adductor tubercle. Femoral shaft fractures occur most frequently in young men after high-energy trauma and elderly women after a low-energy fall [8]
Keany (2013) describes 3 types of femoral shaft fractures as follows:
Type I - Spiral or transverse (most common)
Type II – Comminuted
Type III - Open [9]
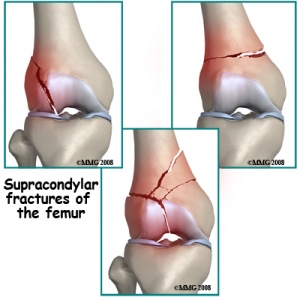
Femoral condyle fracture:
It occurs sometimes after a medial hamstring tendon ACL reconstruction with extra-articulartenodesis. The fracture occurs between the site of fixation of the extra-articular augmentation and the intraosseous femoral tunnel used in the intra-articular reconstruction [10]
Source : Alliance Physical Therapy
Clinically relevant anatomy[edit | edit source]
Osteology[edit | edit source]
The femur thigh bone, is the most proximal (closest to the hip joint) bone of the leg. The femur consists of a head, greater and lesser trochanter, shaft, and lateral and medial condyles with the patellar surface in between. The head of the femur articulates with the acetabulum in the pelvic bone forming the hip joint while the distal part of the femur articulates with the tibia and kneecap forming the knee joint. By most measures the femur is the strongest bone in the body. The femur is also the longest bone in the body. [11]
Musculature[edit | edit source]
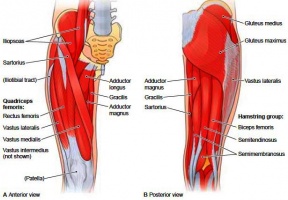
The femur is the only bone in the thigh, it serves as an attachment point for all the muscles that exert their force over the hip and knee joints. Some bi-articular muscles, which cross two joints, like the gastrocnemius and plantarismuscles, also originate from the femur. [12]
- Quadriceps: rectus femoris muscle, vastus lateralis muscle, vastus medialis muscle, vastus intermedius muscle
- Iliacus muscle (insertion on the lesser trochanter)
- Psoas major muscle (Insertion on the lesser trochanter)
- Adductors: Adductos longus muscle, adductor brevis muscle, adductor magnus muscle, pectineus muscle, gracilis muscle
- Popliteus muscle (insertion under the lateral epicondyle)
- Gastrocnemius muscle (Behind the adductor tubercle, over the lateral epicondyle and the popliteal facies)
- Plantaris muscle (over the lateral condyle)
- Abductors: tensor fasciae latae muscle
- Hamstrings: biceps femoris muscle, semimembranosus muscle, semitendinosus muscle
- Gluteus muscles: insertion on the greater trochanter
- Piriformis muscle: insertion on the superior boundary of greater trochanter
- Gemellus superior muscle, gemellus inferior muscle, obturator internus muscle, obturator externus muscle, quadratus femoris muscle
Source picture: https://saveourbones.com/weekend-challenge-the-hip-bone-protector/
Following a femoral fracture, according to Keller et al., most of these muscles are much weaker than before, so physiotherapy is very important for muscle strengthening.
Several large muscles attach to the femur. Proximally, the gluteus medius and minimus attach to the greater trochanter, resulting in abduction of the femur with fracture. The iliopsoas attaches to the lesser trochanter, resulting in internal rotation and external rotation with fractures. The lineaaspera (rough line on the posterior shaft of the femur) reinforces the strength and is an attachment for the gluteus maximus, adductor magnus, adductor brevis, vastus lateralis, vastus medialis, vastus intermedius, and short head of the biceps. Distally, the large adductor muscle mass attaches medially, resulting in an apex lateral deformity with fractures. The medial and lateral heads of the gastrocnemius attach over the posterior femoral condyles, resulting in Flexion deformity in distal-third fractures. [13] Also the dysfunction or atrophy of the muscles such as abductors, iliopsoas, adductors, gastrocnemius and tensor fascia lata can be a initiating point leading to femoral shaft fracture.
Epidemiology/Etiology[edit | edit source]
Fractures of the femoral shaft are caused by a high-energy injury, such as a road traffic accident, unless a pathological fracture in a patient with osteoporosis or metastatic disease. They are often associated injuries to the hip, pelvis, knee and other parts of the body.
Fractures vary in degree and complexity, depending on the degree of force involved. They may be: transverse (horizontally across the shaft), oblique, spiral (due to a twisting force), comminuted (when there are three or more resulting bone pieces), open or closed. [13][14]
The incidence of femoral fractures is reported as 1-1.33 fractures per 10,000 population per year in the USA. In the United States and Europe the incidence of femoral fractures in children comprise 20 per 100,000 yearly. In individuals younger than 25 years and those older than 65 years, the rate of femoral fractures is 3 fractures per 10,000 population annually. [15]
Their incidence is in constant increase probably due to the demographic modifications and the continuous increment of the average life of the population and therefore the presence of a higher number of elderly patients. The reduction of BMD related to age is the main factor which exposes elderly people to a greater risk of hip fracture. Hip fractures are strongly associated with BMD in the proximal femur, but there are also many clinical predictors of hip fracture risk that are independent of bone density. Hip fracture incidence was 17 times greater among 15% of the women who had five or more of the risk factors, exclusive of bone density, compared with 47% of the women who had two risk factors or less. However, the women with five or more risk factors had an even greater risk of hip fracture if their bone density Z score was in the lowest tertile.][16][17]
Several factors are related to increased risk of femoral fracture. Older persons (over 70) have a higher incidence of femoral fracture. A fracture of the proximal femoral is common in the elderly, with special emphasis on intracapsular (of the femoral neck) and extracapsular (trantrochanteric and subtrochanteric). Persons with Osteoporosis are also more likely to break their femur.[18]
The risk of these fractures increases exponentially with the increase of age and is higher in women (male-female ratio). Because women have more bone loss and falls than men, their incidence of hip fractures is about twice that seen in men at any age in the USA and Europe. Furthermore, women live longer than men so that more than three-quarters of all hip fractures occur in women. [19][20]
Morbidity and mortality rates have been reduced in femoral shaft fractures, mainly as the result of changes in methods of fracture immobilization. Current therapies allow for early mobilization, thus reducing the risk of complications associated with prolonged bed rest.
Characteristics/Clinical presentation[edit | edit source]
A broken thigh bone is almost always very obvious. Signs of a fracture include severe pain, inability to move the leg or stand on it,marked limitation of hip movements, local swelling and bruised skin. Typical for femoral neck and trochanteric fractures is the external rotation and the shortened lower limb, but both signs are less pronounced in a femoral neck fracture. Trochanteric fractures tend to cause more pain. Pain at the trochanteric area speaks in favor of a trochanteric fracture, whereas pain in the groin is typical of a neck fracture. [21]
In neck or trochanteric fractures an anterior angulation at the fracture site, a recurvatum, may be present.[22] The absence of external rotation is rather seen in an undisplaced fracture, a shortened leg suggests the fracture is displaced. Yet limb shortening is not seen in fractures displaced in valgus and the limb might even be slightly longer. There may also be a resultant loss of blood in the femur and a haematoma may be present in the surrounding soft tissue. In case of an open fracture: open fractures have added potential for infection.[23]Also knee ligament injuries are common, such as lateral collateral ligament injuries or anterior cruciate ligament injury and must be assessed after fracture fixation.[24]
Differential Diagnosis[edit | edit source]
Hip pain can be localized to one of three anatomic regions. Pain associated with the anterior hip is mostly an intra-articular pathology (ex. Osteoarthritis and hip labral tears). Posterior hip pain can mostly be associated with piriformis syndrome, sacroiliac joint dysfunction, lumbar radiculopathy and ischiofemoral impingement and vascular claudication. The two last ones are less commonly. Greater trochanteric pain syndrome occurs when lateral hip pain is present. [25][26]
Age can also distinguish the differential diagnosis of hip pain. Older patient are more associated with degenerative osteoarthritis and fractures. Congenital malformations of the femoro-acetabular joint, avulsion fractures, apophyseal or epiphyseal injuries are mostly found in prepubescent or adolescent patient. For adults or skeletally mature patients, hip pain is often related to musculotendinous strain, ligamentous sprain, contusion or bursitis. [27]
When patients are asked about their hip pain several questions should be asker like antecedent trauma or inciting activity, factors that decrease/increase pain, mechanism of the injury and time of onset. [28]
In following table causes of hip pain are presented: [29]
Intra-articulair:
- Labral tears
- Loose bodies
- Femoroacetabular impingement
- Capsular laxity
- Lig. Teres rupture
- Chondral damage
Extra-articulair :
- Iliopsoas tendonitis
- Iliotibial band
- Gluteus medius/minimus
- Greater trochanteric bursitis
- Stress fracture
- Piriformis syndrome
- Sacroiliac joint pathology
Hip mimickers:
- Athletic pubalgia
- Sports hernia
- Osteitis pubis
Livingston et al. also described the differential diagnosis for lateral hip pain [30]
- Acetabular labral tear
- Stress fracture, dislocation, fracture, contusion
- Osteonecrosis, avascular necrosis
- Muscle strain/tear, ligament sprain
- Low back pain, sacroiliac joint dysfunction
- Snapping hip syndrome
- Femoral acetabular impingement
- Bursitis Nerve entrapment syndrome
- Inflammatory disorders such as seronegative arthropathy, rheumatoid arthritis Infection
- Childhood disorders (Legg-Calve-Perthes Disease)
- Metabolic disease Tumor Primary or secondary osteoarthritis
- Psychosocial factors
Diagnostic Procedures[edit | edit source]
On plain radiographs, anteroposterior (AP) and lateral views demonstrate most hip fractures. Check the neck-shaft angle, which is determined by measuring the angle created by lines drawn through the centers of the femoral shaft and femoral neck. This should be approximately 120-130°. If radiographic findings are equivocal but the history and physical examination are concerning for fracture, CT scan should be considered. One drawback to this modality, however, is that findings on scintigraphy are often negative during the first 24 hours after stress fracture. The positive predictive value of radionuclide imaging in diagnosing femoral neck stress pathology approaches 68%.[31]
For patients in whom femoral neck fracture is strongly suspected but standard x-ray findings are negative, an AP view with internal rotation provides a better view of the femoral neck.
If standard radiograph findings are negative and hip fracture still is strongly suspected, MRI and bone scan have high sensitivity in identifying occult injuries; MRI is 100% sensitive in patients with equivocal radiographic findings. For patients in whom a fracture is strongly suspected and radiographs are negative, consider admission if MRI or bone scan is not readily available. [32]
Outcome Measures[edit | edit source]
- Dynamic Gait IndexThe Dynamic Gait Index (DGI) was developed as a clinical tool to assess gait, balance and fall risk. Because the DGI evaluates not only usual steady-state walking, but also walking during more challenging tasks, it may be an especially sensitive test [33] <span style="font-size: 13.28px;" /><span style="font-size: 13.28px;" />
<span style="font-size: 13.28px;" /><span style="font-size: 13.28px;" />International Hip Outcome Tool (iHOT)
- The international Hip Outcome Tool-33 (iHOT-33) is a 33-item self administered outcome measure based on a Visual Analogue Scale response format designed for young and active population with hip pathology [34]
Lower Extremity Functional Scale (LEFS)
- Lower Extremity Functional ScaleThe Lower Extremity Functional Scale (LEFS) is a questionnaire containing 20 questions about a person's ability to perform everyday tasks. The LEFS can be used by clinicians as a measure of patients' initial function, ongoing progress and outcome, as well as to set functional goals. [35]
- A simple, quick and widely used clinical performance-based measure of lower extremity function, mobility and fall risk. We speculated that its properties may be different from other performance-based tests and assessed whether cognitive function may contribute to the differences among these tests in a cohort of healthy older adults. [36]
<span style="font-size: 13.28px;" />
Examination[edit | edit source]
It is important that your doctor know the specifics of how you hurt your leg. For example, if you were in a car accident, it would help your doctor to know how fast you were going, whether you were the driver or a passenger, whether you were wearing your seat belt, and if the airbags went off. This information will help your doctor determine how you were hurt and whether you may be hurt somewhere else. [37]
It is also important for your doctor to know whether you have other health conditions like high blood pressure, diabetes, asthma, or allergies. Your doctor will also ask you about any medications you take.
After discussing your injury and medical history, your doctor will do a careful examination. He or she will assess your overall condition, and then focus on your leg. Yourdoctorwill look for:
- An obvious deformity of the thigh/leg (an unusual angle, twisting, or shortening of the leg)
- Breaks in the skin
- Bruises
- Bony pieces that may be pushing on the skin
After the visual inspection, your doctor will then feel along your thigh, leg, and foot looking for abnormalities and checking the tightness of the skin and muscles around your thigh. He or she will also feel for pulses. If you are awake, your doctor will test for sensation and movement in your leg and foot.
The Ottawa Knee Rules are a clinical tool that can be used to determine the need for radiography following knee injury based on the patient's presentation. Other tests that will provide your doctor with more information about your injury include: [38]
- X-rays. The most common way to evaluate a fracture is with x-rays, which provide clear images of bone. X-rays can show whether a bone is intact or broken. They can also show the type of fracture and where it is located within the femur.
- Computed tomography (CT) scan. If your doctor still needs more information after reviewing your x-rays, he or she may order a CT scan. A CT scan shows a cross-sectional image of your limb. It can provide your doctor with valuable information about the severity of the fracture. For example, sometimes the fracture lines can be very thin and hard to see on an x-ray. A CT scan can help your doctor see the lines more clearly.
Medical Management[edit | edit source]
Intracapsular and extracapsular fractures must be viewed as separate and distinct entities. The treatment of intracapsular fractures, which includes femoral head, subcapital or transcervical femoral neck fractures, must account for compromised blood flow and thus be geared toward its prostatic replacement, maintenance or restoration. [39][40](Koval K.J. et al, Level of Evidence 5, Grigoryan K.V. et al, Level of Evidence 1A) For extracapsular fractures, which includes basicervical and intertrochanteric fractures, treatment focuses on reduction of the displacement and stabilization with implants for early mobilization and weight bearing. [41](Handoll H.H.G. et al, Level of Evidence 2A)
Intracapsular Fractures[edit | edit source]
Complete femoral head fractures
Complete femoral head fractures are mostly located on the posterior side of the hip. Initial treatment consist of reduction, unregarded of the presence or type of femoral fracture. The risk of complication, like avascular necrosis, will decrease within the first few hours of injury when reduction is applied. [42](Sheehan S.E. et al, Level of Evidence 2A)
In the majority of the cases, including dislocations of the femoral head and acetabulum, early closed reduction is favored. Yet, it is contraindicated when a femoral neck fractures is present.[43](Loizou C.L. et al, Level of Evidence 4)
Femoral Head Impaction Fractures
The treatment of femoral head impaction fractures is controversial and challenging in younger patients. It is suggested, for elderly patients, to use a treatment consisting of reconstruction with total hip arthroplasty whereby damaged bone can be replaced. [44](Sheehan S.E. et al, Level of Evidence 2A)
Femoral Neck Fractures
Internal fixation with specific fixation approach depending on the pattern of the fracture is most often used to treat nondisplaced or impacted femoral neck fracturs. Generally, they have good results for young and elderly patients. Early fixation is important to prevent the development of displacement of fractures. Which will happen in 10-30% if not treated. [45](Sheehan S.E. et al, Level of Evidence 2A)
For valgus/varus impacted injuries and Garden 2 fractures, the treatment consists of internal fixation with three cannulated lag screws. This also applies for Pauwels 1 and 2 fractures, but can alternately be fixed with sliding hip screw. Pauwels 3 fractures have a higher risk of instability and are therefore more problematic.[46][47](Koval K.J. et al, Level of Evidence 5, Unnanuntana A. et al, Level of Evidence 4)
Extracapsular Fractures[edit | edit source]
Intertrochanteric Fractures
The treatment for intertrochanteric fractures consist of fixation using a laterale plate and screw fixation or intramedullary nail fixation. There is though no clear consensus regarding which implant is optimal for treating simple fracture patterns. [48](Sheehan S.E. et al, Level of Evidence 2A)
Subtrochanteric Fractures
Displacement of the subtrochanteric includes flexion from iliopsoas muscle, abduction for gluteus medius and minimus muscles and external rotation from piriformis. An intramedullary nail is most used to achieve stability. Also often required is an open approach with direct reduction. [49](Sheehan S.E. et al, Level of Evidence 2A)
Video Animation of Intramedullary Nail Fixation (VIDEO)
Surgical reduction and fixation is indicated for the following types of proximal femur fractures:
- Intracapsular femoral neck fracture
- Dislocated femoral head
- Intertrochanteric fracture
- Subtrochanteric fracture [50]
Splints[edit | edit source]
Alternatively, patients who are not medically stable or nonambulatory may be treated with traction. Applying a traction splint results in the reduction of hemorrhage. This is also one of the primary indications for applying these splints. The most common types of splints are the Thomas and Hare splint. Of which the Hare splint is more preferable because of the small application time. Femoral fractures need to be splinted during the initial phase. Those splints are needed to minimize pain and additional tissue damage.
These splints also have complications resulting from the use of traction splints including iatrogenic peroneal nerve injury, pressure sore development, ligamentous injury and pain. Even though these complications research had advised to apply significant forces because they are necessary to obtain fracture reduction. [51][Daugherty, M. et al, Level of Evidence 2B]
Surgical reduction and fixation should be performed within 24-48 hours of the injury.
Physical Therapy Management[edit | edit source]
Whilst in hospital, a therapist will teach the patient how to use a walking aid to allow them to mobilise, depending on their weight bearing status. The patient should be taught basic range of movement and strengthening exercises to maintain a degree of strength and reduce the risk of blood clots.
Surgical fixation and immobilization are followed by extensive physical therapy. Under extensive therapy can be understood that the patients who underwent a femur fracture should receive a treatment by a physiotherapist who will invest time in gait training. Gait training results in an increased bone formation. Even if gait training is completed using 30-50% of body weight support, an increase in bone formation could be found. [52] After a femoral fracture, most of the muscles are much weaker than before so physiotherapy is very important.
The physiotherapist will begin with range of motion exercises for the hip, knee and ankle because mobility is decreased following immobilization. Mobilization is a very important treatment in the recovery process. The patient can also begin strengthening exercises based on the surgeon's orders (typically six weeks post-op). Patients should also undergo balance and proprioceptive rehab and these abilities are quickly lost with inactivity.
Mobility exercises[edit | edit source]
Knee: flexion and extension, abduction and adduction
Hip: flexion and extension, abduction and adduction, rotation
Functional quadriceps exercises should be initiated as soon as possible after the surgery because the quadriceps help provide stability in the knee. Flexion exercises also need to start as soon as possible, provided the fracture is adequated supported (i.e. the selected fixation approach allows for weight bearing). Physiotherapy should be continued until an acceptable functional range has been achieved or until a static position has been reached. It is necessary to record the range of movements in the knee with accuracy; first this should be done at weekly and then at monthly intervals.
During the postoperative treatment of patients with a proximal femoral fracture, physical therapy should focus on increasing the muscle strength, to improve walking safety and efficiency. Allowing the elderly patient to become more independent.
Research indicates that strengthening the abductor and adductor muscles of the hip increase the laterolateral stability during walks. Resulting in an influence in the improvement of the patient’s dynamic balance.[53]
Orthopaedic therapy:[edit | edit source]
During the immobilisatin period of the therapists need to actively mobilise the foot, with or without weight. Another important aspect is the mobilisation through a hole in the plaster of the patellar bone. The use of isometric exercises are also important to train the muscles (quadriceps, hamstring & glutei) of the upper leg. After the immobilisation period it is necessary to fixate the leg manually or by using a brace. The fixation is needed for the re-education of hip and knee and to secure a progressively verticalisation of the leg and to make the patient independent while walking or during other activities. Also stabilisation exercises with unilateral support are recommended, but also balneotherapy. After the consolidation therapists need to focus on progressively increased pressure, the revalidation of the gait cycle, more intense mobilisation, strength-training therapy to reverse the muscle atrophy that occurred during the immobilisation period and condition training to increase the loss of endurance during the immobilisation period.
Osteosynthesis:[edit | edit source]
Before going to bed, it is advised to massage the pre-articular structures and mobilisation of the hip. All mobilisation techniques can be used except rotations! It is also advised to use passive mobilisation techniques for retrieving the mobility of the patellar bone. The osteosynthesis is positively influenced by using isometric exercises of the hamstrings, quadriceps and glutei and the use of active exercises with low resistance to train the muscles of the hip and knee. The use of massage techniques of the quadriceps is advised straight after the verticalisation without support. The synthesis of the bone is also positively influenced by unilateral stabilisation exercises. After the consolidation period, orthopaedic therapy is recommended.[54]
As non-operative treatment there are 3 alternatives:
1. Skin traction: used in adults only for emergency fracture immobilisation in the field for patient comfort and to facilitate patient transport. Main disadvantage is the causing of slippage or skin necrosis when applying sufficient forces to the limb.
2. Skeletal traction: used for early fracture care before a definitive operative procedure can be performed. The goal is to restore the femoral length and to limit rotational and angular deformities. Skeletal traction may be applied through the distal femur or proximal tibia. Problems with skeletal traction include knee stiffness, limb shortening, prolonged hospitalisation, respiratory and skin aliments, and malunion.
3. Cast Brace: an external support device that permits progressive weight bearing by partially unloading the fracture through circumferential support of the soft tissues. Indications for cast bracing include open fracture, distal third fractures, and comminuted midshaft fractures of the femur. Proximal, simple transverse, or oblique fractures are less amendable to cast bracing due to high stress concentration and a propensity to angulate. The cast brace is best used after an initial period of skeletal traction. Consistently high rates of union, superior to 90%, usually by 13 to 14 weeks, have been reported in numerous studies. Problems with cast bracing include loss of reduction and subsequent malunion, shortening and angulation.[13]
Physical Exercices[edit | edit source]
Improving muscle strength is necessary to enhance postoperative walking capacity for rehabilitation and to diminish the risks of falls. Physical activity will help:
- Preventing other fractures
- Increasing gait speed & balance
- Increasing ADL Performance
- Regaining walking capacity as early as possible after immobiliazion to avoid respiratory complications[55](Mariana BarquetCarneiro et al, Level Of Evidence 1A).
- Better brain function and more social contact
Aerobic fitness is useful to include in a physical therapyplan for an improved cardiorespiratory capacity will lead to a better walking capacity.
Physical exercices are not only crucial for rehabilitation after fracture but for ongoing reinforcing of the mineral bone density, especially in vulnerable populations like elder fragile patients, osteoporotic post-menopausal women or people suffering from osteoporosis or osteopenia. Long-term odd-impact exercice-loading, is associated, similar to high-impact exercice-loading, with a 20% thicker cortex around the femoral neck [56](Nikander R. et al, Level of Evidence 1B). In aerobic fitness, these type of movements are most frequently used.
Moderate magnitude impacts from Odd-exercice loading is mechanically less demanding and makes the body work in all directions, retraining the biomechanical qualities and proporties of the bonestructure and impacting positively the bone mineral density. Fitness aerobics, dance fitness, dance, ball games, gymnastics involving rapid turns and movements are good examples of odd-impact exercices.
Futhermore, duration, frequency and intensity are important and should be customized to the different age-groups .
Strengthening exercices seem to be key for the functional improvement [57](Mariana BarquetCarneiro et al, Level Of Evidence 1A). These strength exercices may as well produce advantages in the psychosocial area which tends to be altered in elder patients that suffered a fracture. Weight-bearing exercices will reinforce the dynamic balance and functional performance [58](SD Yang et al, Level of Evidence 3B), especially exercices in standing position since they are more challenging for the postural control [59](Mariana BarquetCarneiro et al, Level Of Evidence 1A).
Home Rehabilitation Training[edit | edit source]
Home Rehabilitation Training leads towards better rehabilitation and better performance in daily activities. Home physiotherapy training is suitable for all elder patients, including those suffering from cognitive or psychological impairment. The literature stresses the importance of home physiotherapy, in combination with day-to-day activities like going to the shop, for gaining confidence, balance, functionality and reducing as such the number of falls. Therefore it can also be seen as a way to prevent falls. [60](Andrea Giusti et al, Level of Evidence 2B)
Fall prevention programmes are important for the elder population that already sufffered a femoral fracture. The literature indicates that elder people often fall again following a previous hip or femoral fracture and that this constitutes a major health problem [61](M. Berggren et al, Level of Evidence 1B). The study of Berggren et al. concludes that fall-prevention must be part of everyday life in fall-prone elderly. Prevention and treatment of fall-risk factors are key. These programs should include gait training with advice on assistive devices and medication, exerciceprogrammes for balance training, treatments for cardiovascular problems, environmental modifications and hypotension.[62](M. Stenvall et al, Level of Evidence 1B)
Electrical Stimulation[edit | edit source]
The literature is still not conclusive on this topic and the results of one study may contradict or, on the contrary, reinforce the results of another study.Yet there is evidence supporting the beneficial effects of electrical stimuation, especially in combination with physical therapy exercices. In a randomized controlled trial Gremeaux et al.conclude that « Low-frequency electric muscle stimulation can thus be proposed as a simple, effective, and safe complementary therapy used in conjunction with standard rehabilitation in everyday clinical practice in these patients. »
In a critical literature review of 2005 Bax et al. stated that only limited evidence suggests that neuromuscular electrical stimulation can be more effective than no exercice in individuals with impaired and unimpaired quadriceps, and volitional exercises appeared more effective in most situations [63](Braid V et al, Level of Evidence 2B). Low-frequency ES may lead to a significant increase in muscle strength in the operated limb and is overall well tolerated by the elder population.
The terms « Functional electrical Stimulation », « Cyclic Stimulation » or « Neuromuscular Electrical Stimulation » all refer to the same « Electrical Stimulation » but speaking of it, distinction should be made between low-frequency and high-frequency stimulation. High-frequency stimulation acts principally on fast-twitch fibers, increasing muscle strength and resistance to fatigue. It could be useful to fight muscle deconditionning but it is mostly not well tolereated in older patients.
Low-frequency Electrical Stimulation(LFES) increases the metabolic activity of slow-twitch muscle fibers and the proportion of slow-twitch fibers. This fiber-type is more dominantly present in the Quadriceps and therefore interesting to use this low frequency on the knee-extensor muscle. Other structural adaptations are the development of mitochondrial apparatus and increase in capillary density, resulting in increased resistance to fatigue.[64](Vincent Gremeaux et al, Level of Evidence 1B). LFES has also been used in the treatment of different neurologic and orthopedic disorders.
ES may attenuate muscle atrophy, helps regaining muscle strength faster after surgery and show a trend towards improved autonomy and walking speed [65](Vincent Gremeaux et al, Level of Evidence 1B). The results of the study of Gremeaux et al. suggest that low-frequency electric muscle stimulation associated with conventional physiotherapy is superior to physiotherapy alone in increasing strength of the knee extensors, which is accompanied by a return to better muscular equilibrium between the operated and nonoperated limb. It leads to a significant increase in muscle strength in the operated limb. In young subjects ES can produce powerful muscle contraction and give training effects as good as or better than voluntary isometric exercice([66]Braid V et al, Level of Evidence 2B).
Key Search[edit | edit source]
- Carneiro, M. et al.Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. 2013. Levels of evidence: 1A
- Koval, K., & Zuckerman, J. et al. Handbook of Fractures. 2002; second edition. Levels of evidence: 5
- Xhardez Y. et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002. Levels of evidence: 5
- Daugherty, M. et al. Significant Rate of Misuse of the Hare Traction Splint for Children with Femoral Shaft Fractures. Journal of Emergency Nursing. 2013. Levels of evidence: 2B
- AAOS. Stress Fractures of the Foot and Ankle. 2009. Level of evidence: 5
- Texas Orthopedic Spine Institute. Types of bone fractures. Level of evidence: 5
- Cleveland Clinic. Fractures. 2013. Level of Evidence: 5
Resources[edit | edit source]
- http://ac.els-cdn.com/S1878764914706291/1-s2.0-S1878764914706291-main.pdf?_tid=65bdb594-5516-11e4-8d24-00000aab0f01&acdnat=1413451721_842b7d8bdef872019e2b5a7408aca409/
- http://apps.webofknowledge.com.ezproxy.vub.ac.be:2048/full_record.do?product=WOS&search_mode=Refine&qid=4&SID=S2zn1kgocpk8Xkj2bxO&page=1&doc=1
- http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0100-879X2006001000012&lng=en&nrm=iso&tlng=en
- http://orthoinfo.aaos.org/topic.cfm?topic=a00379
- http://www.houstonspineandjoint.com/bone-fracture-types.html
- http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures
- http://www.ncbi.nlm.nih.gov/pubmed/23519955
References[edit | edit source]
- ↑ Michael S Wildstein, MD , Femoral Neck Stress and Insufficiency Fractures: http://emedicine.medscape.com/article/1246691-overview#a4 (Level of evidence 5)
- ↑ AAOS. Stress Fractures of the Foot and Ankle. 2009. (Available at http://orthoinfo.aaos.org/topic.cfm?topic=a00379, accessed 19 December 2014) fckLR(Level of evidence: 5)
- ↑ 2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR(Level of evidence: 5)
- ↑ Cleveland Clinic. Fractures. 2013. (Available at http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-fractures, assessed 21 December 2014)fckLR(Level of Evidence: 5)
- ↑ WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR(Level of Evidence: 5)
- ↑ 2.0 2.1 WebMD. Understanding Bone Fractures - the Basics. 2014. (Available at http://www.webmd.com/a-to-z-guides/understanding-fractures-basic-information, accessed 19 December 2014) fckLR(Level of evidence: 5)
- ↑ Michael S Wildstein, MD , Femoral Neck Stress and Insufficiency Fractures: http://emedicine.medscape.com/article/1246691-overview#a4 (Level of evidence 5)
- ↑ Mercer's Textbook of Orthopaedics and Trauma Tenth edition edited by Suresh Sivananthan, Eugene Sherry, Patrick Warnke, Mark D Miller(Level of evidence:5)
- ↑ WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december 2014)fckLR(Level of Evidence: 5)
- ↑ Andrew R. J. Manktelow, Fares S. Haddad, FRCS (Orth), and Nicholas J. Goddard, FRCS . THE AMERICAN JOURNAL OF SPORTS MEDICINE, Vol. 26, No. 4.(Level of evidence:4 )
- ↑ Keller K. et al. Muscle atrophy caused by limited mobilisation. 2013. (Level of evidence 4)
- ↑ Aukerman DF. Femur injuries and fractures. http://emedicine.medscape.com/article/90779-overview (accessed 30 October 2008) (Level of evidence 5)
- ↑ 13.0 13.1 13.2 Keany, J. et al. Femur fracture. 2013. (Available at http://emedicine.medscape.com/article/824856-overview, accessed 6 November 2014)
- ↑ Consensus Development Conference Prophylaxis and treatment of osteoporosis. American Journal of Medicine. 1991;90:107–110. (Level of evidence 5)
- ↑ Keller K. et al. Muscle atrophy caused by limited mobilisation. 2013. (Level of evidence 4)
- ↑ Consensus Development Conference Prophylaxis and treatment of osteoporosis. American Journal of Medicine. 1991;90:107–110. (Level of evidence 5)
- ↑ Lars Kolmert, KristerWulf. Epidemiology and Treatment of Distal Femoral Fractures in Adults. (Level of evidence 4)
- ↑ 7.0 7.1 Aukerman DF. Femur injuries and fractures. http://emedicine.medscape.com/article/90779-overview (accessed 30 October 2008)
- ↑ Cummings SR. Prevention of hip fractures in older women: a population-based perspective. Osteoporos Int. 1998;8(1):S8–12. (Level of evidence 5)
- ↑ Kanis JA, Oden A, Johnell O, Johansson H, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int.2007;18(8):1033–46. (Level of evidence 5)
- ↑ Internal fixation of femoral neck fractures. An atlas. Manninger, Bosch, Cserháti, Fekete, Kazár. Eds Springer, 2007. (Level of evidence 4)
- ↑ WebMD. Broken bone: types of fractures, symptoms and prevention. 2014. (Available at http://www.webmd.boots.com/a-to-z-guides/bone-fractures-types-symptoms-prevention, accessed on 21 december2014)fckLR (Level of Evidence: 5)
- ↑ AAOS. Stress Fractures of the Foot and Ankle. 2009. (Available at http://orthoinfo.aaos.org/topic.cfm?topic=a00379, accessed 19 December 2014) fckLR(Level of evidence: 5)
- ↑ 10.0 10.1 Koval, K., & Zuckerman, J. et al. Handbook of Fractures. 2002; second edition. Levels of Evidence : 5
- ↑ WILSON J.J. et al, Evaluation of the Patient with Hip Pain, American Academy of Family Physicians, January 2014, Volume 89, Number 1 (Level of evidence: 5)
- ↑ DeAngelis N.A. et al, Assessment and differential diagnosis of the painful hip, Clinical Orthopaedics& Related Research, January 2003, Volume 406, p. 11-18 (Level of evidence : 4)
- ↑ WILSON J.J. et al, Evaluation of the Patient with Hip Pain, American Academy of Family Physicians, January 2014, Volume 89, Number 1 (Level of evidence: 5)
- ↑ WILSON J.J. et al, Evaluation of the Patient with Hip Pain, American Academy of Family Physicians, January 2014, Volume 89, Number 1 (Level of evidence: 5)
- ↑ Libor L.M. et al, Differential Diagnosis of Pain Around the Hip Joint, Arthroscopy: The Journal of Arthroscopic & Related Surgery, December 2008, Volume 24, Issue 12, Pages 1407–1421 (Level of evidence: 5)
- ↑ Livingston J.I., Differential Diagnostic Process and Clincal Decision Making in a Young Adult Female With Lateral Hip Pain: A Case Report, The International Journal of Sports Physical Therapy, October 2015, Volume 10, Number 5 (Level of evidence : 4)
- ↑ Moira Davenport: Hip Fracture in Emergency Medicine, http://emedicine.medscape.com/article/825363-overview(Level of evidence : 4)
- ↑ Michael S Wildstein, MD , Femoral Neck Stress and Insufficiency Fractures: http://emedicine.medscape.com/article/1246691-overview#a4 (Level of evidence 5)
- ↑ Herman T, Inbar-Borovsky N, Brozgol M, Giladi N, Hausdorff JM. The Dynamic Gait Index in Healthy Older Adults: The Role of Stair Climbing, Fear of Falling and Gender. Gait& posture. 2009;29(2):237-241
- ↑ Ruiz-Ibán MA, Seijas R, Sallent A, et al. The international Hip Outcome Tool-33 (iHOT-33): multicenter validation and translation to Spanish. Health and Quality of Life Outcomes. 2015;13:62 (Level of evidence : 5)
- ↑ Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999 Apr;79(4):371-83.(Level of evidence : 5)
- ↑ Herman T, Giladi N, Hausdorff JM. Properties of the “Timed Up and Go” Test: More than Meets the Eye. Gerontology. 2011;57(3):203-210. (Level of evidence : 5)
- ↑ Brett Crist, MD; Stuart J. Fischer, MD; Stephen Kottmeier, MD.Femur Shaft Fractures (Broken Thighbone) (Level of evidence 4)
- ↑ Evans P.J., McGrory B.J. Fractures of the proximal femur. Hosp Physician. 2002:30–38. (Level of evidence 4)
- ↑ Koval K.J. et al, Handbook of Fractures, Lippincott Williams & Wilkins, second edition, 2002, p. 180-181; 186-187; ev. (Level of evidence : 5
- ↑ Grigoryan K.V .et al, Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma, 2014;28(3): e49–e55. (Level of evidence : 1A)
- ↑ Handoll H.H.G. et al, Osteotomy, compression and other modifications of surgical techniques for internal fixation of extracapsular hip fractures (Review), Cochrane Library, 2009 (Level of evidence: 2A)
- ↑ Sheehan S.E. et al, Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know, RadioGraphics, 2015, Volume 35-Number 5 (Level of evidence: 2A)
- ↑ Loizou C.L. et al, Classification of subtrochanteric femoral fractures. Injury, 2010;41(7):739–745. (Level of evidence : 5)
- ↑ Sheehan S.E. et al, Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know, RadioGraphics, 2015, Volume 35-Number 5 (Level of evidence: 2A)
- ↑ Sheehan S.E. et al, Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know, RadioGraphics, 2015, Volume 35-Number 5 (Level of evidence: 2A)
- ↑ Koval K.J. et al, Handbook of Fractures, Lippincott Williams & Wilkins, second edition, 2002, p. 180-181; 186-187; ev. (Level of evidence : 5)
- ↑ Unnanuntana A. et al, Atypical femoral fractures: what do we know about them?, AAOS Exhibit Selection. J Bone Joint Surg Am 2013, 95(2):e8 1–13. 71. (Level of evidence : 5)
- ↑ Sheehan S.E. et al, Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know, RadioGraphics, 2015, Volume 35-Number 5 (Level of evidence: 2A)
- ↑ Sheehan S.E. et al, Proximal Femoral Fractures: What the Orthopedic Surgeon Wants to Know, RadioGraphics, 2015, Volume 35-Number 5 (Level of evidence: 2A)
- ↑ Kisner C, Colby LA. Therapeutic exercises: foundations and techniques. Philadelphia: F.A. Davis, 2012.
- ↑ Daugherty, M. et al. Significant Rate of Misuse of the Hare Traction Splint for Children with Femoral Shaft Fractures. Journal of Emergency Nursing. 2013.fckLR(Levels of Evidence : 2B)
- ↑ Carvalho, D.C.L et al. Effect of treadmill gait on bone markers and bone mineral density of quadriplegic subjectshttp. 2006.
- ↑ Carneiro, M. et al. Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. 2013. fckLR(Levels of evidence: 1A)
- ↑ Xhardez Y et al. Vade-mecum kinésithérapie et de reeducation fonctionnelle. 2002. fckLR(Levels of evidence: 5)
- ↑ Mariana Barquet Carneiro, Débora Pinheiro Lédio Alves, and Marcelo Tomanik Mercadante. Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. ActaOrtopédicaBrasileira 2013 May-June; 21(3): 175–178. (Level of evidence 1A)
- ↑ Nikander R, Kannus P, Dastidar P, Hannula M, Harrison L, Cervinka T, Narra NG, Aktour R, Arola T, Eskola H, Soimakallio S, Heinonen A, Hyttinen J, Sievänen H. Targeted exercises against hip fragility. Osteoporos Int. 2009 Aug;20(8):1321-8. (Level of evidence 1B)
- ↑ Mariana Barquet Carneiro, Débora Pinheiro Lédio Alves, and Marcelo Tomanik Mercadante. Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. ActaOrtopédicaBrasileira 2013 May-June; 21(3): 175–178. (Level of evidence 1A)
- ↑ SD Yang, SH Ning, LH Zhang, YZ Zhang, WY Ding. The effect of lower limb rehabilitation gymnastics on postoperative rehabilitation in elderly patients with femoral shaft fracture: A retrospective case-control study. Medicine, 2016 - journals.lww.com (Level of evidence 3B)
- ↑ Mariana Barquet Carneiro, Débora Pinheiro Lédio Alves, and Marcelo Tomanik Mercadante. Physical therapy in the postoperative of proximal femur fracture in elderly. Literature review. ActaOrtopédicaBrasileira 2013 May-June; 21(3): 175–178. (Level of evidence 1A)
- ↑ Andrea Giusti, MD, Antonella Barone, MD, Mauro Oliveri, MD, Monica Pizzonia, MD, Monica Razzano, MD, Ernesto Palummeri, MD, Giulio Pioli, MD, PhD. An Analysis of the Feasibility of Home Rehabilitation Among Elderly People With Proximal Femoral Fractures. Archives of Physical Medicine and Rehabilitation. June 2006, Volume 87, Issue 6, Pages 826-831. (Level of evidence 2B)
- ↑ M. Berggren, M. Stenvall, B. Olofsson, Y. Gustafson.Osteoporosis International . Evaluation of a fall-prevention program in older people after femoral neck fracture: a one-year follow-up. June2008, Volume 19, Issue 6, pp 801-809. (Level of evidence 1B)
- ↑ M. Stenvall, B. Olofsson, M. Lundström, U. Englund, B. Borssén, O. Svensson, L. Nyberg, and Y. Gustafson. A multidisciplinary, multifactorial intervention program reduces postoperative falls and injuries after femoral neck fracture. Osteoporosis International. Feb 2007; 18(2): 167–175.(Level of evidence 1B)
- ↑ Braid V, Barber M, Mitchell SL, Martin BJ, Granat M, Stott DJ. Randomised controlled trial of electrical stimulation of the quadriceps after proximal femoral fracture AgingClinExp Res. 2008 Feb;20(1):62-6. (Level of evidence: 1B)
- ↑ Vincent Gremeaux, MD, Julien Renault, MS, Laurent Pardon, MS, GaelleDeley, PhD, Romuald Lepers, PhD, Jean-Marie Casillas, MD. Low-Frequency Electric Muscle Stimulation Combined With Physical Therapy After Total Hip Arthroplasty for Hip Osteoarthritis in Elderly Patients: A Randomized Controlled Trial Archives of Physical Medicine and Rehabiliation. December 2008, Volume 89, Issue 12, Pages 2265-2273. (Level of evidence: 1B)
- ↑ Vincent Gremeaux, MD, Julien Renault, MS, Laurent Pardon, MS, GaelleDeley, PhD, Romuald Lepers, PhD, Jean-Marie Casillas, MD. Low-Frequency Electric Muscle Stimulation Combined With Physical Therapy After Total Hip Arthroplasty for Hip Osteoarthritis in Elderly Patients: A Randomized Controlled Trial Archives of Physical Medicine and Rehabiliation. December 2008, Volume 89, Issue 12, Pages 2265-2273. (Level of evidence: 1B)
- ↑ Braid V, Barber M, Mitchell SL, Martin BJ, Granat M, Stott DJ. Randomised controlled trial of electrical stimulation of the quadriceps after proximal femoral fracture AgingClinExp Res. 2008 Feb;20(1):62-6. (Level of evidence: 1B)