Female Genital Tract
Original Editor - Khloud Shreif
Top Contributors - Khloud Shreif, Kim Jackson, Anthonia Abraham and Anna Fuhrmann
Introduction[edit | edit source]
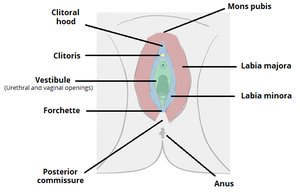
The female genital tract consists of the external genitalia or vulva that consists of ( mons pubis, labia majora, labia minora, clitoris, vestibule, hymen, bartholin's glands, external urethra meatus, and skene's gland). The internal genital tract or reproductive system and consists of ( the vagina, uterus, fallopian tubes, and ovaries).
External Genitalia/ Vulva[edit | edit source]
Function of external genitalia: protect the internal genital tract from infection, act as a sensory tissues during sexual intercourse, assist in micturition.
Innervation of Vulva, it receives parasympathetic and sensory supply if it is divided into anterior and posterior parts:
The anterior part. it is supplied by ilioinguinal nerve L1, the genital branch of the genitofemoral nerve L1,2.
The posterior part, pudendal nerve (S2,3,4), posterior cutaneous nerve of the thigh.
Clitoris and vestibule, parasympathetic innervation from the cavernous nerves a branch from the uterovaginal plexus[1].
Mons Pubis/ Veneris[edit | edit source]
It is a bad of fat located anterior and cover the symphysis pubis underlying the skin, it is covered with hair at puberty.
Labia Majora[edit | edit source]
Two skin fleshy folds, extend posteriorly to mons pubis, the outer skin is covered by hair, the inner surface is smooth, hairless and contain sweat and sebaceous glands that produce lubricant secretion.
Labia Minora[edit | edit source]
Two hairless skin folds lies within and medial to the labia majora.it is about 2 inches wide and surrounds the openings to the vagina and urethra. They meet posteriorly forming skin folds called fourchette. Fourchette separated from hymen by depression named fossa navicularis.
It is rich in blood supply that gives it the bink color, during sexual stimulation it swells and becomes more sensitive to stimulation.
Clitoris[edit | edit source]
It is located between the upper end of the labia minora, formed of erectile corpora cavernosa tissue, and homologous to the penis in the male.
It is sensitive to sexual stimulation can become erect.
Vestibule[edit | edit source]
It is the area between the labia minora where the vagina and urethra open.
Hymen[edit | edit source]
It is a thin membrane of soft tissue covered by stratified squamous epithelium, lies deep to the vestibular orifice. and cover the vaginal orifice. Hymen has many shapes to allow menstrual blood to flow out of the vagina. It is usually torn during the first intercourse.
Bartholin's Glands/ Greater Vestibular Glands[edit | edit source]
Bilateral racemes glands located at the sides of the vaginal orifice. Secret mucous that acts as a lubricant.
External Urethral Meatus[edit | edit source]
It opens in the vestibule behind the clitoris.
Skene's Gland[edit | edit source]
It is a paraurethral glands open adjacent to distal urethra.
Skene's duct may be obstructed because the gland is infected causing skene's duct cyst. If the duct is infected it causes recurrent urinary tract infection and if the cyst is larger than 1 cm it cause dyspareunia[3]
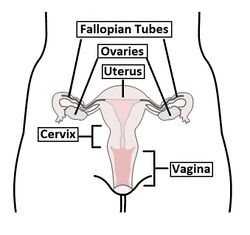
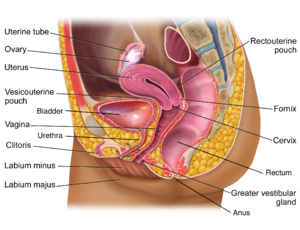
Internal Reproductive System[edit | edit source]
Vagina[edit | edit source]
A fibromuscular tube extends from vulva to the uterus in an oblique direction forming angle about 60° with the horizontal line, directed upward and backward. ranging from 6-8 cm in length and due to its obliquity, its posterior wall is larger than the anterior wall. It is more like the H shape than a round tunnel.
Located anterior to the rectum and posterior to the urethra and bladder.
Between the connection of the upper end of the vagina and cervix, it forms two fornix, anterior fornix, and the posterior fornix which is deeper than the anterior and acts as a reservoir for the semen it can keep it for about 20-30 min allowing for better penetration through the cervical canal.
Function of the Vagina[edit | edit source]
It is a canal for menstrual tissue and fluid during the menstruation.
Expands during the childbirth for the delivery of new fetus.
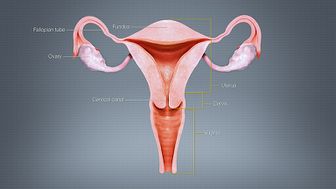
Uterus[edit | edit source]
It is a pear hollow central landmark organ of the pelvic anatomy and internal genitalia, its lower end at the level of the ischial spine, and supported by pelvic floor muscles and cervical ligaments. It is highly muscular, relatively larger in multipara females, and relatively mobile, its cavity lining with endometrium.
During pregnancy, it reaches the epigastric area due to the fetus growth, divided into:
The cervix: the most lower part of the uterus connect it to the vagina through the external OS, and connect to the uterus via the internal OS, 2.5-3 cm in length.
The isthmus: the area of connection between the uterine body and the cervix 4-5mm in length.
The body: the largest part of the uterus about 5 cm length.
The fundus: the area above the insertion of the fallopian tubes, the corny, the area where the insertion of fallopian tubes arise.
The uterus is located anatomically in anteversion anteflexion position anterior to the rectum and posterior and superior to the bladder.
Anteversion, the angle between the axis of the cervix and the axis of the vagina making 90 angle, rotated forward. Anteflexion, the angle between the body of the uterus and the axis of the cervix, the body is bent forward.
Fallopian tubes[edit | edit source]
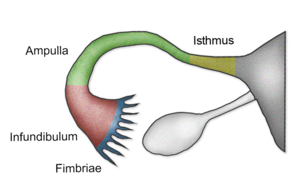
A muscular J shape tubes presented on both sides of the uterus extend to open into the abdominal cavity it is 10 cm in length. Its main function to transmit the ovum to the uterus and the site for fertilization, divided into:
Fimbriae: fingers like projections, it brings the ovum from the ovary.
Infundibulum: it is a funnel shape, the fimbriae attaches to it.
Ampulla: the widest section of the tube, where fertilization happens.
Isthmus: the narrowest part of the fallopian tube presents with the uterine wall.
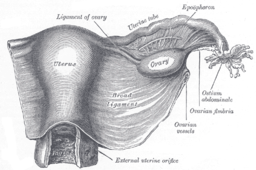
Ovaries[edit | edit source]
Two almond-shaped organs, its main function is the production of ova and sex hormones, they attach to the uterus by ovarian ligaments, and to the broad ligament via a mesovarium, it is a peritoneal ligament[4].
Clinical Relevance[edit | edit source]
Bartholinitis, the Bartholin's Glands can be infected or inflamed that can be treated by an antibiotic if it is obstructed it can cause vulva swelling forming a cyst or abscess, in this case, surgical intervention will be the effective treatment.
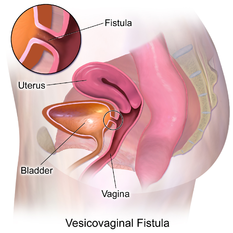
Vaginal Fistulae, an abnormal connection between the vagina and adjacent pelvic organs that can happen as a result of prolonged labor, the fetus exerts pressure during delivery causing obstruction of the blood supply and necrosis. Treated surgically, types:
- Vesicovaginal fistulae, an abnormal fibrous connection between the vagina and bladder in which there is a continuous leakage of urine causing UI, it happens as a post-operative pelvic surgery complication[5].
- Urethrovaginal fistulae, abnormal communication between the vagina and urethra in this situation urine enters the vagina during urination only.
- Rectovaginal fistula, an abnormal epithelialized connection between the vagina and rectum. Obstetrical trauma is the most common cause of along with neoplasm, trauma from previous surgeries, infection.[6]
Endometriosis. chronic inflammation of the lining layer of the cavity of the uterus.
Salpingitis, acute or chronic inflammation of the fallopian tube caused by bacterial infection causing adhesion formation that causing infertility or ectopic pregnancy[7] and one of the causes of pelvic inflammatory disease. It is diagnosed by using diagnostic ultrasound abdominal or vaginal.
Polycystic ovarian cyst syndrome. a disorder affecting the women's hormones.
Suggested reading:[edit | edit source]
Polycystic ovarian cyst syndrome.
Resources[edit | edit source]
References[edit | edit source]
- ↑ Nguyen J, Duong H. Anatomy, Abdomen and Pelvis, Female External Genitalia. InStatPearls [Internet] 2019 Oct 10. StatPearls Publishing.
- ↑ AnatomyZone. Introduction to Female Reproductive Anatomy Part 4 - External Genitalia - 3D Anatomy Tutorial . Available from: http://www.youtube.com/watch?v=0NFZUrDNadc[last accessed 12/6/2020]
- ↑ https://www.msdmanuals.com/professional/gynecology-and-obstetrics/miscellaneous-gynecologic-disorders/skene-duct-cyst
- ↑ Hoare BS, Khan YS. Anatomy, Abdomen and Pelvis, Female Internal Genitals. InStatPearls [Internet] 2020 Feb 27. StatPearls Publishing.
- ↑ El-Azab AS, Abolella HA, Farouk M. Update on vesicovaginal fistula: A systematic review. Arab journal of urology. 2019 Jan 2;17(1):61-8.
- ↑ Das B, Snyder M. Rectovaginal fistulae. Clinics in colon and rectal surgery. 2016 Mar;29(01):050-6.
- ↑ Briceag I, Costache A, Purcarea VL, Cergan R, Dumitru M, Briceag I, Sajin M, Ispas AT. Fallopian tubes–literature review of anatomy and etiology in female infertility. Journal of medicine and life. 2015 Apr;8(2):129.