Female Athlete Triad
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (9/04/2019)
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - James Chad Cissell, Michelle Walsh, Ethan Adams, Aarti Sareen, Lucinda hampton, Wanda van Niekerk, Regan Haley, Kim Jackson, Nicole Hills, Elaine Lonnemann, 127.0.0.1, Oyemi Sillo, WikiSysop, Adam Vallely Farrell, Rishika Babburu and Claire Knott
Definition/Description[edit | edit source]
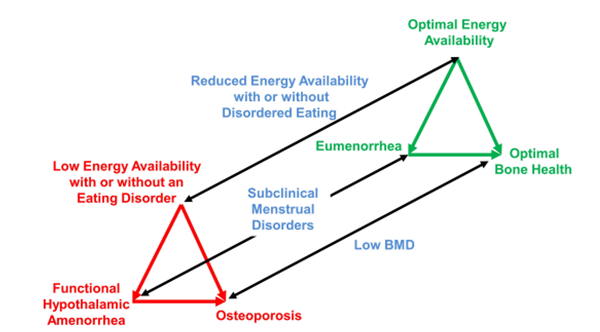
The Triad is a medical condition often observed in physically active girls and women, and involves any of the three components.[1] Female Athlete Triad is a syndrome that evolves from the interrelationship between low energy availability with or without disordered eating, low bone mineral density, and menstrualdysfunction. The clinical manifestations include eating disorders, improper nutrition, functional hypothalamic amenorrhea, and osteoporosis. Not all clinical signs must be present to diagnose Female Athlete Triad.[2] Female Athlete Triad commonly occurs in adolescent or highly competitive female athletes. This syndrome is most common in adolescent athletes, largely due to their skeletal immaturity and naturally low Bone Mineral Density (BMD) being more susceptible to physical and metabolic stressors. Along with health care providers, all coaching staff members of high level and high school women’s sports teams should be highly aware of signs of this disease in order to manage the health of their players.[3] It is also recommended that all female athletes are screened for Female Athlete Triad on a yearly basis.[4] Early signs of the Female Athlete Triad include weight changes, repeated fractures, and decreased energy. Longterm effects of Female Athlete Triad include low peak BMD, Osteoporosis, Thoughts of suicide during long term disease process, and kidney and liver dysfunction.[4]
Below is a Female Athlete Triad Coalition diagram for the clinical spectrum of Female Athlete Triad. The red triangle represents pathological changes, the green represents clinical findings needed before return to play is recommended.
The International Olympic Committee (IOC) has developed a broader syndrome called Relative Energy Deficiency in Sport (RED-S). It has been described by the IOC as an umbrella term for energy disorders in athletes. RED-S is still a relatively new attempt to create a general guideline to the identification and treatment of athletes across genders and pathologies. There is still only shallow research supporting this evolving term, but as of now the IOC considers Female Athlete Triad part of their over all RED-S diagnosis.[6][7]
For the purposes of this page, the ACSM definition of Female Athlete Triad will be discussed. The IOC does not yet have much evidence to support it's use for predicting and understanding pathology.
Prevalence[edit | edit source]
Due to inconsistencies and limitations in criteria defining Female Athlete Triad, study methodology, and experimental design there is an evident discrepancy in the literature when determining the prevalence of the triad.[1] Commonly patients present with only one of the conditions of female athlete triad. These patients range from 16% to 60% of female athlete triad patients. Patients clinically presenting with two conditions at the same time range from 3% to 27% of patients. Clinical manifestation of all three conditions of female athlete triad simultaneously is reported to occur from 0% to 16% of patients. This is rarely seen outside of severe cases.[8] Development of Female Athlete Triad is possible for sedentary and normally active females. This occurs at rates that are only slightly less than competitive female athletes.[9][10]
Characteristics/Clinical Presentation[edit | edit source]
- Weight loss
- Absent or irregular periods
- Fatigue
- Stress fractures
- Restrictive dieting
- Binge eating
- Induced vomiting
- Excessive exercise
Screening and Risk factor stratification[edit | edit source]
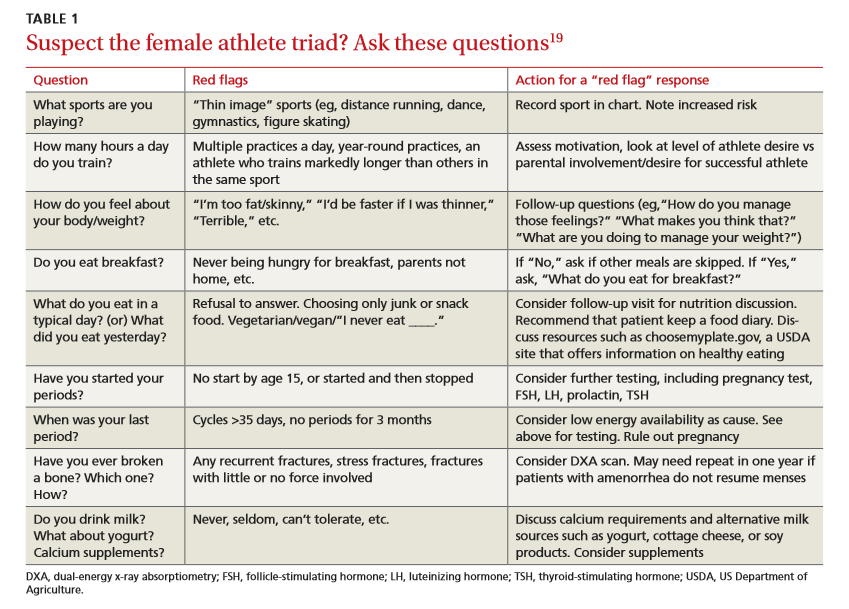
Early detection of athletes who are at risk is critical to prevent the Triad. Screening for the Triad should be undertaken as part of the Pre-Participation Physical Evaluation (PPE).[1] The PPE should include questions that address all aspects of the Triad spectrums. There is a standardised screening tool that has been endorsed by several medical societies and includes nine questions related to the Triad.
A consensus statement on the Female athlete triad developed a screening questionnaire that should be asked at the time of pre-sport participation. These questions are;
- Have you ever had a menstrual period?
- How old were you when you had your first menstrual period?
- When was your most recent menstrual period?
- How many periods have you had in the past 12 months?
- Are you presently taking any female hormones (oestrogen, progesterone, birth control pills)?
- Do you worry about your weight?
- Are you trying to or has anyone recommended that you gain or lose weight?
- Are you on a special diet or do you avoid certain types of foods or food groups?
- Have you ever had an eating disorder?
- Have you ever had a stress fracture?
- Have you ever been told you have low bone density (Osteopenia or Osteoporosis)?[1]
The most important risk factors that should be assessed for the triad include; history of menstrual irregularities and amenorrhoea, history of stress fractures, history of critical comments about eating or weight from parent, coach or teammate, a history of depression, a history of dieting, personality factors (such as perfectionism and obsessiveness), pressure to lose weight and/or frequent weight cycling, early start of sport-specific training, overtraining, recurrent and non-healing injuries and inappropriate coaching behaviour.[1]
Associated Co-morbidities[edit | edit source]
Due to the loss in bone mineral density the primary co-morbidity associated with female athlete triad is osteoporosis. Female athlete triad generally occurs in the primary age range for storing and depositing calcium in the bones (12-19 years old).[8] Slowing or reversing bone development at this age results in the potential to increase the risk of fractures later in life, even after resolving the issues leading to a diagnosis of female athlete triad.
Systemically low Bone Mineral Density, low blood estrogen level, and menstrual dysfunction has been linked to Endothelial Dysfunction in endurance athletes. Endothelial Dysfunction is directly related to the bodies ability to constrict or dilate blood vessels. If Endothelial Dysfunction is present (indicated by Brachial Artery flow-mediated dilation) the risk for cardiovascular events, poor blood flow mediation, and atherosclerotic disease are all increased significantly.[6]
Medications[edit | edit source]
Antidepressants are often used to treat associated concomitant depression and anxiety disorders. They are also used following weight restoration for bulimia nervosa and anorexia nervosa. Research has show mixed results for improving BMD or restoring menstrual cycles when using hormone replacement therapy (HRT) or oral contraceptive pill (OCP). While BMD may not be improved by using OCP, it may help to reduce further loss in BMD in athletes under the age of 16. Young women with functional hypothalamic amenorrhea should not use biphosphonates that are approved for the treatment of postmenopausal osteoporosis due to their unproven efficacy in women of childbearing age. Also since the medication tend to linger in the bones for many years they have the potential to cause harm to a developing fetus is the patient becomes pregnant later in life. Ovulation inducing agents such as clomiphene citrate and exogenous gonadotropins are indicated if the aim of therapy is to restore fertility.[2] Nutritional therapy has the best evidence for successfully treating female athlete triad due to its ability to in increase energy availability.[7]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
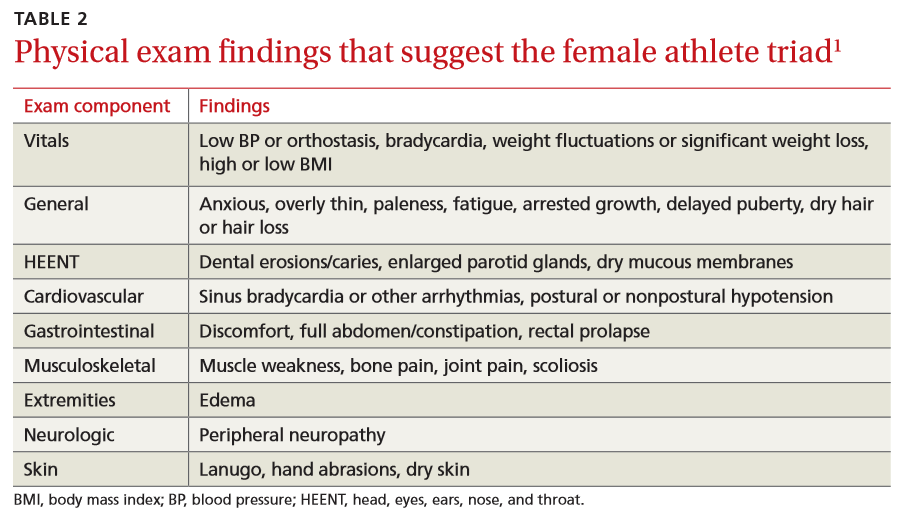
Athletes most commonly show signs of 1 or 2 components of Female Athlete Triad. If suspected due to pain, recurrent fractures, recurrent sprains, Low BMI (<85% expected weight), poor eating habits, or other, use the following questions to see if there is cause for concern.
Non-Modifiable:
- Female Gender
- Age 12-19
Modifiable:
- Early age sport specialization
- Low BMI (Z-score less than or equal to -1)
- Over-training
- Engaging in sports with endurance, aesthetic, and weight class components
- Severe Dieting
- Family Dysfunction
- Abuse
Energy Availability (EA)
- Energy Intake should be at least 45 kcal/kg of fat-free mass (FFM)[6]
- < 30kcal/kg FFM disrupts bone mineralization and menstruation[6]
- 5 days or more of < 30kcal/kg decreases luteinizing hormone availability in the body[6]
Triggers for disordered eating may include: Prolonged dieting, weight fluctuations, changes in coaching, injury, and social attention to weight.
Bone Mineral Density
In women, about 90% of bone formation should be complete by 18 years old[4], with bone density peaking between 20-30 years old. Poor Bone Mineral density is correlated with being <85% expected weight for height and age. A Z-score at or below -1.0 significantly increased risk for fractures and osteoporotic changes.
Long Distance Running is a highest risk sport for negatively impacting BMD
Use BMD Screenings to rule out other diagnoses such as celiacs disease[11]
Menstruation
Disorders in menstrual function can be as mild as anovulation and luteal dysfunction to Oligomenorrhea and Amenorrhea
Menstrual disturbances are common in all adolescents (~21%), but more common in adolescent athletes (~54%)[6]
- Anovulation - ovaries do not release an oocyte and ovulation doesn’t occur. (few overt symptoms)
- Luteal Deficiency - low concentration of blood progesterone and or Luteal phase lasting less than 11 days (few overt symptoms)
- Oligomenorrhea - menstrual cycles lasting longer than 35 days
- Primary Amenorrhea is the “absence of menarche by the age of 15 years.”[6]
- Secondary Amenorrhea is absence of menstruation for greater than or equal to 3 consecutive months after menarche
Etiology/Causes[edit | edit source]
Female Athlete Triad may be caused by one or more of several factors in each individual patient.[4][6][7][3][4]
Low Energy Availability is thought to be the primary cause of Female Athlete Triad.
- Energy Availability is the dietary energy left in the body after exercise is completed, or total dietary energy in (calories in) minus total exercise energy expended (calories out).[5][8] Low energy availability is not synonymous with disordered eating.[11]
- Causes - Restricted Diet, Disordered Eating, Genetic absorption problem.
Over-training is also a common factor in Female Athlete Triad.
- Over-training can be the trigger for the pathology as working your body past a reasonable training schedule prevents it from being able to heal from previous training sessions. This increases metabolic demands and releases stress-related hormones that affect blood flow and is severe cases absorption of nutrients. Over-training may prevent appropriate musculoskeletal recovery, perpetuate high levels of blood cortisol, and negatively affect energy absorption. These factors over time can cause cortical thinning of bones, pathological weakening of muscles and ligaments, and disrupt normal metabolic cycles. Over time the excess stress hormone and physical demand degrade the bone density of the athlete.[5]
- Over-training is engaging in repetitive stressful activity (>7 Met) for more than 60 min 6 days/week.
Systemic Involvement[edit | edit source]
- GI - low intake, atrophy, abnormal acid balance, and nutrient deficits
- Cutaneous - without appropriate nutrients, the skin becomes brittle and takes longer to heal
- Integumentary - lax weak ligaments from poor recovery time and nutrition.
- Musculoskeletal - inability to grow new muscle due to lack of resources and poor recovery time. Strength and endurance depletion from systemic catabolism.
- Cardiopulmonary and Circulatory - poor blood sugar, poor serum cholesterol and triglycerides, fragile balance of metabolites with decreased ability to compensate for imbalances due to poor storages. Reduced clotting factor. Increased incidence of endothelial dysfunction.
- Endocrine - increased production of stress hormones, decreased ability to balance homeostatic control due to poor systemic condition from prolonged stress and absent nutrients.
- Lymphatic and Immune - Immune system becomes fragile due to systemic stress.
- Neurological - decreased attention span. possibly poor balance.
- Reproductive System - Reproductive system shuts down (reduced blood flow, reduced metabolism, reduced hormone production) to maintain energy for vital functions.
Medical Management[edit | edit source]
An interdisciplinary team is necessary to manage female athlete triad.
- Nutritionist - Energy imbalance is the corner-stone of Female Athlete Triad, the first treatment is to have a full nutritional assessment. Vitamins, Minerals, and Nutrition
- Psychologist - there is often a psychological factor that drives disordered eating or over training. Athletes affected with eating disorders have a long-term increased risk of suicide.[4]
- Primary Care Provider - Important for pharmaceutical management and regular physical check ups.
Energy Balance
- Acute stages: restore or create sufficient nutrition balance for caloric needs.
- Subacute/Chronic stages: If long term, get back to healthy weight then treat as acute
Training Balance
- Acute stages: Make sure training is in appropriate proportion
- Chronic stages: training may need to be modified to low impact exercise if the patient has suffered extensive disease process.
Bones Mineral Density
Focus medical treatment on fractures first, restore nutrition to appropriate level, decrease training to appropriate levels.
If Z score is less than or equal to -1.0 no high impact activity is allowed and the patient must increase Ca Vit D intake. A lab study to rule out underlying hormonal issues is recommended. Z-score may not reach 1. Return to moderate volumes of high impact activity may take place once Z-score exceeds -1.[5]
Lower bone density may persist in life after triad - may improve with resistance training and augmented Ca Vit D consumption.[6]
Physical Therapy Management[edit | edit source]
Once a physical therapist notices the signs and symptoms of Female Athlete Triad, it is important that they get other health care professionals involved in the treatment of the patient. Physical Therapists are educated to be experts of movement and the physiological response to exercise, it is imperative that they are involved in patient education and exercise prescription once the patient’s nutritional/energy needs are resolved. Physical Therapists may also help develop criteria for returning to sport.[9][10]
Differential Diagnosis[edit | edit source]
- Primary Amenorrhea
- Secondary Amenorrhea due to other factors listed above[6]
- Brittle Bone Disease
- Secondary causes of low BMD (such as B12 Deficiency)
- Thyroid Disorders[11]
- Parathyroid Disorders
- Celiacs Disease[6]
- Osteoporosis - inadequate accumulation of optimal BMD during childhood and adolescence[11]
- Ewing's Sarcoma
Resources[edit | edit source]
Female Athlete Triad Coalition - http://www.femaleathletetriad.org/
APTA - http://www.moveforwardpt.com/symptomsconditionsdetail.aspx?cid=0ca4bf2e-6d14-4b90-b1ec-ed8ebe13069e
NCAA - http://www.ncaa.org/health-and-safety/sport-science-institute/female-athlete-body-project
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 De Souza, Mary Jane, et al. "2014 Female Athlete Triad Coalition Consensus Statement on treatment and return to play of the female athlete triad: 1st International Conference held in San Francisco, California, May 2012 and 2nd International Conference held in Indianapolis, Indiana, May 2013." Br J Sports Med 48.4 (2014): 289-289.
- ↑ 2.0 2.1 2.2 2.3 The Female Athlete Triad. Medicine & Science In Sports & Exercise [serial on the Internet]. (2007, Oct), [cited March 27, 2017]; 39(10): 1867-1882. Available from: Academic Search Complete.
- ↑ 3.0 3.1 Mukherjee S, Chand V, Wong X, Choong P, Lau V, Ng K, et al. Perceptions, awareness and knowledge of the Female Athlete Triad amongst coaches—Are we meeting the expectations for athlete safety?. International Journal Of Sports Science & Coaching [serial on the Internet]. (2016, Aug), [cited March 27, 2017]; 11(4): 545-551. Available from: PsycINFO.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Thein-Nissenbaum J. Long term consequences of the female athlete triad. Maturitas [serial on the Internet]. (2013, June), [cited March 27, 2017]; 75(2): 107-112. Available from: MEDLINE.
- ↑ 5.0 5.1 5.2 5.3 Stickler L, Hoogenboom B, Smith L. THE FEMALE ATHLETE TRIAD-WHAT EVERY PHYSICAL THERAPIST SHOULD KNOW. International Journal Of Sports Physical Therapy [serial on the Internet]. (2015, Aug), [cited March 27, 2017]; 10(4): 563-571. Available from: MEDLINE.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 De Souza M, Williams N, Nattiv A, Joy E, Misra M, McComb J, et al. Misunderstanding the female athlete triad: refuting the IOC consensus statement on Relative Energy Deficiency in Sport (RED-S). British Journal Of Sports Medicine [serial on the Internet]. (2014, Oct), [cited March 27, 2017]; 48(20): 1461-1465. Available from: MEDLINE.
- ↑ 7.0 7.1 7.2 Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Ljungqvist A, et al. The IOC consensus statement: beyond the Female Athlete Triad--Relative Energy Deficiency in Sport (RED-S). British Journal Of Sports Medicine [serial on the Internet]. (2014, Apr), [cited April 2, 2017]; 48(7): 491-497. Available from: MEDLINE.
- ↑ 8.0 8.1 8.2 Gibbs J, Williams N, De Souza M. Prevalence of individual and combined components of the female athlete triad. Medicine And Science In Sports And Exercise [serial on the Internet]. (2013, May), [cited March 27, 2017]; 45(5): 985-996. Available from: MEDLINE.
- ↑ 9.0 9.1 Hoch A, Pajewski N, Moraski L, Carrera G, Wilson C, Gutterman D, et al. Prevalence of the female athlete triad in high school athletes and sedentary students. Clinical Journal Of Sport Medicine: Official Journal Of The Canadian Academy Of Sport Medicine [serial on the Internet]. (2009, Sep), [cited March 27, 2017]; 19(5): 421-428. Available from: MEDLINE.
- ↑ 10.0 10.1 Torstveit M, Sundgot-Borgen J. The female athlete triad exists in both elite athletes and controls. Medicine And Science In Sports And Exercise [serial on the Internet]. (2005, Sep), [cited March 27, 2017]; 37(9): 1449-1459. Available from: MEDLINE.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 11.6 Payne J, Kirchner J. Should you suspect the female athlete triad?. The Journal Of Family Practice [serial on the Internet]. (2014, Apr), [cited March 27, 2017]; 63(4): 187-192. Available from: MEDLINE.