Facial Palsy
Original Editor - Wendy Walker.
Top Contributors - Wendy Walker, Jess Bell, Kim Jackson, Redisha Jakibanjar, Vidya Acharya, Muhammad Umar, Lucinda hampton, Admin, Rishika Babburu, Evan Thomas, WikiSysop, Ahmed Essam, 127.0.0.1, Naomi O'Reilly, Tarina van der Stockt and Darine Mohieldeen
Topic Expert - Wendy Walker
Introduction[edit | edit source]
Facial palsy is due to the damage in the facial nerve that supplies the muscles of the face. It can be categorized into two based on the location of casual pathology:
- Central facial palsy- due to damage above the facial nucleus
- Peripheral facial palsy-due to damage at or below the facial nucleus[1]
Clinically Relevant Anatomy[edit | edit source]
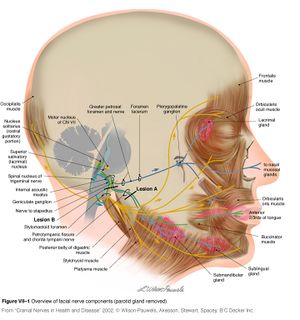
For more detail on the anatomy of the facial nerve, please see the Facial Nerve page.
The VIIth cranial Nerve has its nucleus in the Pons and takes a rather winding route before exiting the skull through the stylomastoid foramen. It then passes through the parotid gland, splitting into 5 branches: Temporal, zygomatic, buccal, mandibular and cervical.
See Facial Muscles Video :facial Muscles
Causes of Peripheral Facial Palsy[1][edit | edit source]
There are several causes of Facial Palsy:
- Idiopathic or Bell's palsy - Cause not known [2] but likely to be linked to Herpes Simplex infection [3]
- Tumour - A tumour compressing the facial nerve can result in facial paralysis, but more commonly the facial nerve is damaged during surgical removal of a tumour. The most common tumour to result in facial palsy during surgical removal is the Acoustic Neuroma (AKA Vestibular Schwannoma). Less commonly, cholesteatoma, hemangioma, Facial Schwannoma or parotid gland tumours (or the surgery to remove them) are the cause.
- Infection
- Ramsay Hunt Syndrome - Caused by Herpes Zoster infection = a syndromic occurrence of facial paralysis, herpetiform vesicular eruptions, and vestibulocochlear dysfunction. Patients presenting with Ramsay Hunt syndrome generally have a greater risk of hearing loss than do patients with Bell palsy, and the course of disease is more painful. Moreover, a lower recovery rate is observed in these patients.
- Lyme Disease - Infection with Borrelia burgdorferi via tick bites is another cause of facial paralysis. Of patients affected with Lyme disease, 10% develop facial paralysis, with 25% of these patients presenting with bilateral facial palsy.[4]
- Iatrogenic Facial Nerve Damage - Iatrogenic facial nerve injury occurs most commonly in temporomandibular joint replacement, mastoidectomy, and parotidectomy[5].
- Congenital
- Rare causes - These include:
- Neurosarcoidosis, Otitis media, Multiple Sclerosis, Moebius Syndrome, Melkersson-Rosenthal syndrome, Guillain-Barre Syndrome, Millard-Gubler Syndrome AKA Ventral Pontine Syndrome (Ipsilateral facial palsy with contralateral hemiplegia caused by involvement of the corticospinal tract along with paralysis of lateral rectus on the ipsilateral side due to the involvement of the abducent nerve), Foville Syndrome AKA Inferior Medial Pontine Syndrome (ipsilateral facial palsy, contralateral hemiplegia with ipsilateral conjugate gaze effects), Eight-and-a-half syndrome (facial palsy with Internuclear ophthalmoplegia and horizontal gaze palsy)
- Trauma, especially temporal bone fractures
Risk factors[edit | edit source]
- Diabetes
- Pregnancy - might be due to hypercoagulability, elevated blood pressure, increased fluid load, virus infection and suppressed immunity
- Exposure to cold
- Infection of ear
- Upper respiratory tract infection
- Obesity [6][7][1]
Clinical Presentation[edit | edit source]
Paralysis of the muscles supplied by the Facial Nerve presents on the affected side of the face as follows:
Appearance and Range of Movement:[edit | edit source]
- Inability to close the eye
- Inability to move the lips eg. into a smile, pucker
- At rest, the affected side of the face may "droop"
- The lower eyelid may drop and turn outward - "ectropion"
Functional Effects:[edit | edit source]
- Difficulty eating and drinking as lack of lip seal makes it difficult to keep fluids and food in the oral cavity
- Reduced clarity of speech as the "labial consonents" (ie. b, p, m, v, f) all require lip seal
- Dryness of the affected eye - see the Dry Eye page for more details
Somatic Effects:[edit | edit source]
The facial nerve supplies the lachrymal glands of the eye, the saliva glands, and to the muscle of the stirrup bone in the middle ear (the stapes). It also transmits taste from the anterior 2/3 of the tongue.
Facial palsy often involves:
- Lack of tear production in the affected eye, causing a dry eye, with risk of corneal ulceration.
- In Facial Nerve palsy there are 2 problems which contribute towards making the eye dry:
- The greater petrosal nerve, derived from the facial nerve, supplies the parasympathetic autonomic component of the lacrimal gland. - controlling the production of moisture/tearing in eyes.
- The zygomatic branch of the Facial Nerve supplies Orbicularis Oculi, and the resulting paralysis causes inability(or reduced ability) to close the eye or blink, so the tears (or indeed artificial lubrication in the form of drops, gel or ointment) are not spread across the cornea properly.
- Hyperacusis = sensitivity to sudden loud noises
- Altered taste sensation.
Differential Diagnosis[edit | edit source]
Upper Motor Neuron versus Lower Motor Neuron[edit | edit source]
If the forehead is not affected (ie the patient is able to raise fully the eyebrow on the affected side) then the facial palsy is likely to be a result of a lesion in the Upper Motor Neuron (UMN). Paralysis which includes the forehead, such that the patient is unable to raise the affected eyebrow, is a Lower Motor Neuron (LMN)lesion.
However, caution is advised in using preservation of forehead function to diagnose a central lesion. Patients may have to spare of forehead function with lesions in the pontine facial nerve nucleus, with selective lesions in the temporal bone, or with an injury to the nerve in its distribution in the face. It is worth remembering that a cortical lesion that produces a lower facial palsy/paresis is usually associated with a motor deficit of the tongue and weakness of the thumb, fingers, or hand on the ipsilateral side[8].
Diagnostic Procedures[edit | edit source]
- Laboratory investigations include an audiogram, nerve conduction studies (ENoG), computed tomography (CT) or magnetic resonance imaging (MRI), electromyography (EMG)[10].
- According to a clinical guideline, clinicians should not obtain routine laboratory and imaging testing in patients with new-onset Bell’s palsy.[7]
Outcome measures[11][edit | edit source]
- Sunnybrook Facial Grading System
- House-Brackmann facial nerve grading scale
- Linear Measurement Index
- Facial Disability Index
- Lip-length (LL) and Snout (S) Indices
- Five-Point Scale
Management / Interventions[edit | edit source]
Medical and surgical management depends on the cause of facial palsy.
Medical Management[edit | edit source]
Bell's Palsy and Ramsay Hunt Syndrome are treated with corticosteroids (prednisone), given within 72 hours of onset,[12]and this can be accompanied by antiviral medication[13].[14][15]
Surgical Management[edit | edit source]
Acoustic Neuromas or Facial Schwannomas are frequently resected surgically. See Acoustic Neuroma page for more details.
Patients at high risk of a corneal ulcer may be offered oculoplastic surgery to protect the eye.
For patients with dense facial palsy and no nerve function, a number of surgical interventions may be used. These fall into the following categories:
- Facial reanimation surgeries which involve nerve graft or anastomosis
- Facial reanimation surgeries which involve muscle transposition
- Static surgeries, ie. plastic surgery to improve symmetry at rest but no improvement in movement
Physiotherapy[edit | edit source]
- Neuromuscular Retraining (NMR) [16]
- Electromyography (EMG) and mirror biofeedback [17][1]
- Trophic Electrical Stimulation (TES) [18]
- Proprioceptive Neuro Muscular Facilitation Techniques[6]
- Kabath technique[19]
- Mime's therapy[20]
Evidence of Physiotherapy Treatments[edit | edit source]
- According to clinical practice guidelines, physiotherapy is not recommended in Bell's palsy.[7][21]
- Mime therapy can improve functionality for patients with facial palsy. The therapy must consist of exercises with mirrors, which are both low cost and easily available, and the patient must help in the execution of the movements for both biofeedback purposes and to prevent synkinesis.[11][20]
- Effect of electric stimulation is controversial.[1][22]
- PNF technique is effective than conventional exercises.[6]
- Kabath technique is effective than no exercise.[19]
Complications/Sequelae[edit | edit source]
Synkinesis (AKA aberrant regeneration) occurs after injury to the facial nerve. For more information on this, see the dedicated Synkinesis page.
Effects on Quality of Life[edit | edit source]
A large retrospective study [920 patients] published in September 2018 looked into the correlation between facial palsy severity and quality of life[23]; it concluded "A correlation between facial palsy severity and quality of life was found in a large cohort of patients comprising various etiologies. Additionally, novel factors that predict the quality of life in facial palsy were revealed".
Resources[edit | edit source]
Charity for Facial Palsy from any cause
Bell's Palsy Association, Charity
Information web-site on Bell's Palsy
Here's a link to the Facebook group for Facialpalsy.org
This link is to an introductory video about the effects of facial palsy
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Zhao Y, Feng G, Gao Z. Advances in diagnosis and non-surgical treatment of Bell's palsy. Journal of otology. 2015 Mar 1;10(1):7-12.
- ↑ Peiterson,E. Bell's Palsy; the spontaneous course of 2,500 peripheral facial nerve palsies of different etiologies. Acta Oto-Laryngologica. Supplementum 2002;549:4-30
- ↑ Holland NJ, Weiner GM. Recent developments in Bell's Palsy. BMJ 2004; 329(7465):553-7
- ↑ Clark JR, Carlson RD, Sasaki CT, et al. Facial paralysis in Lyme disease. Laryngoscope. Nov 1985;95(11):1341-5.
- ↑ Hohman MH, Bhama PK, Hadlock TA. Epidemiology of iatrogenic facial nerve injury: a decade of experience. Laryngoscope. 2014 Jan;124(1):260-5.
- ↑ 6.0 6.1 6.2 Gopalakrishnan, RAJALAXMI & Gmoorthy, Tharani & Gopinath, Yuvarani. (2018). COMPARISION OF PNF VERSUS CONVENTIONAL EXERCISES FOR FACIAL SYMMETRY AND FACIAL FUNCTION IN BELL’S PALSY. International Journal of Current Advanced Research. 7. 10.24327/ijcar.2018.9350.1542. available from: https://www.researchgate.net/publication/323254591_COMPARISION_OF_PNF_VERSUS_CONVENTIONAL_EXERCISES_FOR_FACIAL_SYMMETRY_AND_FACIAL_FUNCTION_IN_BELL'S_PALSY
- ↑ 7.0 7.1 7.2 Baugh RF, Basura GJ, Ishii LE, Schwartz SR, Drumheller CM, Burkholder R, Deckard NA, Dawson C, Driscoll C, Gillespie MB, Gurgel RK. Clinical practice guideline: Bell’s palsy. Otolaryngology–Head and Neck Surgery. 2013 Nov;149(3_suppl):S1-27.
- ↑ Jenny AB, Saper CB. Organization of the facial nucleus and corticofacial projection in the monkey: a reconsideration of the upper motor neuron facial palsy. Neurology. Jun 1987;37(6):930-9. [Medline].
- ↑ MedEdPRO Facial Palsy Upper and Lower Motor Neuron Lesions - Dr MDM Available from https://www.youtube.com/watch?v=5T4G27xkckE
- ↑ Kumar A, Mafee MF, Mason T. Value of imaging in disorders of the facial nerve. Top Magn Reson Imaging. Feb 2000;11(1):38-51. [Medline].
- ↑ 11.0 11.1 Pereira LM, Obara K, Dias JM, Menacho MO, Lavado EL, Cardoso JR. Facial exercise therapy for facial palsy: systematic review and meta-analysis. Clinical rehabilitation. 2011 Jul;25(7):649-58.
- ↑ ^ Gronseth, GS; Paduga, R (2012 Nov 7). "Evidence-based guideline update: Steroids and antivirals for Bell palsy: Report of the Guideline Development Subcommittee of the American Academy of Neurology". Neurology 79 (22): 2209–13.
- ↑ Daniel P Butler and Adriaan O Grobbelaar. Facial palsy: what can the multidisciplinary team do? J Multidiscip Healthc. 2017; 10: 377–381. Published online 2017 Sep 25. doi: 10.2147/JMDH.S125574
- ↑ De Almeida JR, Al Khabori M, Guyatt GH, Witterick IJ, Lin VY, Nedzelski JM, Chen JM. Combined corticosteroid and antiviral treatment for Bell palsy: a systematic review and meta-analysis. Jama. 2009 Sep 2;302(9):985-93.
- ↑ Salinas RA, Alvarez G, Daly F, Ferreira J. Corticosteroids for Bell's palsy (idiopathic facial paralysis). Cochrane Database of Systematic Reviews. 2010(3).
- ↑ Manikandan N. Effect of facial neuromuscular re-education on facial symmetry in patients with Bell's palsy: a randomized controlled trial. Clin Rehabil. 2007 Apr;21(4):338-43.fckLR*Electromyography (EMG) Biofeedback <ref>Bossi D, Buonocore M et al. Usefulness of BFB/EMG in facial palsy rehabilitation. Disabil Rehabil. 2005 Jul 22;27(14):809-15.
- ↑ Bossi D, Buonocore M et al. Usefulness of BFB/EMG in facial palsy rehabilitation. Disabil Rehabil. 2005 Jul 22;27(14):809-15
- ↑ Targan R S, Alon G, Kay SL. Effect of long-term electrical stimulation on motor recovery and improvement of clinical residuals in patients with unresolved facial nerve palsy Otolaryngol Head Neck Surgery February 2000 vol. 122 no. 2 246-252
- ↑ 19.0 19.1 Monini S, Iacolucci CM, Di Traglia M, Lazzarino AI, Barbara M. Role of Kabat rehabilitation in facial nerve palsy: a randomised study on severe cases of Bell's palsy. Acta Otorhinolaryngologica Italica. 2016 Aug;36(4):282.
- ↑ 20.0 20.1 Beurskens CH, Heymans PG. Mime therapy improves facial symmetry in people with long-term facial nerve paresis: a randomised controlled trial. Australian Journal of Physiotherapy. 2006 Jan 1;52(3):177-83.
- ↑ de Almeida JR, Guyatt GH, Sud S, Dorion J, Hill MD, Kolber MR, Lea J, Reg SL, Somogyi BK, Westerberg BD, White C. Management of Bell palsy: clinical practice guideline. Cmaj. 2014 Sep 2;186(12):917-22.
- ↑ Teixeira LJ, Valbuza JS, Prado GF. Physical therapy for Bell's palsy (idiopathic facial paralysis). Cochrane database of systematic reviews. 2011(12).
- ↑ Tavares-Brito J, van Veen MM, Dusseldorp JR, Bahmad F Jr, Hadlock TA Facial Palsy-Specific Quality of Life in 920 Patients: Correlation With Clinician-Graded Severity and Predicting Factors. Laryngoscope. 2018 Sep 12. doi: 10.1002/lary.27481. [Epub ahead of print]