Equipment for individuals with limb deficiency
Original Editor - Ahmad Al-Mosa Al-Malkawi as part of the WCPT Network for Amputee Rehabilitation Project
Top Contributors - Leslie Angama, Tony Lowe, Admin, Kim Jackson, Tarina van der Stockt, Jess Bell, Amanda Ager, 127.0.0.1 and Claire Knott
Introduction [edit | edit source]
Individuals with amputation are in need of a proper rehabilitation program as early as possible and generally require compensatory equipment to reach maximum functional independence.
The prescription of an appropriate assistive device or walking aid will involve a multidisciplinary team evaluating many different factors and also should involve the patient in this decision.
Risk assessment [edit | edit source]
Risk factor assessment tools[edit | edit source]
The causes of falls vary for different age groups and can lead to serious outcomes. Risk factor assessment tools are utilised to identify the issues around the potential of falls for an individual patient.
Example gait and balance assessment tools [1] include:
- Timed up and Go (TUG)
- Timed Up and Go TestBerg Balance Scale (BBS)
- Berg Balance ScaleTinetti Performance Oriented Mobility Assessment (POMA)
- Tinetti testDynamic Gait Index
- Dynamic Gait Index
- Dynamic Gait IndexGet Up and Go test.
These assessment tools measure a person's ability to balance and to walk in an appropriate way. They determine how long the person can keep their balance during gait, as well as considering a few activities of daily living (ADL) while moving from one point to another.
The ulitmate aim of using these tools are to identify issues that can be taken into account in the management of this patient and so reduce their likelihood of experiencing a fall. Potential issues identified could include:
- Mental problems.
- Language difficulties.
- Short term verbal memory.
- Construct ability.
- Calculation problems.
Falls Risk Assessment and Management Plan (FRAMP)[edit | edit source]
FRAMP [2] is a comprehensive tool that evaluates a patient's risk of falls from the early stage of hospitalization. FRAMP uses three similar stages of assessment during a specific period of time which identifys the history of falls, use of walking aids, cognitive impairment and other urinary and fecal problems.
FRAMP includes individualized intervention for specific risks such as:
- Mobility risks.
- Functional ability risks.
- Medication/ Medical condition risks.
- Cognitive state risks.
- Continence/ elimination risks.
Each one of the above risks is assessing the level of a patient's ability to perform the test with an appropriate intervention for each problem.
FRAMP also provides a minimum intervention to be applied to all patients which are:
- Provision of information for the patient about their environment (Toilet, bed and ward) and the use of the call bell to facilitate their needs.
- Education of patients about mobility aids and to enable them to use it in the proper way.
- Improve their awareness about the conditions that increase their risks of falls in order to prevent it.
- Improve the quality of the surrounding environment to reduce the risk of falls (lighting and remove obstacles).
Wheelchairs[edit | edit source]
Manual Wheel chair[edit | edit source]
The WHO[3] defined the manual wheel chair as: “Wheel Chair propelled by the user or pushed by another person, and it is appropriate when it meet the user needs and environmental condition”. According to WHO statistics 2008 [3]; 10% of 650 million Persons with disabilities (PwDs) are in need of a Wheel Chair, which reflects the huge need for a wheel chair and the resources needed to provide them.
Wheelchairs are important for individuals with disability:
- To avoid immobility and being bed ridden.
- To prevent secondary complications.
- To involve their users in community activities.
- To increase the opportunity for education, employment, and social interaction.
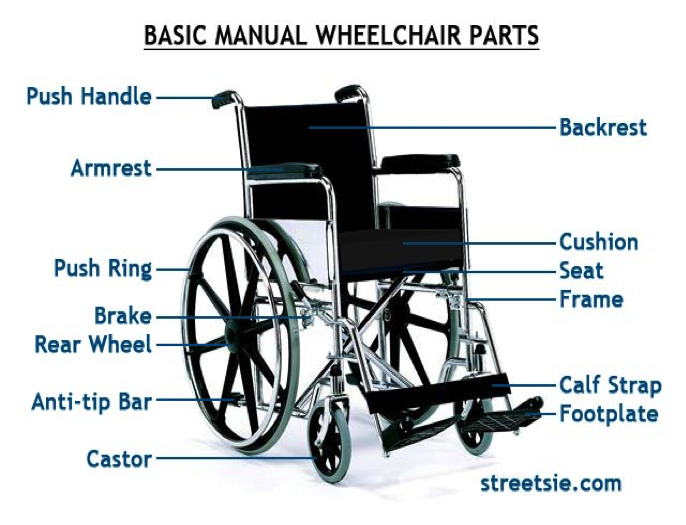
The picture below shows the main components of a wheel chair.
According to the International Labor Organization(ILO) individuals with disability have a low employment rate with 80 % or more unemployed in low resourced countries which makes their living conditions worse.
The majority of these individuals with disability are living in developing countries, so the infrastructure and living environment also present physical barriers to access. They also lack related rehabilitation Services, which reduces the level of awareness and education in the community, as well as limits the ability to meet the users needs in wheel chair design.
Type of Wheel Chairs:[edit | edit source]
There is huge variation in the type of the wheel chairs, and no single wheel chair will suit all users when considering their physical and environmental needs. The appropriate wheel chair for a user is the wheel chair which can to provide good safety and comfort, that fulfills the user’s physical and environmental needs to become mobile, healthy, and participate in the community.
Foldable wheel chairs are used for the transportiation. A wheel chair can have extra support padding or cushions to address postural needs. A wheel chair that will be used indoors will be different from the one used outdoors.
Functional Performance[edit | edit source]
A wheel chair's functional performance is how well it fulfils it's user's needs in their particular environment [3]. So it is the performance of the wheel chair for a specific user in their specific environment.
The evaluation of wheel chair design for functional performance includes the evaluation of its static and dynamic stability, its rolling capacity and resistance, the access to repairs and spare parts, and its overall dimensions, mass and required turning space.
For example when a wheel chair user has a bilateral above knee amputation his Centre of Gravity will be further back. So a wheel chair for this user needs to have its rear wheel positioned farther back behind the center of gravity for the user in order to have a good functional performance for this user.
Pressure Relief[edit | edit source]
As an early stage for the rehabilitation of amputee patients postoperatively and especially with bilateral amputees, they will need to depend on the wheel chair, therefore they will might use it for long period during the day which might put them at risk of developing pressure sores if they don't follow instructions and complete appropriate exercises.
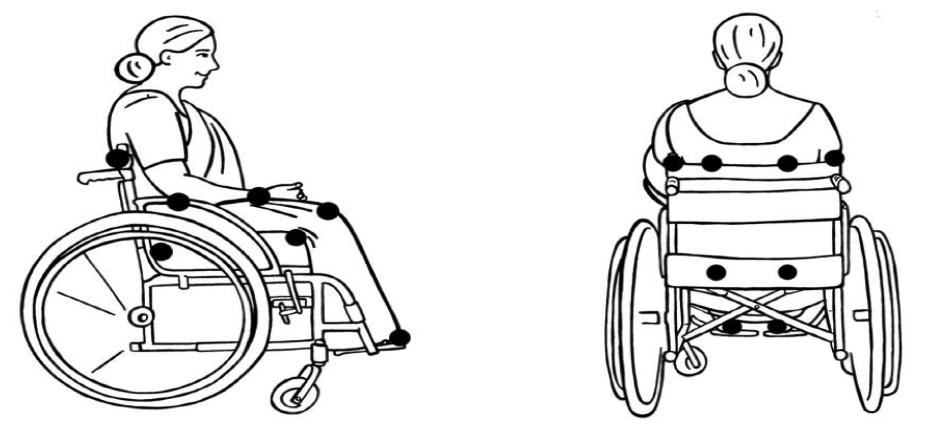
The diagrams below show the most sensitive areas for a pressure sore [3]
Pressure relief exercises [4]:
The use of an appropriately modified wheel chair with cushiosn can help in both decreasing the risk and in practicing the exercises. The common exercises used are:
- Independent push up.
- Leaning from side to side.
- Leaning forward.
Very Important: Don’t forget to instruct the patient to lock the brake while exercising.
The video below demonstrates pressure relief exercises [5]:
http://www.naric.com/?q=en/content/pressure-relief-techniques-manual-wheelchair
Manual Handling Equipment[edit | edit source]
When it’s difficult to avoid manual handling it’s possible to reduce the related complications and risk by adapting the working environment or systems used for the benefit of the patient and care giver.
This handling equipment will vary in usage from one person to another due to their disability, age, severity of the case and socioeconomic status. Example equipment includes: transferring board, wheel chair, transferring sheet, stretcher, shower and bath equipment, standing hoist, transfer belt and other equipment.
The main activities involved in patient moving and handling are:
- Sitting, standing and walking.
- Bed mobility.
- Lateral Transfer.
- Hoisting.
Handling and safety[edit | edit source]
Poor pratice in the handling process canl lead to serious injuries in the carer like: LBP, disc problems and muscles strain. According to the Health and Safety Authorities 2011 [6], for the safety of both patient and the caregiver many issues should be considered:
- The surrounding environment, ergonomic and workplace design should meet the needs of both the individual with disability and the carers.
- The patient’s situation and degree of disability determine the kind of equipment involved in the handling process.
- Qualified staff and trainees assisting in the process of shifting and transferring.
- Staff must follow best practice guidance for safe manual handling.
Early walking Aid (EWA)[edit | edit source]
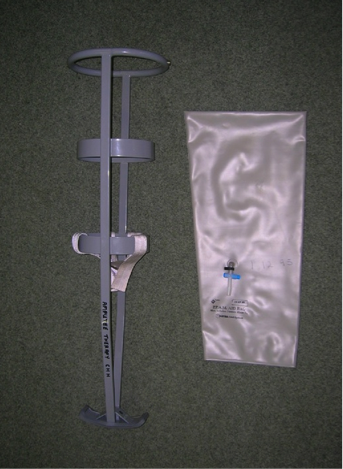
The early walking aid (EWA) is a temporary socket made up from an inflatable bag, supported by metallic frame with padded safely rings with a prosthetic or rocker foot [7].
The EWA has been used to help in patient assessment and to start the treatment. One of the most important objectives of the EWA is to help the patient ambulate in an upright posture as early as their wound condition alows which will help patient psychological status. Also the EWA can accelerate the rehabilitation process through starting gait training and facilitating prosthesis fitting.
The use of a EWA helps to improve balance, posture and sensory integration. The pressure provided by the air bag also helps to control the oedema, and decreases pain.
Types of EWA [8]:
- Pneumatic using air bag.
- Vacuum Technique as LIC Tulip.
- Preformed Plastic Socket as LIC Femorett, LIC LEMA, and Hexilite temporary patellar tendon Weight bearing.
- Local Variations.
plastic socket EVA pneumatic using airbag
Application of EWA [8] [7] [9]:
According to (Enstgrom and Van de Ven 1999) [9]; training with a Pneumatic EWA can start 7 to 10 days postoperatively, with gradual increasing of the pressure taking into consideration the wound condition.
Special consideration during the application:
- Usually starting the air inflation with 15 to 25 mmHg.
- Gradual increase of the pressure to a limit of 40 mmHg.
- Adapt the pressure according to the patients’ attitude to amputation, stability, recovery, and comfort.
- Continue inspection and observation of the wound as needed.
- Weight bearing should be restricted according to the physician's order.
Prostheses[edit | edit source]
Please see the prosthetics page.
Walking Aids[edit | edit source]
A patient with an amputation can use a walking aid, either temporary or permanent to restore the functional ambulation and independency. The choice of aid is dependent on the level of fitness, strength, balance skills, and risk of falls. In addition the walking aid will help to control the allowed weight bearing on the injured leg, compensate the lack of balance, and decrease the risk of fall.
Named, Types, Advantages, Disadvantages, and Adjustment[edit | edit source]
Watch the video below explaining how to choose and use some assistive devices:
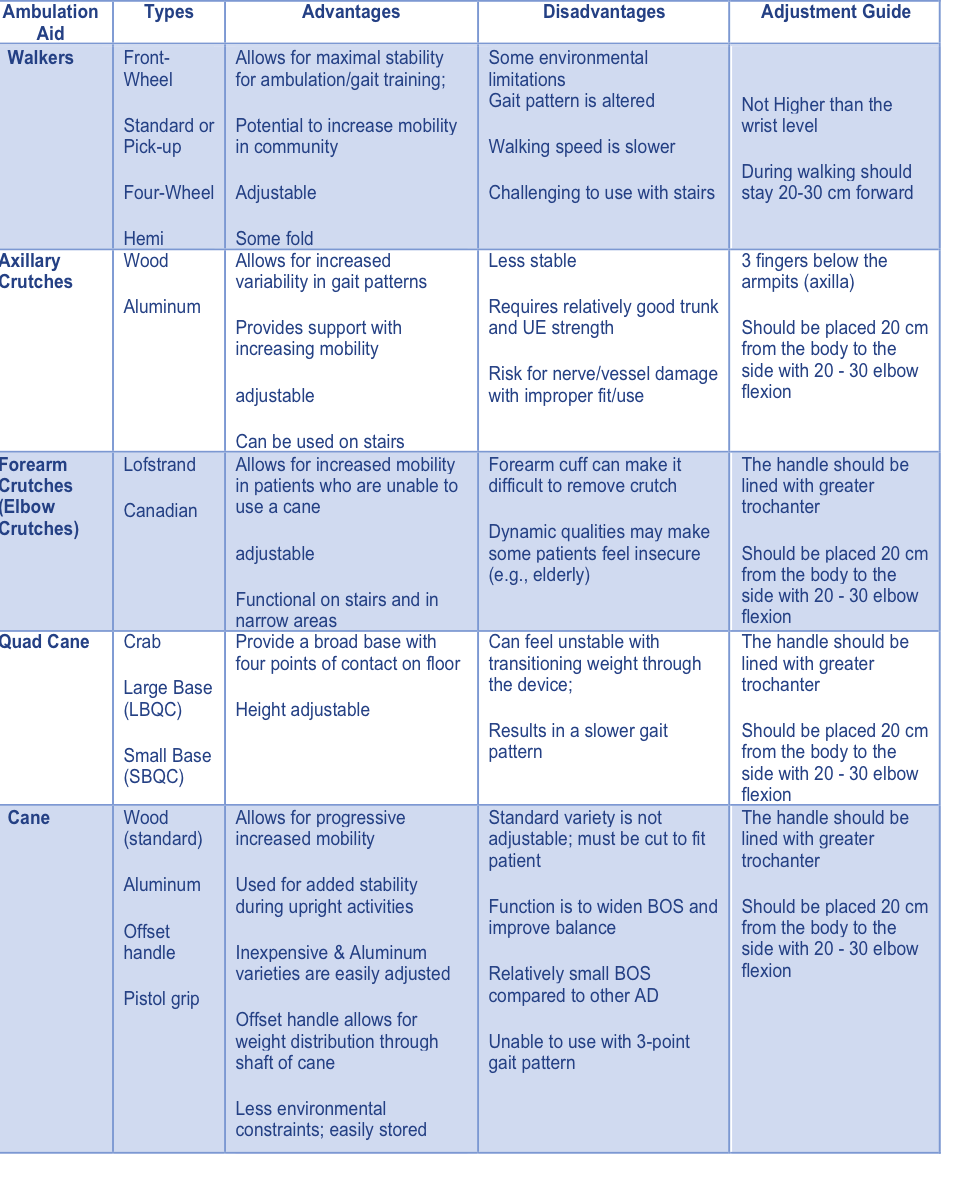
The table below explains different types of walking aids, the advantages, the disadvantages and the adjustment guide [10] [11]
Special considerations for walking aids[edit | edit source]
Our long term goal with amputee patients it to reach maximum functional independency without walking aids, a special consideration should be taken such as [11] [12]:
- Some patients can’t achieve this goal due to their age or another medical problem.
- Ambulation using a walker is not a required step to shift the patient from the parallel bar to crutches or cane, if their physical and medical condition allows.
- Usually when using a single walking aid it should be handled on their sound side, however it can be used on the amputation side if the goal is to shift more weight to this side.
- The drill to ascend and descend the stair is to ascend with the sound leg, and descend with the amputee side (Up good and down bad).
- A proper selection of a walking aid with proper adjustment will speed up the rehabilitation process and improve the quality of the outcomes.
Other equipment for physiotherapy units[edit | edit source]
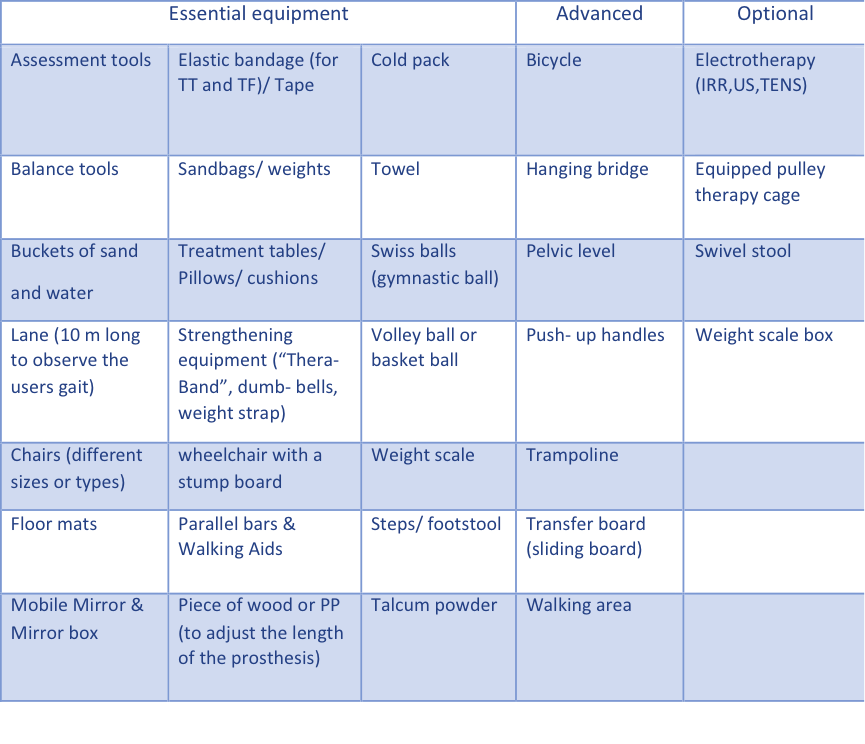
There are many items of equipment that are required in the rehabilitation of amputees. Below is a table which outlines many of these and classifies them as essential, advanced and optional. [13]:
References[edit | edit source]
- ↑ (1) Risk Factor Assessment Tools, Minnesota Falls Prevention website: http://www.mnfallsprevention.org/professional/assessmenttools.html
- ↑ (2) Falls Risk Assessment and Management Plan (FRAMP) ,Fall Risk Assessment Australia: http://www.healthnetworks.health.wa.gov.au/docs/FRAMP-Statewide-Template.pdf
- ↑ 3.0 3.1 3.2 3.3 (3) Guidelines on the provision of manual wheelchairs in less-resourced settings, Chapter 1 Introduction, World Health organization, Geneva, 2008 http://www.who.int/disabilities/publications/technology/wheelchairguidelines/en/
- ↑ (5) Pressure Relief in a Manual Wheelchair, National Spinal Cord Injury Association (NSCIA), A Program of United Spinal Association, 2011, NY 11370 / 718-803-378: http://www.spinalcord.org/resource-center/askus/index.php?pg=kb.page&id=2427
- ↑ (6) Pressure Relief in a Manual Wheelchair, National Spinal Cord Injury Association (NSCIA), A Program of United Spinal Association, 2011, NY 11370 / 718-803-378 http://www.naric.com/?q=en/content/pressure-relief-techniques-manual-wheelchair
- ↑ (7) Guidance on the Management of Manual Handling in Healthcare, The Health and Safety Authority, 2011, the Metropolitan Building, James Joyce Street, Dublin 1 http://www.hsa.ie/eng/Publications_and_Forms/Publications/Occupational_Health/Guidance_on_the_Management_of_Manual_Handling_in_Healthcare.39324.shortcut.html
- ↑ 7.0 7.1 (8) The early Rehabilitation of Lower Limb Amputees using a Pneumatic Walking Aid, R.G.Redhead, 1983, London. http://www.oandplibrary.org/poi/1983_02_088.asp
- ↑ 8.0 8.1 (9) Limb Amputation: From Etiology to Rehabilitation, the Postoperative Phase, Early Walking Aids, By R. Ham and L. T. Cotton, 1991, UK.
- ↑ 9.0 9.1 (10) Tidy's Physiotherapy 13th Edition, Physiotherapy for Amputees, The Pre-prosthetic Stage, Edited by Stuart B. Porter, 2003, UK.
- ↑ (11) Gait Training with Ambulation Aids, PTA 104L Orthopedic Dysfunctions Lab http://media.lanecc.edu/users/howardc/PTA104L/104LAmbAids/104LAmbAids_print.html
- ↑ 11.0 11.1 The Rehabilitation of People with Limb Amputation, World Health Organization, 2004, USA, http://issuu.com/quetechceus/docs/amputee-rehabilitation/1
- ↑ Walking Aids, Special considerations about walking aids, ICRC, PDF Walking aids.
- ↑ Prosthetic Gait Analysis for Physiotherapists, Materials and equipment, International Committee of the Red Cross(ICRC) , 2014, Geneva, https://members.physio-pedia.com/open-ebooks/prosthetic-gait-analysis-for-physiotherapists