Subjective Assessment of the Equine Patient
Introduction[edit | edit source]
Animal physiotherapy is an emerging profession[1]. Physiotherapists who
treat human use their skills to treat animals. Usually, the process of physiotherapy assessment in animals starts by referral from a veterinary surgeon who co-operates with physiotherapists as a multidisciplinary team in the assessment, treatment and rehabilitation of animals[1].[2] Physiotherapists provide a functional assessment to identify pain or loss of function caused by pain, injury, disorders or disability. Equine athletes and their riders now access a team of professionals including physiotherapists.[1]
Process oF Assessment[edit | edit source]
Physiotherapy assessment does not require a pathoanatomic diagnosis to develop a treatment plan[2]. In contrast, physiotherapists use a more functional approach to assess the horse by the way of observing and identifying movement dysfunctions or impairments and using their clinical reasoning to relate what they observe and also palpate to the presenting problem.[3]
There is some basis for Physiotherapy assessment in equine[3]:
- Good communication skills with the owner, handler, and trainer.
- Good powers of observation in both static and dynamic status.
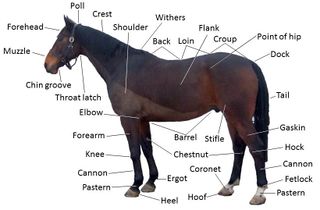
- Knowledge of anatomy, functional anatomy, and biomechanics of the horse.
- The ability to perform or direct functional movement tests, good palpation skills and the ability to interpret all of these assessments.
Subjective Assessment[edit | edit source]
Subjective assessment in equines is limited as unlike humans it is very difficult to determine SIN, 24- hour pattern[3]and the exact area of pain/ discomfort. Due to this gathering info from as many different sources is very important ie veterinarian, farrier, the rider. trainer, groom and owner. Collecting data could be done through:[2]
- Background Information[2]: Important to have background information so that you can ID the horse and contact the MDT for information.
- Discipline, training hx, the reason for referral: Clues to the type of injury, MOI and cause of injury i.e. over-training.[2]
- Present Medical History: What is the problem and how has it been assessed? What treatment has been given thus far and how has the horse responded?[2]
- Past Medical History: Clues to if the previous injury as it may be causing the current issue, what the horse responds to in Rx and was there enough rehabilitation?[2]
- Special questions /Red flags: Similar to human patients ie sudden weight loss, general health, respiratory conditions ...etc.[2]
Unlike human physiotherapy, you can not interview the patient thus you often have to interview the team to find out all the information you need by asking:[2]
- Rider: what they are feeling during training.
- Coach: what they are seeing during training.
- Owner & Groom: How is the horse at home and are there any abnormal behaviours.
- Vet & other med professionals: What was found on examination and investigations. All of this can assist in formulating a treatment plan.
There are some factors that could help in the assessment process;
1- AGE[edit | edit source]
Gives us clues to the type of pathology and can be considered a differential diagnosis.
YOUNG HORSES (2-6 years)
- Developmental problems i.e. OCD.
- Injuries related to poor motor control to cope with work demands. Still developing soft tissue structures.
- Competing racehorses under huge stress.
MID-AGED HORSES (7-15 years)
- Competing often at a peak in sport horses, therefore, soft tissue injuries due to overuse.
- Biomechanical problems will also cause soft tissue injuries.
- DJD sometimes present already.
OLDER HORSES (15-20 years)
- Wear and tear especially joints i.e. DJD/Arthritis.
2- GENDER[edit | edit source]
Hormonal changes can mimic the behavioural changes associated with musculoskeletal pain.
- A common behavioural problem can occur in performance mares when these mares exhibit heat or oestrus. Mares begin periods of heat due to increasing day length. In general, these periods of heat last 5 to 7 days out of a 21-day cycle. Clinical signs that affect performance mares include attitude changes, tail swishing, difficulty in training, squealing, horsing, excessive urination, kicking, decrease in performance, and colic like pain associated with ovulation.
- Question the owner or rider regarding previous problems with oestrus, or whether there appears to be a regular monthly pattern to the pain or performance-related symptoms they are experiencing with their mare.
3- Length Of Ownership[edit | edit source]
- During the change of ownership, it is very rare that all the previous medical history is passed on. We are guided by pre-purchase vetting and unfortunately, not all previous MSK history will present its self in a vetting.[2]
- One of the greatest tools we use to identify MSK pain or discomfort is behaviour, it is important to note that new owners may not know what is ‘normal’ behaviour for their horse yet.
4-DISCIPLINE & TRAINING HX[edit | edit source]
- Discipline&level, It’s important to understand what discipline and level as it will help determine what injury/ problem the horse has, the mechanism of injury (MOI) and the severity. I.e. dressage horse is susceptible to.[2]
- LAST COMPETITION: This will give you an idea when last the horse was possibly put under great strain or how long the horse has been out for
- TRAINING PROGRAM: It is important to determine how often is the horse working and what are they doing? Are they cross-training and variety of work? I.e. pole work, jumping, flatwork, hill work or track work and hacking.[2]
5- PRESENT MEDICAL HX[edit | edit source]
- What is the main complaint or what behavioural issue does the horse present with that made the owner phone us i.e. the horse recently started biting[4] while being tacked up or the horse has stopped wanting to work forward?
- How long has the complaint or issue been present for?
- Has the VET seen the horse and what investigations, were done? Was there a diagnosis? Medications prescribed & for how long?
- 24-hour pattern more or less i.e. does the horse worsen with work or improve? Is the horse worse on walking out the stable in the morning? Please also note how long does it take for the horse to improve?
- Are there any other professionals involved? What did they do and did it help to any degree i.e. saddle, fitter, dentist, chiro etc.
6- PAST MEDICAL HX[edit | edit source]
Not always available/ accurate
- What VETERINARY treatment has the horse had?
- A good start is to look at what was picked up on the pre-purchase vetting.
- Was there a pre-purchase vetting?
Vetting is an opportunity for a vet to conduct a comprehensive general check-up on a horse, at which time certain problems may be discovered. On extensive vettings, x-rays are also conducted. However, it is important to note that it is often the expense of the horse which determines how extensive the vetting is or if there is even a vetting. In some cases with expensive horses or horses with great potential are x-rayed every few years as preventative medicine. It is important to note that these horses may not be symptomatic, however, the therapist should find if the horse’s veterinarian has ever recommended further diagnostic tests that have not been done by the owner.
7- RED FLAGS[edit | edit source]
- General health (MEDICAL) questions Metabolic diseases such as Cushing’s, Respiratory diseases such as COPD
- Medications/ supplements that the horse may be on. Remember that your Subjective assessment must give you an indication of:
- What/where to look for the source of the problem?
- Whether something is not adding up/ making sense – requires a referral?
OBJECTIVE ASSESSMENT[5][edit | edit source]
The stages of the functional assessment:[3]
- Active physiological movements.
- Soft tissues—palpation and testing.
- Passive physiological joint assessment.
- Passive accessory joint assessment.
Objective physiotherapy tests in the equine assessment are very much based on functional assessment and palpation skills. Which consists of four elements[5][6]
| 1- Functional Assessment | 2- ROM | 3- Palpation | 4- Special Tests & Neurological Ax |
|---|---|---|---|
| Conformation, Gait, Reflexes | Baited stretches, Reflexes, Limb ROM | Temp, Swelling, Bony landmarks, Muscular | Neurological tests |
CONFORMATION:[7]
POSTURE:
|
It is very difficult to do an active ROM assessment on most of the joints in isolation. Thus we try note ROM in
functional movements and test passively. However, we can use baited stretches to test cervical and thoracic movements as well as reflex tests. |
||
| CONFORMATION & POSTURE AX[7]
Observe the horse standing on a flat, firm surface.
most comfortable standing?
View from the left, right, front and rear.
|
BACK CONFORMATION[7][edit | edit source]
Typically horses back should be 1/3 of the body from the highest vertebra of the whither to the point of the hip. Long backed horses are generally more flexible however can be prone to injury as they generally find it harder to work correctly and strengthen their core. Short backed horses are generally strong but more ridged and can be difficult when fitting saddles as they ”run out” of the thoracic spine.
|
Conformational Faults[7] |
Explanation | Predisposed issues |
|---|---|---|
| Base Wide | Standing with forelimbs outside the plumbline. | Medial stress on joints, medial splint bone stress |
| Base Narrow | Standing with forelimbs inside the plumbline. | Lateral sidebone, lateral heel bruises and lateral strain on joints |
| Toed Out | Toes pointing outward | Inward arc when advancing; results in interference with opposite forelimb especially if combined with base- narrow stance. |
| Pigeon Toed | Toes pointing inward | Outward deviation of foot during flight (paddling or winging-out) resulting in interference
with hind limb |
| Bowlegged | Varus deformity of carpus | Increased tension on the lateral collateral ligament and medial surface of carpal bones |
| Knock-Kneed | Valgus deformity of carpus | Increased stress on medial carpal collateral ligaments, outward rotation of cannon bone,
fetlock and foot |
| Camped Out | Entire forelimb from body to ground is
too far forward |
Seen in navicular syndrome and laminitis |
| Calf Kneed | Backward deviation of carpus | Carpal chip fractures, injuries to check ligaments |
| Camped Under | Entire limb below elbow placed too far underbody; can occur
with a disease as well as be a conformational fault. |
Overloading of forelimbs, shortened cranial phase of stride and low arc of foot flight can lead to stumbling |
| Buck Kneed | Forward deviation of carpus; knees
knuckle forward so dangerous for rider |
Strain on sesamoid bones, suspensory ligament,ligament, and SDFT and extensor
carpi radialis muscle |
| Sickle Hocked | Excessive angulation of the hock (<53) | High stress on hock and ligaments |
| Post Legged | High stress on back of hock joint and
the soft tissue support structures | |
| Cow Hocked | Medial deviation of the hocks and
accompanied by base wide from hocks to feet. |
Excessive stress on hock leads to bone
spavin |
| Base Narrow | Distance between hooves less than
centre of the thighs, heavily muscled horses (often accompanied by ‘bowlegs’ with hocks too far apart) |
Strains to lateral structures of limb |
| Base Wide | Distance between hooves greater than
distance between centre of thighs; commonly associated with cow-hocks. |
Strains to medial structures of limb |
HOOF PASTERN AXIS[7][6][edit | edit source]
Although we are not Farriers it is important to understand the hoof conformation and its axis as it may interfere with joints and ligaments above.It is an imaginary straight line running from the centre of the fetlock, through the pastern, continuing straight from the coronet to the ground surface[8].
- 48 – 55 degree angle =NORMAL
- 45 degree angle or less = SLOPING
- 60 degree angle or more = UPRIGHT
Broken back = when the imaginary line running through the fetlock and pastern is broken at the coronet through to the ground surface.The hoof is at a lesser degree angle compared to the pastern. Strain on the tendons and may cause wear on the navicular.
Broken Forward = when the imaginary line running through the fetlock and pastern is broken at the coronet through to the ground surface. The hoof is at a greater degree angle compared to the pastern. Strain on the joints above.
Gait Assessment[5][3][edit | edit source]
When performing a gait assessment in hand have the horse:
- Walk away from you, past you and towards you
- Trot away from you, past you and towards you
- Walk in a circle with limbs crossing (Turn on the forehand)
- Rein back
- Trot on a circle in both directions (Usually on the lunge)
It is important to note the surface you are examining on as it can influence the lameness if any. As a rule of thumb soft tissue lameness, ie tendons/ ligaments will generally show greater lameness in soft or deep going such as a sand arena,
Joint lameness is usually more evident on hard ground. Trotting on bricks or concrete can sometimes help you assess lameness through hearing the foot- fall rhythm.
GRADING LAMENESS[5]
There are many types of scales which grade lameness. The most widely accepted grading is the American Association of Equine Practitioners (AAEP) scale. The vets commonly use the lameness locator to assess lameness. This is a machine which analysis's movement through motion sensors. It objectively quantifies how a horse moves through space and bears weight.[9]
| Grades | lameness is |
|---|---|
| Grade 1 | Difficult to observe ,not consistently apparent,just in weight- bearing or circling in inclines or hard surfaces |
| Grade 2 | Difficult to observe at walk or trotting in straight line , consistently apparent when weight bearing or circling on inclines or hard surfaces |
| Grade 3 | consistently seen at trots under all circumstances |
| Grade 4 | Obvious with marked head nodding or short stride |
| Grade 5 | Obvious with minimal weight-bearing, in motion or and at rest. inability to move. |
FLEXION TEST[edit | edit source]
A flexion test is a preliminary veterinary procedure performed on a horse, generally during a prepurchase or a lameness exam.The animal's leg is held in a flexed position for approximately a minute, and then the horse is immediately trotted off and its gait is analysed for abnormalities and unevenness.[3]
- A flexion test is a preliminary veterinary procedure performed on a horse, generally during a prepurchase or a lameness exam.
- The flexion places stress on the joint capsule and soft tissue of the joint,and sometimes the cartilage and bone, usually accentuating any lameness
that is present, such as arthritis. The horse may take a few uneven steps, or may be lame for several minutes following the procedure.
- Flexion tests are non-specific.
ACTIVE ROM[5][edit | edit source]
- It is very difficult to do an active ROM assessment on most of the joints in isolation. Thus we try note ROM in functional movements and test passively. However we can use baited stretches to test cervical and thoracic movements as well as reflex tests.
REFLEXES[edit | edit source]
VENTRODORSAL LIFT REFLEX (whither lift): Tests: Thoracic vertebra flexion[5]
Preformed:. A firm pressure applied with fingernails, pen cap or blunt hoof pick to the midline of the level of the girth. Causes the horse to ‘lift’ the cranial thoracic region.
LATERAL REFLEX: Tests: Lateral flexion
Preformed: A firm pressure applied with fingernails, pen cap or blunt hoof pick to the bricep femoris line on the contralateral side and around the buttocks. Causes the horse to laterally flex the lumbar region and caudal thoracic region. Watch ROM.
ROUNDING REFLEX:Tests: lumbar flexion[5]
Preformed: A firm pressure applied with fingernails, pen cap or blunt hoof pick to the caudal border of biceps fem bilaterally. Ensure you are standing to the side of the horse and beware of being kicked. The horse will flex. Watch for rotation and ROM.
EXTENSION REFLEX: Tests lumbar or Thoracic extension
Preform: Standing on a box behind the horse, draw your fingers or two hoof picks caudally along the lumbar/ thoracic paravertebral musculature. Observe for quantity and symmetry of movement.
BAITED STRETCHES[edit | edit source]
Stretches used to test active movement of the cervical and cranial thoracic regions. During these movements the therapist uses a treat to encourage the movement. Remember to compare left and right of lateral movements.[5]
BAITED STRETCHES – CX SPINE[5][edit | edit source]
CERVICAL EXTENSION: Guide the horses muzzle upwards and forward with a treat with a treat[7]
CERVICAL FLEXION: Guide horse’s muzzle towards upper chest to effect a nodding movement (at the poll).[3]
For caudal cervical spine[5]
Flexion: For lower cervical/upper thoracic flexion, guide horse’s muzzle down between fetlocks (or observe horse grazing – check for even weight distribution between forelimbs); also guide horse’s muzzle towards sternum to check mid-cervical flexion.[3]
Lateral flexion: Guide muzzle around along horse’s lateral trunk towards the flank and compare range side to side.
Lateral flexion/flexion: Guide muzzle around towards the carpal region and compare range side to side.
BAITED STRETCHES:TX SPINE[5][edit | edit source]
It is important to not that when testing caudal cervical spine you will get some thoracic movement of flexion and lateral flexion.
PASSIVE ROM – HEAD & NECK[5][edit | edit source]
Extension: Guide muzzle upwards and stabilise with one hand gently over C1. Apply gentle overpressure from underneath the muzzle. Assess end-feel.[2]
Flexion: Guide muzzle towards the upper chest; stabilise with one hand gently over C1 and apply gentle overpressure to the front of the muzzle. Assess end-feel.[2]
Rotation: Stabilise with one hand over C2 and guide horse’s muzzle toward you on an rotatory axis. Apply gentle overpressure via the muzzle. Compare range of motion and end-feel side to side[2]
Lateral flexion: Motion at each cervical level between C3–C6 can be assessed by palpating the ‘opening’ of the cervical vertebra when an assistant laterally flexes the horse’s neck away from the assessor. Or: Stabilise with one hand over the vertebral body to effectively ‘block’ motion from the chosen level caudal, and gently guide the horse’s muzzle toward you, in a lateral flexion direction. Apply gentle overpressure; assess range of motion and end-feel and compare side to side.[3]
PASSIVE ROM – THORACIC SPINE[edit | edit source]
Passive testing: Very difficult due to deep joint levels, tight connective tissue structures and restrictive facet joint morphology. Globally one can mobilise the whither however there is very little movement.Some rib springing sometimes possible depending on soft tissue tone.[2]
PASSIVE ROM – LUMBAR[edit | edit source]
Unilateral DV mobs,standing on a tall box or step, apply a gradual downwards force over the transverse process of each consecutive lumbar vertebra. Repeat on the other side.
Central DV L5 & L6,Standing on a tall box or step, apply a gradual downwards force over the spinous processes of L5 and L6. Horses with pain in this area (usually ligamentous in origin) will dip away from the pressure. Non-painful horses will show no response (and no movement should be palpable)
Lateral mobs, Standing on a tall box, stablise the lumbar segment above the testing vertebra and grip the dock of the tail with your other hand. Pull gently on the dock towards you and grade the mobs.
AX of SIJ[5][edit | edit source]
ACTIVE TESTING, Weight-bearing weight displacement,Stand on a box behind the horse (or next to the horse if you suspect he may kick). Palpating the tuber sacrale bilaterally, have an assistant lift one hindleg. Feel for a slight cranial shift of the contralateral tub sacrale as the SIJ of the weight-bearing leg assumes close-packed position. Repeat with the other leg.
Movement during limb protraction, Stand on a box behind the horse (or next to the horse if you suspect he may kick). Palpating the tuber sacrale bilaterally, have an assistant lift one hind leg and stretch it forward. Feel for a slight caudal shift of the contralateral tub sacrale.
PASSIVE TESTING,Stand on a box or step next to the horse. Apply a slow, repetitive downwards force on the tuber coxae. Feel for reflex muscle guarding in response to the movement. A non-painful horse should allow a soft oscillation of the ilium. Compare to the other side Again, bear in mind that movement of the pelvis also causes movement in the lumbar spine and hip, so observe carefully.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 McGowan CM, Stubbs NC, Jull GA. Equine physiotherapy: a comparative view of the science underlying the profession. Equine veterinary journal. 2007 Jan;39(1):90-4.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 Paulekas R, Haussler KK. Principles and practice of therapeutic exercise for horses. Journal of equine veterinary science. 2009 Dec 1;29(12):870-93.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 McGowan C, Goff L, editors. Animal physiotherapy: assessment, treatment and rehabilitation of animals. John Wiley & Sons; 2016 May 2.
- ↑ Johnson C. How to assess the equine mouth when bitting. Equine Health. 2018 Mar 2;2018(40):44-6.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 Tabor G, Williams J. Objective measurement in equine physiotherapy. Comparative Exercise Physiology. 2020 Feb 5;16(1):21-8.
- ↑ 6.0 6.1 McIlwraith, C.W., Anderson, T.A., Douay, P., Goodman, N.L. and Overly, L.R., 2003. Role of conformation in musculoskeletal problems in the racing Thoroughbred and racing quarter horse. In Proceedings of the 49th Annual Convention of the American Association of Equine Practitioners, New Orleans, Louisiana, USA, 21-25 November 2003 (pp. 59-61). American Association of Equine Practitioners (AAEP).
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 Duberstein KJ. Evaluating horse conformation.
- ↑ Genius Equestrian - The Home of Everything Equine [null https://www.geniusequestrian.com/]
- ↑ Garcia EF, Loughin CA, Marino DJ, Sackman J, Umbaugh SE, Fu J, Subedi S, Lesser ML, Akerman M, Schossler JE. Medical infrared imaging and orthostatic analysis to determine lameness in the pelvic limbs of dogs. Open veterinary journal. 2017;7(4):342-8.