Electrocardiogram
Original Editor Uchechukwu Chukwuemeka
Top Contributors - Uchechukwu Chukwuemeka, Kim Jackson, Lucinda hampton, Ayelawa Samuel, Karen Wilson and Rishika Babburu
Introduction[edit | edit source]
An electrocardiogram also termed an ECG or EKG (K means kardia for heart in Greek) or a 12 lead ECG. is a simple test that records the heart's electrical activity[1]. The ECG machine is designed to recognise and record any electrical activity within the heart. It provides information about the function of the intracardiac conducting tissue of the heart and reflects the presence of cardiac disease through its electrical properties. Understanding ECG helps to understand how the heart works. With each heartbeat, an electrical impulse starts from the superior part of the heart to the bottom. The impulse prompts the heart to contract and pump blood.
Some heart problems are easier to diagnose when your heart is working hard and beating fast. During stress testing i.e. exercise ECG, exercise is used to make the heart work hard and beat fast while an EKG is done. If exercise can't be done, you'll be given medicine to make your heart work hard and beat faster[2]. Heart rate and blood pressure will also be monitored throughout the test period. It usually takes about 7 to 12 minutes to complete[2].
What ECG Test is used[edit | edit source]
ECG is used to
- detect bradycardia and tachycardia.
- determine if symptoms, such as chest pain, shortness of breath or palpitations are due to a heart problem[2].
- know steady or irregular heart rhythm.
- know the strength and timing of electrical signals as they pass through each part of your heart.
- detect other disorders that affect heart function.
- Study and detect many heart problems, such as heart attacks, arrhythmia, heart failure.
- asses coronary blood flow and heart valves integrity.
- monitor deeply-sedated patients and for consciously-sedated patients with compromised cardiovascular function.
- monitor some medications for the heart.
- The indications for exercise electrocardiography include to ascertain the correct exercise prescription, the investigation of angina and post-myocardial infarction assessment as well as the postoperative examination of bypass surgery[2].
Electrode and Lead[edit | edit source]
An electrode is a sensor (conductive pad) attached to the skin and enables recording of electrical currents. An ECG lead is a graphical description of the electrical activity of the heart created by reading several electrodes. This means that each ECG lead is gotten by analysing the electrical currents detected by several electrodes[1]. A 12-lead ECG is obtained using 10 electrodes. These 12 leads consists of limb leads and chest leads (percordial leads). For further reading see...
To better under why there are only 10 leads instead of 12 leads read about Einthoven's triangle and the heart's action potential generation.
ECG PAPER[edit | edit source]
The ECG paper is a strip of graph paper with large and small grids with horizontal axis(Time in seconds) and vertical axis(amplitude in volts). Each 1 mm square (the smallest square) represents 0.04 seconds and each large square (5 mm) represents 0.2 seconds. On the vertical axis, each large square represents 0.5 mV and each small block equals 0.1 mV.
Procedures[edit | edit source]
The procedures are to be explained to the patient and what is to be expected during testing will also be clearly communicated to the patient.
Electrode placement[edit | edit source]
Limb Sensor Application
Place the 4 limb sensors on a smooth fleshy area of the lower inner forearm and lower inner legs, or upper inner arms and lower inner thighs, or upper inner arms and lower abdomen[3]. Attach the limb leads.
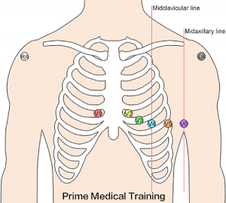
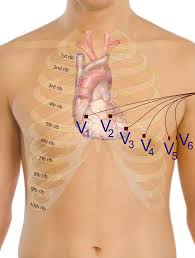
Chest Sensor Application
Place the 6 Chest sensors on the patient’s chest as follows:
V1 Fourth intercostal space at right border of the sternum
V2 Fourth intercostal space at left border of the sternum
V3 Midway between position V2 and position V4
V4 At the mid-clavicular line in the fifth intercostal space
V5 At the anterior axillary line on the same horizontal level as V4
V6 At the mid-axillary line on the same horizontal level as V4 and V5
Attach the chest leads.
To better under why there are only 10 leads instead of 12 leads read about
Stress test (Exercise electrocardiogram)[edit | edit source]
Before exercise commencement, the investigator will perform an EKG at a resting heart and also take blood pressure reading.
Conditions to end the test will be told to the patients and that they should inform the investigator if they feel any of the following:
- Chest or arm discomfort
- Short of breath
- Dizzy
- Lightheaded
- Any other unusual symptoms
At regular intervals, the lab personnel will ask how you are feeling.
It’s normal for your heart rate, blood pressure, breathing rate, and perspiration to increase during the test. The lab personnel will watch for anything on the EKG monitor that suggests the test should be stopped.
The patients starts the exercise at slow pace (e.g. walking on a treadmill or pedaling a stationary bicycle without resistance at a leisure pace). The intensity of the exercise will be gradually increased, until the patient feels exhausted. The patient then reverts back to slow walking pace or pedal slowly for a couple of minutes to cool down. The heart rate, blood pressure, and EKG will continue to be monitored until the levels begin returning to normal.
If medication is used, an IV will be inserted in on the arm in order to have the medication administered.
Electrocardiogram wave[4][edit | edit source]
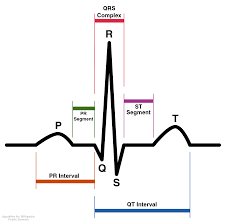
•The first wave (P wave) represents atrial depolarisation (ventricular filling)
•Q wave representing septal depolarisation
•R wave representing ventricular depolarisation
•S wave representing depolarisation of the Purkinje fibres
•QRS is ventricular depolarisation
•T wave is ventricular repolarisation
•ST segment is a flat line any change shows myocardial infarction
• P wave, QRS complex, and T wave show the 3 phase of cardiac cycle in one heart beat.
•after the PQRST complex a U wave, seen electrolyte imbalance(potassium)
Interpretation of ECG waves[5][edit | edit source]
The ECG must always be interpreted systematically because failure to do so, may be detrimental. The step by step sequence of interpreting ECG makes it easy for anyone, as well as reduces the chances of missing important abnormalities and also expedite the process.
1. Rhythm[edit | edit source]
Assess ventricular (RR intervals) and atrial (PP intervals) rate and rhythm by checking:
- ventricular rate (beats/min)
- regular or irregular ventricular rhythm
- atrial rate (beats/min)
- regular or irregular atrial rhythm
- P-waves should precede every QRS complex and the P-wave should be positive in lead II.
Possible findings are
- Sinus rhythm (which is the normal heart rhythm) has the characteristics heart rate of 50–100 beats/minute,P-wave before every QRS complex and positive in lead II and also a constant PR interval.
- Bradycardia: sinus bradycardia is seen in a skipped rhythm, Causes are second and third degree AV block, sinoatrial block and arrest termed sinus node dysfunction (SND) bradycardia and sick sinus syndrome (SSS) if symptomatic.
- Tachycardia (tachyarrhythmia) with narrow QRS complexes (QRS duration <0,12 s): Causes are sinus tachycardia, inappropriate sinus tachycardia, sinoatrial re-entry tachycardia, atrial fibrillation, atrial flutter, atrial tachycardia, and multifocal atrial tachycardia. Tachyarrhythmia with narrow QRS complexes rarely cause circulatory compromise.
- Tachycardia (tachyarrhythmia) with wide QRS complexes (QRS duration ≥0,12 s): The main cause is ventricular tachycardia and it can be life-threatening. QRS complexes become wide due to abnormal ventricular depolarization but 10% of wide complex tachycardia starts from the atria.
2. P-wave morphology and PR interval[edit | edit source]
Assess P- wave morphology and PR interval by checking:
- P-wave is actually positive in leads II, III and aVF.
- All leads P-wave duration is <0,12 seconds
- All leads P-wave amplitude is ≤2,5 mm.
- All leads PR interval must be 0,12–0,22 seconds.
Possible findings are:
- A P-wave that is not positive in lead II is not sinus rhythm.
- First-degree AV block seen when PR interval >0,22 seconds
- Pre-excitation (WPW syndrome) seen when PR interval <0,12 seconds.
- P-wave may be biphasic in V1 (the negative deflection should be <1 mm). It may have a prominent second hump in the inferior limb leads (particularly lead II)
- Longer P-wave duration, amplified second hump in lead II and enhanced negative deflection in V1 depicts P mitrale
- P pulmonale is seen in amplified P-wave in lead II and V1.
- If P-wave not clearly visible, look for inverted P-waves, that is anywhere between the J point and the terminal part of the T-wave.
- Second-degree AV-block Mobitz type I (Wenckebach block) is seen if there is repeated cycles of gradually increasing PR interval until an atrial impulse (P-wave) is blocked in the atrioventricular node and the QRS complex does not appear.
- Second-degree AV-block Mobitz type II is noted if there is intermittently blocked atrial impulses (no QRS seen after P) but with constant PR interval.
- Third-degree AV-block is noted when all atrial impulses (P-waves) are blocked by the atrioventricular node. An escape rhythm arises (cardiac arrest ensues otherwise), which may have narrow or wide QRS complexes, depending on its origin. There is no relation between P-waves and the escape rhythm’s QRS complexes, and atrial rhythm is typically faster than the escape rhythm (both rhythms are typically regular)
3. QRS complex[edit | edit source]
Asses QRS complex by checking:
- QRS duration should normally be between 0,07-0,10 s
- There must be at least one limb lead with R-wave amplitude >5 mm and at least one precordial lead with R-wave amplitude >10 mm; otherwise there is low voltage.
- High voltage exists if the amplitudes are too high, i.e if the following condition is satisfied: S-waveV1 or V2 + R-waveV5 >35 mm.
- Look for pathological Q-waves. Pathological Q-waves are ≥0,03 s and/or amplitude ≥25% of R-wave amplitude in same lead, in at least 2 anatomically contiguous leads.
- If the R-wave progression in the V1–V6 leads normal
- If the electrical axis normal; Electrical axis assessed in limb leads should be between –30° to 90°.
Possible findings are:
- Short QRS duration is of no clinical relevance.
- QRS duration ≥0.12 s depicts left bundle branch block, right bundle branch block, nonspecific intraventricular conduction disturbance, hyperkalemia, use of class I antiarrhythmic drugs, use of Tricyclic antidepressants. Ventricular ventricular extrasystoles (premature complexes), artificial pacemaker use which stimulates in the ventricle, aberrant conduction (abberancy) or Pre-excitation (Wolff-Parkinson-White syndrome).
- High voltage noted in any leads colud be due to cardiac muscle hypertrophy, left bundle branch block (leads V5, V6, I, aVL), right bundle branch block (V1–V3). Normal variant is noted in younger, well-trained and slender individuals.
- Low voltage is noted in cardiac myopathies, previous myocardial artery infarctions resulting reduced cardiac muscle mass, precardial effusion, pleural effusion, pulmonary emphysema
References[edit | edit source]
- ↑ 1.0 1.1 The ECG leads: electrodes, limb leads, chest (precordial) leads, 12-Lead ECG (EKG).https://ecgwaves.com/ekg-ecg-leads-electrodes-systems-limb-chest-precordial/ accessed on 14 Nov, 2018
- ↑ 2.0 2.1 2.2 2.3 Heart disease and stress.https://www.webmd.com/heart-disease/guide/stress-test#2 accessed on 14 Nov, 2018
- ↑ Khan GM. A new electrode placement method for obtaining 12-lead ECGs. Open Heart. 2015; 2(1): e000226. doi: 10.1136/openhrt-2014-000226
- ↑ Kenny WL,Wilmore JH, Costill DL. Physiology of Sport and Exercise, 5th ed. Human Kinetics, 2011. 146-148.
- ↑ Guyton C, Hall E. Test book of medical physiology. Philadelphia:Elsevier Inc. 2006; pg.131-156