Elbow Examination
Original Editor - Jason Brandi and Krista Dayton as part of the Temple University EBP Project
Top Contributors - Jason Brandi, Krista Dayton, Laura Ritchie, Kim Jackson, Nikhil Benhur Abburi, Admin, Rachael Lowe, Kai A. Sigel, Scott A Burns, Anas Mohamed, Tarina van der Stockt, WikiSysop, Wanda van Niekerk, 127.0.0.1, Johnathan Fahrner and Naomi O'ReillyClinical Presentation[edit | edit source]
Pain and symptoms localized in or around elbow. May present with neurological symptoms local or distant to elbow.
Subjective History[edit | edit source]
- Exact location of pain
- Timeline-When are the patients reported symptoms at their worst?
- Mechanism of the injury- In the case of a traumatic event, the mechanism of injury helps guide the diagnosis.[1] For atraumatic injuries, specific symptoms can be highly useful in determining a diagnosis.
For example: patient reported numbness and/or tingling in the 5th digit may suggest ulnar neuropathy.[1] - Presence of numbness or tingling?
- Medications?
- Past Medical History
- Diagnostic Testing/Imaging?
Region Specific Historical Question[edit | edit source]
These questions will help guide the examination. For example[2]:
- Do your symptoms change (better or worse) with any movements of the neck or shoulder?
- Does your elbow ever “slip out” or feel unstable?
- Does the pain change with gripping activities?
- Do you ever experience numbness of tingling in the hand?
- Was the elbow hyper extended during the time of injury?
- Do you relate the symptoms to a throwing activity?
Environmental and Personal Factors[edit | edit source]
During the initial examination, environmental and personal factors should be addressed. These issues could affect healing and return of function after an elbow injury. Table 1 outlines these issues.[1]
| Table 1. Patient Factors that can affect healing and return of function after elbow injury |
| Diabetes * Immunosuppression * Infection * Multiple site injuries * Tobacco use * Excessive alcohol intake * Complications following injury or surgery(joint stiffness, heterotopic ossification, infection, joint instability) |
Self-Report Outcome Measures[edit | edit source]
- DASH (Quick Dash)
- Patient-Specific Functional Scale
- PREE and ASES: Patient-rated elbow evaluation (PREE)[1] and American Shoulder and Elbow Society evaluation(ASES)[3] are two similar scales that allow the patient to self-report their pain and disability related to their elbow pathology. The conceptual difference between the two scales is minimal and the correlation between the two scales usually exceeds 0.90.[1]
- P4: P4 is a 4-item pain intensity measure. The P4 asks patients to rate pain in the morning, afternoon, evening, and with activity over the past 2 days. The P4 can be particularly useful as the elbow is greatly impacted by movement and time of day.[1]
- SF-36: SF-36 is a generic health form. It is appropriate to address broad areas of health. For individuals with elbow dysfunction, the SF-36 is not a good tool to evaluate change in the clinic for patients with elbow disorders because it is not responsive and specific to the symptoms that the patient is reporting with. This measure can also be very time consuming and difficult to use.[1]
Special Questions[edit | edit source]
- Red and Yellow Flags- Conditions that may require referral to appropriate health care provider.
| Red Flags |
|
| Yellow Flags |
|
Investigations[edit | edit source]
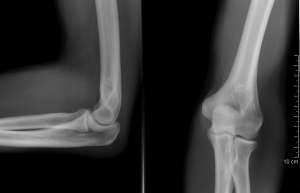
- Radiological Considerations
- The information from the history should be correlated with imaging findings of the elbow when available.[1]
Objective[edit | edit source]
Observation[edit | edit source]
- General posture of the upper quarter: Proximal factors should be considered which could predispose the patient to elbow symptoms.
- Thoracic and cervical spine including kyphosis and forward head
- Scapula
- Carrying angle: The carrying angle has a mean value of 10 degrees for men and 13 degrees for women.[4] variability occurs till age of 14 -15
- Swelling/ecchymosis/deformities/muscle wasting
- Triangle Sign
Functional Tests[edit | edit source]
The goal in performing functional test is to obtain and quantify an asterisk sign to assess and reassess after intervention is performed.
- Determination of an asterisk sign-(What activity increases symptoms?)
- Pain-Free Grip Strength
- Push-off Test: The push off test can be used to quantify a person’s ability to bear weight through the upper extremity. This can help identify functional/occupational limitations. (ICC=0.31-0.97).[1]
- Functional Impairment Test-Hand, Neck, Shoulder Arm (FIT-HaNSA): Standardized physical test. Assesses gross activities of the upper extremity. Validation in elbow conditions has not yet been completed. [1]
Palpation[edit | edit source]
- Medial/lateral epicondyle
- Olecranon and olecranon fossa
- Radial head
- Ulnar Collateral Ligament (UCL) of the elbow
- Soft tissue in upper arm and forearm/wrist for pain provocation, heat, swelling
Image 2: Anterior Elbow[4] Image 3: Lateral Elbow[4] Image 4: Medial Epicondyle[4]
Bicep tendon Marked Circle represents lateral epicondyle Dot represents medial epicondyle
Neurologic Assessment[edit | edit source]
- Reflexes: C5-C7
- Myotomes: C5-T1
- Dermatomes: C5-T1
Movement Testing[edit | edit source]
- Active Range Of Motion(AROM)/Passive Range Of Motion(PROM) with or without overpressure
- Elbow
Flexion
Extension
- Positive Elbow Extension Test may indicate fracture and referral.
Forearm pronation/supination - Wrist
Flexion
Extension - Cervical, Shoulder and Elbow Range of Motion with or without overpressure
Posterior-anterior glide assessment on cervical/thoracic spine for distal symptoms reproduction as well.
- Elbow
- Resistive Testing
- Elbow flexion/extension
- Forearm pronation/supination
- Wrist flexion/extension
- Pain-free grip strength
- Thumb
- Fingers
- Accessory motion testing
- Humeroulnar traction
- Humeroradial traction
- Proximal/distal radioulnar Anterior/Posterior and Posterior/Anterior glides
Special Tests[edit | edit source]
- Elbow Flexion Test
- Tinel's Sign
- Ulnar Nerve Compression Test
- Passive elbow extension, pronation, wrist flexion (Mill's Test)
- Resisted wrist extension with radial deviation (Cozen's Test)
- Resisted middle finger extension (Maudley's Test)
Ligamentous Tests:
- Median nerve bias: Upper Limb Neurodynamic Test 1
- Radial nerve bias: Upper Limb Neurodynamic Test 2b
- Ulnar nerve bias: Upper Limb Neurodynamic Test 3
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 MacDermid JC, Michlovitz SL. Examination of the elbow: linking diagnosis, prognosis, and outcomes as a framework for maximizing therapy interventions. J Hand Ther. 2006; 19(2):82-97.
- ↑ Flynn TW, Cleland JA, Whitman JM. User’s Guide to the Musculoskeletal Examination: Fundamentals for the Evidence Based Clinician. Evidence in Motion, 2008.
- ↑ King GJ, Richards RR, Zuckerman JD, et al. A standardized method for assessment of elbow function. Research Commitee, American Shoulder and Elbow Surgeons. J Shoulder Elbow Surg. 1999; 8:351–4.
- ↑ 4.0 4.1 4.2 4.3 Colman WW, Strauch RJ. Physical examination of the elbow. Orthop Clin North Am. 1999; 30(1):15-20.
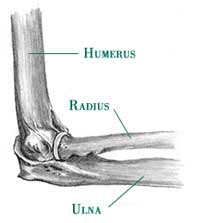
![Illustration adapted from [Colman WW & Strauch RJ].](/images/3/35/Anterior_elbow.jpg)