Parkinson's Pharmacotherapy
Introduction[edit | edit source]
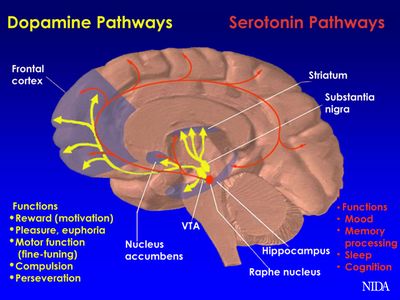
Parkinson’s is a progressive neurodegenerative disorder that affects motor function. This disease has become an epidemic, affecting approximately 1 percent of individuals over the age of 65 years old [1]. It is caused by decreased dopamine production in the basal ganglia due to degeneration of dopamine-secreting neurons [2],[3].
Initially, people with Parkinson's may be asymptomatic with the first clinical symptoms appearing after 60% of the dopaminergic neurons have degenerated in the substantia nigra [4]. Cardinal symptoms of Parkinson disease include bradykinesia, akinesia, rigidity, and resting tremors [2],[5]. The exact cause of Parkinson's is unknown; however, contributing factors to may include trauma, infection, cortical degeneration, antipsychotic drugs and cerebrovascular disease [6][7][8][9]. If Parkinson's goes untreated, total incapacitation will occur due to uncontrolled motor problems. This is why it is extremely important for Parkinson's patients to be prescribed the proper drug regimen. The video below outlines briefly medication rational and major drug types
The inter-dependency of healthcare professionals is significant in the management of Parkinson's. Specialists are encouraged to have the knowledge and understanding of the condition and its impact on the quality of life. Communication is a key and it should aim to empower individuals who suffer Parkinson's to develop effective self-management strategies with an optimistic and realistic approach.
Understanding the impact of medication on both the movement and thought quality of people with Parkinson’s will help set goals and plans for physiotherapy intervention. Individual Parkinson’s Associations provide country-specific information about medications prescribed. E.g. In the UK, where physiotherapists can train to prescribe medication, a good summary of drug therapies can be found on the Parkinson’s UK site and in the US, the National Parkinson’s Foundation provides advice.
Parkinson's medications are most commonly administrated orally. Injections and subcutaneous medications are available but expensive.
Medication help in controlling motor and non-motor symptoms, however, fluctuations in the responsiveness are experienced as the condition is progressed. Wearing off and motor fluctuations occur as the body develops dependency and the threshold to medications is altered. Refer to the EPDA website to learn more on wearing off.
Deep brain stimulation, stem cell therapy and gene therapy are alternative approaches that aim to lower the need to medications.
The main types of drugs that are used to treat Parkinson’s are[11]:[edit | edit source]
- Levodopa
- Dopamine agonists
- Glutamate antagonist
- Anticholinergics
- COMT inhibitors
- MAO-B inhibitors
- Dopaminergic Medications
Levodopa[edit | edit source]
Levodopa (L-dopa) is a common drug administered during the progressive stages of PD. L-dopa is considered a prodrug, meaning it is not activated until after it crosses the blood brain barrier via active transport[12]. The primary use of Levodopa is to restore depleted levels of dopamine at the presynaptic terminal of the substantia nigra, which restores functional movement[13]. This replacement can relieve symptoms of PD, such as freezing and rigidity[14]. If a tolerance is built up to L-dopa, or adverse motor effects become present with this drug alone, partner drugs Benserazide and Carbidopa (LD-CD) can be supplemented to prevent the further premature breakdown in the periphery[15].
Optimal oral dosing of LD-CD is typically between 97.5 mg-390 mg for a single dose, and 25mg-100mg bi-daily/tri-daily for either sustained release or immediate release[16]. The volume of distribution is typically around 28.5 L and the plasma half-life clearance is 1.8 hours. Therefore, frequent dosage is required. The renal clearance of L-dopa is approximately 72 ml/min[13].
Many of the adverse effects that are present with Levodopa are due to the fact that it is not combined with a partner drug. Some of the most common adverse effects to be aware of during a physical therapy visit include gastrointestinal distress due to the enteral administration, cardiac difficulties, gait disturbances due to dyskinesias, end of dose akinesia, and a tolerance after around 3-4 years. Administering physical therapy treatment during the peak time of this drug helps to avoid these end of dose side effects[14].
MAO-B Inhibitors[edit | edit source]
Monoamine Oxidase B Inhibitors, such as Selegiline and Rasagiline, are commonly used by patients with Parkinson's because of their potential disease modifying and neuroprotective effects [17]. This drug class is considered a potential disease modifier due to its ability to inhibit the monoamine oxidase type B (MAO-B) enzyme, which naturally breaks down dopamine in the brain[17].By inhibiting the breakdown of the MAO-B enzyme, these drugs are able to extend the effects of dopamine at the CNS synapse [18][19]. However, more research needs to be done on the ability of MAO-B inhibitors to slow the progression of PD. MAO-B inhibitors exhibit neuroprotection by decreasing dopamine oxidation, therefore preventing excessive production of free radicals, while prolonging the effects of endogenous dopamine[20][21] MAO-B inhibitors can be used as an initial drug in the treatment of Parkinson’s Disease or can be combined with Levodopa in order to reduce motor fluctuations[17].
The prototypical selective, irreversible MAO-B inhibitor, Selegiline, is absorbed in the GI tract and then distributed to tissues throughout the body, including the brain[22]. Selegiline is metabolized to L-amphetamine-like metabolites which may promote insomnia [17]. This drug is primarily metabolized in the liver and then excreted by the kidneys [22]. Selegiline has an oral bioavailability of 10% and an oral clearance rate of 59 L/min [23]. This drug is given at a therapeutic dose of 10mg/day and has a half-life of 10 hours[17]. Selegiline is typically administered twice per day as a 5mg oral tablet [24]. If this dose is increased Selegiline will lose it’s selective ability[17].
Rasagiline, another selective, irreversible MAO-B inhibitor, is metabolized into aminoindan in the liver by cytochrome p450 type 1A2, which means it does not have the amphetamine-like effects that Selegiline displays and may be preferred[25]. Its oral bioavailability is 35% and it reaches its therapeutic maximum after 0.5-1 hour [25]. The oral clearance rate of Rasagiline is 94.3 L/day[25]. This drug is given at a recommended dose of 0.5-1 mg/day and has a half-life or 1.5-3.5 hours [25]. It is typically administered once per day as a 0.5mg or 1mg oral tablet [24].
When used in adjunct with Levodopa both Selegiline and Rasagiline have been known to decrease motor fluctuations in patients with Parkinson's [17]. These two drugs are relatively safe compared to other MAO inhibitors due to their selective ability[26]. Common adverse effects of other MAO-B Inhibitors may include dizziness, headache, GI distress, and sedation[26].
Dopamine Agonist Medications[edit | edit source]
Dopamine agonists are another commonly used class of drugs implemented during the treatment of PD[27][28]. Dopamine agonists work by actively influencing dopamine receptors in the brain to produce more in-vivo dopamine, thus making it the preferential treatment early on in the disease process. Apomorphine is considered the premier drug in this category, due to its powerful motor fluctuation modulating capabilities, such as those seen in end of dose dyskinesias generated by some anti-parkinsonian medications (i.e. LD)[29]. Apomorphine is typically administered subcutaneously on a continuous cycle for an average of 16 hours per day at a rate of 3-6 mg/hr[30]. Further pharmacokinetics of apomorphine, include the drug taking approximately 15-20 minutes to reach its maximum bioavailability within the bloodstream[31][32]. Once in the blood, the drug takes about 30-40 minutes to reach its half life[30][31][32]. This is fairly quick and the reason for the drug being given on a constant basis throughout the day[30]. Apomorphine’s clearance in the system is close to 3-4 L/h/kg, meaning that it leaves the plasma at a rapid rate[33]. After the drug has been metabolized, it is then excreted through urine by the kidneys[30].
The main adverse effects seen after the intake of this medication include somnolence, withdrawal, and psychiatric disorders, such as confusion and hallucinations[29][30]. It is vital that the physical therapist is aware of such side effects to dictate the treatment.
Anticholinergic Medications[edit | edit source]
Anticholinergic drugs, including Benztropine mesylate, Biperiden, Diphenhydramine, and Trihexyphenidyl, are another important class of medications used to mitigate the motor symptoms of Parkinson’s disease. By using these drugs in the early progression of the disease, the need for Levodopa can be prolonged. While the exact mechanism of action is unknown, it is said that anticholinergic drugs are competitive antagonists of muscarinic receptors; thus, inhibiting disproportionate acetylcholine action from the basal ganglia, specifically involuntary muscle movement. These drugs are taken orally and range from 30-70% bioavailable. After taken, they are rapidly absorbed (with the exception of benztropine mesylate) into the brain and produce a high volume of distribution, then biotransforming via N-dealkylated and hydroxylated metabolites. The drug clearance appears to be low in comparison to hepatic blood flow, which reduces the chances of first pass effect. Excretion of the parent drug and metabolite are through the kidneys. With these things being said, there is very little information on the pharmacokinetic information for anticholinergic drugs.
As for dosage, the suggested amount of this class of drugs is between 6-20 mg daily; however, there is a specific anticholinergic phenothiazine compound that is to be taken from 50-600 mg daily. The half life of anticholinergic drugs is between 4 hours to 24 hours, with Diphenhydramine being on the shorter range and Biperiden being on the higher range.
Each medication has its own particular side effects; however common adverse effects of anticholinergic drugs include memory problems, drowsiness, constipation, sedation, urinary retention, blurred vision, tachycardia, and delirium. Increased side effects are typically seen in the elderly, when compared with younger adults. As a physical therapist, these are all things to consider, especially when treating your elderly patients. Future studies must be performed to get a better understanding of why elderly patients tolerate this drug less[34].
References[edit | edit source]
- ↑ Harris PE ,C. K. Prevalence of complementary and alternative medicine (CAM) used by the general population: a systematic review and update. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/22994327. October, 2012. Accessed November 5, 2018.
- ↑ 2.0 2.1 Chen JJ, Nelson MV, Swope DM. Parkinson’s disease. DiPiro JT, Et al, eds. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York: Mcgraw-Hill. 2011.
- ↑ Parent M, Parent A. Substantia nigra and Parkinson's: a brief history of their long and intimate relationship. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/20481265. May, 2010. Accessed November 5, 2018.
- ↑ Lecht, S., Haroutiunian, S., Hoffman, A., & Lazarovici, P. Rasagiline – A Novel MAO B Inhibitor in Parkinson’s Disease Therapy. NCBI. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2386362/. June, 2007. Accessed November 5, 2018.
- ↑ Garcia Ruiz PJ, Catalan MJ, Fernandez Carril JM. Initial motor symptoms of Parkinson disease. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/22045320. November 17, 2011. Accessed November 5, 2018.
- ↑ Gelabert-Gonzalez M, Serramito-Garcia R, Aran-Echabe E. Parkinsonism secondary to subdural haematoma. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/22527627. July, 2012. Accessed November 5, 2018.
- ↑ Gupta D Kuruvilla. Vascular parkinsonism: what makes it different? NCBI. https://www.ncbi.nlm.nih.gov/pubmed/22121251. December, 2011. Accessed November 5, 2018.
- ↑ Lopez-Sedon JL, Mena MA, de Yebenes JG. Drug-induced parkinsonism in the elderly: incidence, management and prevention. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/22250585. February, 2012. Accessed November 5, 2018.
- ↑ Mazokopakis EE, Koutras A, Starakis I, Panos G. Pathogens and chronic or long-term neurologic disorders. NCBI. https://www.ncbi.nlm.nih.gov/pubmed/21446901. March, 2011. Accessed November 5, 2018.
- ↑ PD care New York Taking Control: Medications for Parkinson's Available from: https://www.youtube.com/watch?v=T8VojsSvv4E (last accessed 8.11.2019)
- ↑ Parkinsons Victoria Medications Available from: https://www.parkinsonsvic.org.au/parkinsons-and-you/medications/ (last accessed 7.11.2019)
- ↑ Standaert DG, Roberson ED. Chapter 22: Treatment of Central Nervous System Degenerative Disorders. In: Goodman & Gilman's: The Pharmacological Basis of Therapeutics. Vol 1. 12th ed. New York, NY: The McGraw-Hill Companies, Inc. ; 2011.1.
- ↑ 13.0 13.1 Lewitt MD, PA. Levodopa therapy for Parkinsons disease: Pharmacokinetics and pharmacodynamics. Movement Disorders. 2014;30(1):65-67. doi:10.1002/mds.26082.
- ↑ 14.0 14.1 Connolly MD, BS, Lang MD, AE. Pharmacological Treatment of Parkinson Disease. Jama. 2014;311(16):1670. doi:10.1001/jama.2014.3654.
- ↑ del Amo EM, Urtti A, Yliperttula M. Pharmacokinetic role of L-type amino acid transporters LAT1 and LAT2. European Journal of Pharmaceutical Sciences. 2008;35(3):161-174. doi:10.1016/j.ejps.2008.06.015
- ↑ Hsu A, Yao HM, Gupta S, Modi NB. Comparison of the pharmacokinetics of an oral extended‐release capsule formulation of carbidopa‐levodopa (IPX066) with immediate‐release carbidopa‐levodopa (Sinemet®), sustained‐release carbidopa‐levodopa (Sinemet® CR), and carbidopa‐levodopa‐entacapone (Stalevo®). The Journal of Clinical Pharmacology. 2015 Sep 1;55(9):995-1003.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Teo KC, Ho SL. Monoamine oxidase-B (MAO-B) inhibitors: implications for disease-modification in Parkinson’s disease. Translational neurodegeneration 2013 Dec;2(1):19.
- ↑ Fabbrini G, Abbruzzese G, Marconi S, Zappia M. Selegiline: a reappraisal of its role in Parkinson disease. Clinical neuropharmacology 2012 May 1;35(3):134-40.
- ↑ Magyar K. The pharmacology of selegiline. In: International review of neurobiology. Academic Press, 2011 (Vol. 100, pp. 65-84).
- ↑ Weinreb O, Amit T, Bar-Am O, Youdim MB. Rasagiline: a novel anti-Parkinsonian monoamine oxidase-B inhibitor with neuroprotective activity. Progress in neurobiology 2010;92(3):330-44.
- ↑ Aluf Y, Vaya J, Khatib S, Loboda Y, Finberg JP. Selective inhibition of monoamine oxidase A or B reduces striatal oxidative stress in rats with partial depletion of the nigro-striatal dopaminergic pathway. Neuropharmacology 2013;65:48-57.
- ↑ 22.0 22.1 Heinonen EH, Myllylä V, Sotaniemi K, Lamintausta R, Salonen JS, Anttila M, Savijärvi M, Kotila M, Rinne UK. Pharmacokinetics and metabolism of selegiline. Acta neurologica Scandinavica. Supplementum 1989;126:93-9.
- ↑ Mahmood I. Clinical pharmacokinetics and pharmacodynamics of selegiline. Clinical pharmacokinetics 1997;33(2):91-102.
- ↑ 24.0 24.1 UCSF School of Medicine. Parkinson's Clinic and Research Center. Available from: http://pdcenter.neurology.ucsf.edu/patients-guide/parkinson’s-disease-medications/monoamine-oxidase-b-mao-b-inhibitors(accessed 5 November 2018).
- ↑ 25.0 25.1 25.2 25.3 Lecht S, Haroutiunian S, Hoffman A, Lazarovici P. Rasagiline–a novel MAO B inhibitor in Parkinson’s disease therapy. Therapeutics and clinical risk management 2007;3(3):467.
- ↑ 26.0 26.1 Chen JJ, Wilkinson JR. The monoamine oxidase type B inhibitor rasagiline in the treatment of Parkinson disease: is tyramine a challenge? The Journal of Clinical Pharmacology 2012 May;52(5):620-8.
- ↑ Bonuccelli U, D. D. Role of dopamine receptor agonist in the treatment of early Parkinson's. Parkinsonism Related Disorders, 2009;(4): S44-53.doi: 10.1016/S1353-8020(09)70835-1.
- ↑ Harris PE ,C. K. Prevalence of complementary and alternative medicine (CAM) used by the general population: a systematic review and update. Int J Clin Pract, 2012; 66(10): 924-939. doi: 10.1111/j.1742-1241.2012.02945.x.
- ↑ 29.0 29.1 Regina Katzenschlager MD, W. P. Apomorphine subcutaneous infusion in patients with Parkinson's with persistent motor fluctuations (TOLEDO): a multicentre, double-blind, randomised, placebo-controlled trial. The Lancet Neurology, 2018;(9):749-759. doi: 10.1016/S1474-4422(18)30239-
- ↑ 30.0 30.1 30.2 30.3 30.4 Auffret M, D. S. (2018) Pharmacological Insights into the Use of Apomorphine in Parkinson's: Clinical Relevance. Clinical Drug Investigation, 2018; 38(4) 287-312. doi: 10.1007/s40261-018-0619-3.
- ↑ 31.0 31.1 Nomoto M, Kubo SI, Nagai M, Yamada T, Tamaoka A, Tsuboi Y, Hattori N, Parkinson's Study Group. A randomized controlled trial of subcutaneous apomorphine for Parkinson disease: a repeat dose and pharmacokinetic study. Clinical neuropharmacology. 2015 Nov 1;38(6):241-7.
- ↑ 32.0 32.1 Elisa Unti, R. C. Apomorphine hydrochloride for the treatment of Parkinson's . Expert Review of Neurotherapeutics, 2015; 15(7): 723-732. doi: 10.1586/14737175.2015.1051468.
- ↑ rgiolas A, H. H. (2001). The pharmacology and clinical pharmacokinetics of apomorphine. BJU international, 2001; 88(3): 18-21. https://doi.org/10.1046/j.1464-4096.2001.00124.x
- ↑ Brocks, D. R. Anticholinergic drugs used in Parkinson's: An overlooked class of drugs from a pharmacokinetic perspective. J Pharmaceut Sci.https://sites.ualberta.ca/~csps/JPPS2(2)/D.Brocks2/anticholinergic.htm. August 22, 1999. Accessed November 5, 2018