Diagnostic Approaches to Low Back Pain - Comparing Maitland, McKenzie and Movement Impairment Syndromes
Original Editor - Kathryn Priest, Katherine Portas, Lea Cobham and Anj Leung as part of the Nottingham University Spinal Rehabilitation Project
Top Contributors - Kathryn Priest, Katherine Portas, Angela Hiu-Wai Leung, Kim Jackson, Lea Cobham, Lucinda hampton, Admin, 127.0.0.1, Evan Thomas and Candace Goh
Introduction [edit | edit source]
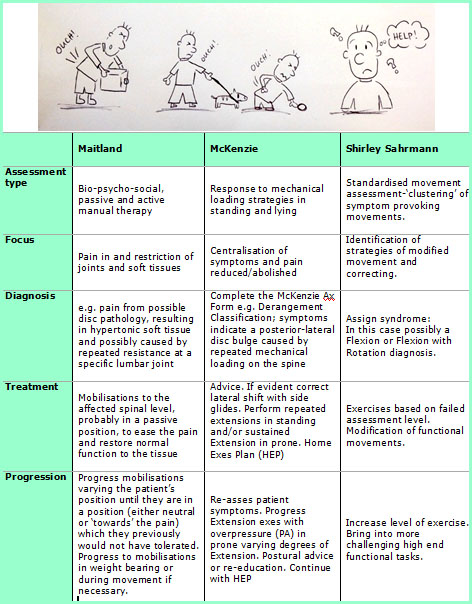
Physiotherapists use a range of techniques to assess and diagnose low back pain. The most commonly used in the UK are those of Geoffrey Maitland (mobilisations), Robin McKenzie (derangement, dysfunction) and Shirley Sahrmann (movement impairment). (For extensive details on each approach, please see the links above for the relevant Physiopedia pages. A short summary will be provided for each below).
Determining which approach is best to use, in what circumstances and with which patients, can be confusing, especially for students and newly qualified clinicians. Furthermore, clinicians rarely use just one approach, and can often use these in combination with other modalities such as acupuncture, massage[1] or electrotherapy[2].
Maitland's Mobilisations[edit | edit source]
Geoffrey Maitland first described his concept of mobilisations and manipulations in 1965[3]. It is a passive mechanical approach that aims to move synovial joints ("passive arthro-kinematic motion"; literally 'joint-moving')[4] and their surrounding tissues.
This can be applied both to the spine and to the extremities, with the goal of reducing pain and stiffness and restoring correct alignment and function.
There is no specific patient group that this is suitable for, although contraindications are shown to the right of this page. The nature of these contraindications shows that the Maitland techniques are a relatively conservative treatment for patients without severe or acute joint pathology.
Contraindications to Maitland's Mobilisations[5][edit | edit source]
- Malignancy
- Pregnancy
- Vertebral artery insufficiency
- Active ankylosing spondylitis
- Rheumatoid arthritis
- Spondylolisthesis
- Gross foraminal encroachment
- Acute nerve root irritation or compression
- Instability of the spine
- Recent whiplash
Key Principles of Maitland's Approach Include[edit | edit source]
- Mobilisations should be focused on the specific spinal segment(s) that are painful or restricted in their movement during diagnosis[6]
- Regular re-assessment (to check and re-check that the current diagnosis is correct and that the treatment is having a positive effect)[7]
- A consideration at all times of the bio-psycho-social presentation of the patient, and how this affects treatment[7]
Grading Maitland Mobilisations[edit | edit source]
A mobilisation is a controlled oscillatory repeated movement of the joint (REF). Mobilisations are described in five grades, varying in amplitude of movement and force against resistance.
Grade I - Small amplitude movements at the beginning of the range of movement, against no resistance (pain gating effect[8])
Grade II - Large amplitude movements, through range up to a feeling of resistance (also pain-gating effect)
Grade III - Large amplitude movements, shallowly into resistance but not to the full feeling of restricted movement
Grade IV - Small amplitude movements, deep into resistance to begin to increase the range of motion of the joint
Grade V - High velocity, low amplitude thrust to a joint, beginning at the endpoint of resistance of the joint with decreased range (commonly called a 'manipulation' as opposed to a 'mobilisation').
Although these grades appear quite specific, Maitland himself wrote, as recently as 2005, that adaptions to technique will always need to be made as every patient is different and presents with different symptoms[9].
Evidence for the Effectiveness of Maitland's Mobilisations[edit | edit source]
- Chiradejnant et al (2003) found that although lumbar spine Maitland mobilisations did have an immediate pain-relieving effect, the specific mobilisation performed was not important. Pain-relieving effects tended to be greater if the mobilisation was performed at lower lumbar levels rather than higher[11]
- In a small trial comparing grade II and grade III mobilisations in 30 patients with sub-acute to chronic lumbar spine pain, Seema (2012) found that both techniques had a significant positive effect (p=0.001) on pain scores. Grade III mobilisations had a greater effect than grade II. [12]
Moderate evidence exists for the benefits of Maitland's mobilisations in combination with other approaches. However, this is often focussed on other parts of the body rather than the spine, such as the shoulder. In a systematic review of the effectiveness of manual therapy to the shoulder, Caraminos and Marinko (2009) found that end-range / high-grade mobilisations had greater significant positive outcomes compared to mid-range mobilisations. However, the review also showed that mobilisations-with-movement had a similar, though not as significant, beneficial effect[13]. This literature is of course not specific to the spine, but may be taken to inform the use of mobilisations while the literature remains heterogeneous on the subject.
Evidence for Effectiveness Compared to Other Techniques[edit | edit source]
- Naik et al (2007) suggested that Maitland's mobilisations are more effective at improving range of movement than Mobilisations With Movement (MWMs - Mulligan approach), although MWMs are more effective if pain is the most prominent factor for the patient. They also noted that the group receiving Maitland mobilisations required more sessions before being discharged than the MWM group[14]. However it is worth noting that this was a study on mobilisations after a Colles (distal radius) fracture.
- In a systematic review of randomised controlled trials in five languages, Bronfort et al (2004) found that one treatment of spinal manipulation therapy (SMT) was superior to one treatment of spinal mobilisations for acute low back pain. There was also moderate quality evidence that SMT:
- Is superior to detuned diathermy 1 week after treatment
- Resulted in faster recovery than patients receiving a combination of diathermy, exercise and ergonomic instruction.
- Resulted in a faster recovery time than heat therapy for patients with LBP accompanied by sciatica [15]
- A comparison of Maitland mobilisations versus McKenzie -style press ups in 30 patients with non-specific low back pain found that both methods significantly reduced the patient-reported pain rating. However, neither treatment was found to be superior to the other [6].
Other Points to Consider: Clinical Expertise and Practical Application[edit | edit source]
Interview with Heather Reid, Physiotherapy Lecturer at The University of Nottingham
The McKenzie Approach [edit | edit source]
Using McKenzie Mechanical Diagnosis and Therapy (MDT) the patient can be classified into one of three mechanical syndromes; Derangement, Dysfunction or Postural Syndrome. If the patient has no symptom improvement after several sessions they will be classified into "Other" [16].
In Clinical Guidelines and Systematic Reviews the McKenzie method has frequently been defined as an intervention (often in the form of extension exercises) without a preceding MDT assessment[16].
An MDT assessment enables the clinician to clinically reason the most appropriate management to pursue for the specific classification[17]. Find an example of an assessment form here
The McKenzie approach is a combination of active therapy and education for patients with acute, sub-acute and chronic non-specific low back pain [18].
McKenzie Classifications[edit | edit source]
| Derangement Syndrome | Dysfunction Syndrome | Postural Syndrome |
|
|
|
For an in-depth description of these syndromes please follow this link:
Evidence Regarding the Effectiveness of the McKenzie Approach [edit | edit source]
- Many pain measures showed that the McKenzie method is a successful treatment to decrease chronic low back pain in the short term, while the disability measures determined that the McKenzie method is better in enhancing function in the long term[19]
- When a lumbar assessment is performed by a clinician with McKenzie training there is high reliability of classifications (Kappa =0.89)[20].
- Evidence highlights short-term improvements in pain and disability using the McKenzie method however; more research is needed into the long-term benefits[21].
- Directional preference exercises encourage active management and elicit patient empowerment. In health care practice it is perceived as a cost effective intervention[16].
- MDT primarily treats the mechanical dysfunction, with the intention that the improvement of symptoms may positively affect the psychological presentation of the patient [17].
Evidence for Effectiveness Compared to Other Techniques[edit | edit source]
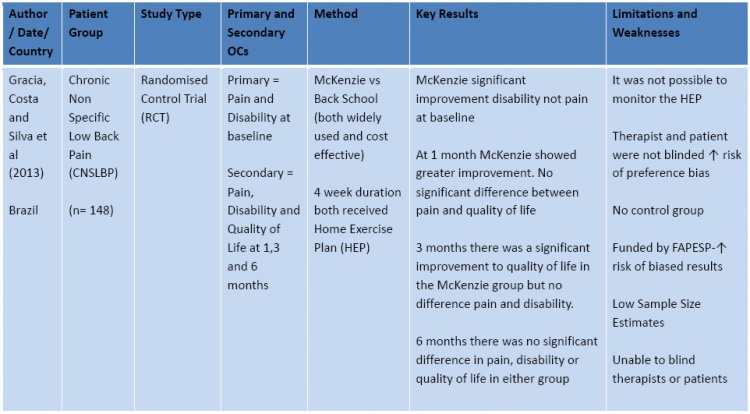
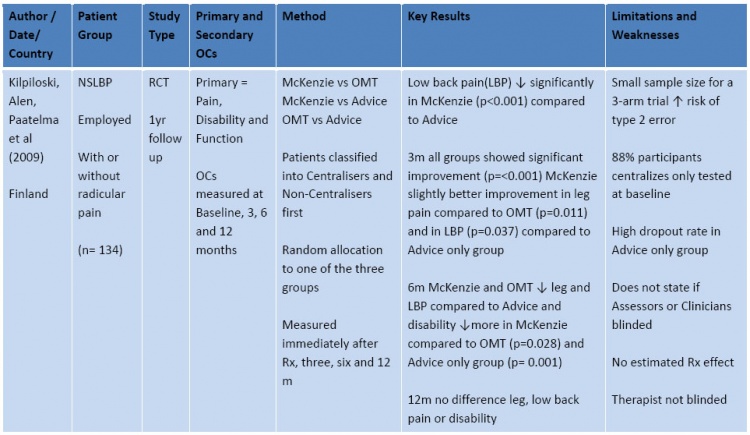
The tables below summarise the evidence since 2009. This summary is not exhaustive, but follows the principles of critical assessment for randomised controlled trials as defined at www.bestbets.org .
To conduct your own search, try http://www.ncbi.nlm.nih.gov/pubmed or www.thecochranelibrary.com .
ABBREVIATIONS for Tables:
CNSLBP = Chronic Non-Specific Low Back Pain
RCT = Randomised Control Trial
Rx = Treatment
n= number of participants
Other points to Consider: Clinical Expertise and Practical Application[edit | edit source]
Interview with Jackie Hollowell, Physiotherapy Lecturer at The University of Nottingham:
Movement Impairment Syndromes[edit | edit source]
For a more detailed description of this approach and treatment structure visit this link .
Like McKenzie, Sahrmann’s Movement Impairment Syndromes (MIS) approach to diagnosis of LBP is one of a number of movement based classification systems designed to help therapists categorise patients and inform treatment [22] .
The theory behind the approach revolves around the human ‘Movement System’ and impairments within this system. Impairments are caused by decline in the quality and precision of joint movements in the spine, as a result of repeated habitual movements or prolonged postures. This may result in:
- Muscle length/strength imbalances
- Altered patterns of motor recruitment patterns and timing
- De-recruitment
- Stiffness
[17][23]
These adaptations can cause altered movements resulting in microtrama to tissue that can accumulate to form macro trauma over time. This is because the human movement system works on the principle of the ‘Path of least resistance’. Stiffness in a muscle or joint will result in a compensatory movement elsewhere resulting in a movement strategy that is not mechanically advantageous and can result in pain.
Assessment[edit | edit source]
The role of the physiotherapist is to systematically identify these detrimental adaptations by assessing the Movement System.
A copy of a standard assessment can be accessed here.
The tests contained in the assessment focus on the influence of hip and pelvic movements on the lumbar spine in weight bearing and non-weight bearing positions[17]. These tests are more sensitive than specific and guide the therapist search to identify the cause of their patients pain. During each test the therapist should assess:
• Quality of movement
• Alignment
• Stiffness
• Muscular recruitment pattern/timing
Classification[edit | edit source]
Each of the tests within the assessment bias one or more movements. By bringing together the results of each test a movement impairment syndrome can be identified. The syndromes are named after the provocative movements:
In order of frequency of diagnosis[24]:
- Extension-rotation
- Extension
- Rotation
- Flexion-Rotation
- Flexion
Unlike a more medical/patho-anatomical approach the therapist is not seeking to identify a specific structure to rehabilitate, rather the direction of impairment within the movement system is identified.
'Birth to death Practitioners' Concept[edit | edit source]
Sahrmann has expressed the importance of emphasising the existence of the ‘Movement System’ to both physiotherapist and those outside the profession. She sees the therapist as being responsible for this system throughout a person’s life span; guiding it during its development, maintaining it through adult years and slowing degeneration towards end of life. She has called for a paradigm shift in thinking that sees therapists assessing many people infrequently for ‘check ups’ much like the business model of the dentist[25].
Evidence Regarding the Effectiveness of the Movement Diagnosis Approach[edit | edit source]
- Intertester reliability for diagnosis using the MIS approach had ‘substantial’ agreement (Kappa >60%). But this was dependant on the diagnostic subgroup and training level of testers. The Flexion and Rotation with Flexion diagnosis the most reliably diagnosed[17].
- No clear advantage has been found for having a specific patho-anatomical diagnosis for LBP over a movement based approach, or vice versa. Although Sahrmann acknowledges that a ‘modified approach’ if needed when a patient has a specific medical diagnosis such a stenosis, but how this is to be operationalized is less well defined[17].
- MIS has established itself as an effective diagnostic tool for sub classifying LBP, however there is a sparse amount of literature showing the effectiveness treatment within this approach[26] [27]. There have been a few case studies reporting reduction of symptoms [28] [24] and many physiotherapists utilising this approach with their patients have seen positive results anecdotally.
Limitations[edit | edit source]
- There is little reference to bio-psycho-social factors within the MIS approach, although fear avoidance can be measured, but it is not clear how differently a patient with high fear avoidance would be managed[17]. Sahrmann and Van Dillen acknowledge that the bio-psycho-social subtype have not featured strongly in their research[17].
- No acknowledgement of central sensitisation within LBP was found in the MIS approach[17] and Sahrmann has eluded to the overuse of this term by therapists as a way of explaining why their patients are not getting better[29]. However, there is a growing amount of strong evidence that LBP, particularly chronic LBP, is fuelled by a combination of bio-psychosocial factors that lead to maladaptive behaviours and physiological changes that cause central sensitisation of the nervous system[30].
- This approach has been criticised for its exclusion of patho-anatomical factors; factors such as tissue healing which are important for effective treatment[31]
- One final limitation of the MIS approach to diagnosis of LBP is that it takes quite a long time to perform this thorough assessment. In a busy hospital outpatients setting, time constraints may limit the practicality of using this approach.
Other Points to Consider: Clinical Expertise and Practical Application[edit | edit source]
Interview with Catherine Moore, Physiotherapy Lecturer at The University of Nottingham
Considering a Combined Approach[edit | edit source]
Interview with Roger Kerry, Physiotherapy Lecturer at The University of Nottingham
Case studies: Applying Approaches to Clinical examples[edit | edit source]
Patient 1[edit | edit source]
A 36-year-old male, presents with a 2-week history of right sided low back pain. Patient works as a shop assistant and recently had to complete extra shifts for Christmas. Whilst bending down to lift a heavy box, he felt a sharp pain and immediately struggled to stand back up. He has been experiencing occasional numbness in his right leg when he has been walking for more than 15 minutes.
Aggs:Bending forwards, walking the dog, walking up hill
Eases: sleeping on front with pillows propped up, rest, hot water bottle over back
Patient 2[edit | edit source]
A 56-year-old female, presents with a 3-month history of central low back pain. She has been experiencing low back pain for the past 18 months but has been gradually getting worse over the last 3 months. She cannot recall any trauma or change in activity to flare up the pain. The patient is an office worker and is currently off work. she denies any leg and buttock symptoms, and has no obvious red flags.
She recalls having had 3 sessions of physiotherapy previously, which had some effect but he was too busy to carry on with the exercise regime. She cannot recall any of the exercises she was given previously.
Aggs: bending forward, rotating to L+R, bending to the side L+R
Eases: lying flat on back, hot baths, heat rub
Conclusions[edit | edit source]
As a whole, all three approaches have their strengths and limitations. Clinical opinions on all three show both positives and negatives. Choosing which approach to use tends to depend on the learning experience of a therapist during their time as a student, as well as clinical and personal experiences.
Approaches can be adapted and used in combination; allowing a thorough assessment and diagnosis of a patient’s problem, looking at both mechanical, structural and movement impairments.
References[edit | edit source]
- ↑ Gross A, Miller J, D’Sylva J, Burnie SJ, Goldsmith CH, Graham N, Haines T, Brønfort G, Hoving JL. Manipulation or Mobilisation for Neck Pain. Cochrane Database of Systematic Reviews 2010, Issue 1.
- ↑ Gracey J, McDonough S, Baxter D, Physiotherapy Management of Low Back Pain: A Survey of Current Practice in Northern Ireland, 2002, fckLRSpine, Vol 27(4), p 406-411
- ↑ Banks, K. Geoffrey D. Maitland, 1924–2010, Physical Therapy March 2010 vol. 90 no. 3 326 http://ptjournal.apta.org/content/90/3/326.full [accessed online 03/01/2014]
- ↑ Heiser R, O’Brien V, Schwartz D. The use of joint mobilization to improve clinical outcomes in hand therapy: A systematic review of the literature, 2013, Journal of Hand Therapy Vol 26, 297-311
- ↑ Hall J. Fundamentals Of Maitland Mobilizations, 2013 Morphopedics, SPThttp://morphopedics.wikidot.com/fundamentals-of-maitland-mobilizations [accessed 04/01/2014]
- ↑ 6.0 6.1 Powers C, Beneck G, Kulig K, Landel R, Fredericson M, Effects of a Single Session of Posterior-to-Anterior Spinal Mobilization andfckLRPress-up Exercise on Pain ResponsefckLRand Lumbar Spine Extension in PeoplefckLRWith Nonspecific Low Back Pain, 2008, Physical Therapy, Vol 88(4) p485-493
- ↑ 7.0 7.1 Maitland G, Hengeveld E, Banks K, English K, Maitland's Vertebral Manipulation, 7th Edition, 2005, Elsevier
- ↑ Dickenson, A H. Editorial I: Gate Control Theory of pain stands the test of time British Journal of Anaesthesia, 2002, Vol 88 (6): 755-757
- ↑ Maitland G. Maitland's Vertebral Manipulation. 7th ed. Philadelphia, PA. Elsevier. 2005
- ↑ Maitland Mobilization Grades Available on YouTube at http://www.youtube.com/watch?v=MNVLNP18dTA [accessed 03/01/2014]
- ↑ Chiradejnant A, Maher C, Latimer J, Stepkovitch N. Efficacy of “therapist-selected” versus “randomly selected” mobilisation techniques for the treatment of low back pain: A randomised controlled trial, 2003, Australian Journal of Physiotherapy, Vol. 49 233-241
- ↑ Seema S, Effect of Grade II and Grade III Mobilization by Maitland Technique in Low Back Pain, 2012, Indian Journal of Physiotherapy and Occupational Therapy - An International Journal, Vol 6 (4), p91 - 95
- ↑ Caraminos J, Marinko L. Effectiveness of Manual Physical Therapy for Painful Shoulder Conditions: A Systematic Review, 2009, The Journal of Manual and Manipulative Therapy, Vol 17, No.4, 206-215 fckLRAccessed 05/01/2014
- ↑ Naik VC, Chitra J, Khatri S. Effectiveness of Maitland versus Mulligan mobilization technique following post-surgical management of Colles fracture; randomized clinical trial, 2007. Indian Journal of Physiotherapy and Occupational Therapy. Vol 1(4):14-19.
- ↑ Bronfort G, Haas M, Evans R, Bouter L, Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis, 2004, The Spine Journal, Volume 4, Issue 3, P 335–356
- ↑ 16.0 16.1 16.2 May, S. and Donelson, R. Evidence- informed management of chronic low back pain with the McKenzie method. The Spine Journal. 2008;8:134-141
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 17.7 17.8 Karayannis, N.V., Jull, G.A. and Hodges, P. Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert opinion. BioMed Central Musculoskeletal Disorders.2012;13:24
- ↑ 18.0 18.1 18.2 18.3 Garcia, A.N., Costa, L.C.M., Silva, T.M., Gondo, F.L.B., Cyrillo, F.N., Costa, F.M., Costa, L.O.P. Effectiveness of Back School Versus McKenzie Exercises in Patients with Chronic Nonspecific Low Back Pain: A Randomized Control Trial.2013;93(6):729-747
- ↑ Namnaqani FI, Mashabi AS, Yaseen KM, Alshehri MA. The effectiveness of McKenzie method compared to manual therapy for treating chronic low back pain: a systematic review. Journal of Musculoskeletal & Neuronal Interactions. 2019;19(4):492.
- ↑ Clare,H.A., Adams, R.and Maher, C.G. Reliability of the McKenzie Classification of patients with cervical and lumbar pain. Journal of Manipulative and Physiological Therapeutics. 2005;28(2):122-127
- ↑ Machado, L.A.C., Sperling de Souze, M.V., Ferreira, P.H. and Ferreira, M.L. The McKenzie Method for Low Back Pain: A systematic Review of the Literature with a Meta-Analysis Approach. SPINE. 2006;31(9): 254-262
- ↑ Karayannis, N.V., Jull, G.A., and Hodges, P.W. (2012) Physiotherapy movement based classification approaches to low back pain: comparison of subgroups through review and developer/expert survey. BMC Musculoskeletal Disorders.13:24
- ↑ Sahrmann, S.A. (2001) Diagnosis and Treatment of Movement Impairment Syndromes. Mosby.
- ↑ 24.0 24.1 Van Dillen LR, Sahrmann SA, Norton BJ, et al. Effect of active limb movements on symptoms in patients with low back pain. J Orthop Sports Phys Ther 2001;31:402-413.
- ↑ Sahrmann, S.A. Diagnosis and Treatment of Movement Impairment Syndromes. Missouri: Mosby; 2002.
- ↑ Sahrmann Interviewed by L. Payne: 6th December 2012a part 1. Available at: http://www.youtube.com/watch?v=faEzHR5zLjs. [Accessed 13/01/14]
- ↑ Trudelle-Jackson, E., Sarvaiya-Shah, S. and Wang, S. Interrater reliability of a movement impairment-based classification system for lumbar spine syndromes in patients with low back pain. The Journal of Orthopaedic and Sports Physical Therapy 2009;38(6):371-376.
- ↑ Harris-Hayes, M., Van Dillen, L. and Sahrmann, S. Classification, treatment and outcomes of a patient with lumbar extension syndrome. Physiotherapy Theory and Practice 2005; 21(3):181-196.
- ↑ Sahrmann Interviewed by L. Payne: 6th December 2012b part 3. Available at: http://www.youtube.com/watch?v=TsDbmAyzMd8. [Accessed 13/01/14]
- ↑ O’Sullivan, P. It’s time for change with the management of non-specificfckLRchronic low back pain. Br J Sports Med 2011. Available from: http://bjsm.bmj.com/content/early/2011/08/04/bjsm.2010.081638.full.htmlfckLR[Accessed 11/01/14]
- ↑ Ford, J. J. and Hahne, A. J. Pathoanatomy and classification of low back disorders. Manual Therapy 2013.18:165-168