Diabetic Rehabilitation
Original Editors -Cindy John-Chu and ReLAB-HS
Top Contributors - Cindy John-Chu, Naomi O'Reilly, Kim Jackson, Rachael Lowe, Oyemi Sillo, Candace Goh, Rucha Gadgil, Ashmita Patrao, Aminat Abolade and Rishika Babburu
Introduction[edit | edit source]
Diabetes is a chronic metabolic disease in which the body is unable to appropriately regulate the level of sugar, specifically glucose, in the blood, either by poor sensitivity to the protein insulin, or due to inadequate production of insulin by the pancreas. It is characterised by hyperglcaemia following a disorder of insulin secretion, insulin action or both.[1] A diagnosis of diabetes is made when Fasting Plasma Glucose (FPG) is ≥ 126 mg/dL (7.0 mmol/L) on two occasions of testing, with fasting referring to no caloric intake for at least 8 hours.[2]
There are various forms of diabetes, with the most common being Type 2 Diabetes (T2D). Previously referred to as adult onset diabetes or non insulin dependent diabetes, risk factors for T2D may include:
- Family History
- Obesity
- Sedentariness
- Increasing Age
- History of Gestational Diabetes
- Race (more common with African American, American Indian, Hispanics and Asian American)[2]
Classification of Diabetes[edit | edit source]
The American Diabetes Association (ADA) classifies diabetes into four categories namely: [2]
- Type 1 Diabetes which is an absolute deficiency of insulin due to an autoimmune destruction of β cells in the pancreas. This also includes latent autoimmune diabetes of adulthood.
- Type 2 Diabetes occurs from insulin resistance and a progressive reduction in insulin secretion. T2D is largely attributed to physical inactivity and excess body weight [3].
- Gestational Diabetes, which is diabetes diagnosed in the second or third trimester of pregnancy and was not present prior to the pregnancy period.
- Specific type diabetes that are due to other causes such as monogenic diabetes syndromes, diseases of the exocrine pancreas, and drug or chemical induced.
Classification of the condition is important to aid appropriate management of the condition. According to the ADA, previous assumptions of Type 1 Diabetes occurring only in children and Type 2 Diabetes in adults is now outdated as the two conditions can be expressed both in adults and children alike.
Epidemiology[edit | edit source]
According to the World Health Organisation (WHO), there is an estimated 422 million people with diabetes worldwide and with most of these individuals living in low and middle-income countries[4]. This is beside the estimated projection by the international diabetes federation that 1 in 10 persons worldwide will have T2D by 2035.[5] It has also been reported by WHO that 1.6 million deaths can be directly linked to diabetes yearly. The aforementioned report went on to say that there is however a unified global target to prevent the rise in diabetes and obesity by 2025.[4]
Complications of Diabetes[edit | edit source]
Over time, diabetes causes damage to various systems of the body including: cardiovascular, neurological, musculoskeletal and integumentary systems with increased risk of developing comorbidities. It is known to affect specific organs such as the eyes, kidneys, nerves and heart. These complications may be categorized as acute or chronic.
Acute complications of diabetes include:
- Hypoglycaemia
- Diabetic ketoacidosis
- Hyperosmolar nonketotic coma [6]
Chronic complications of diabetes relate to the long term effects of hyperglycaemia on the vasculature and can be divided into:
- Microvascular complications consisting:
- Retinopathy
- Nephropathy
- Neuropathy (including peripheral distal symmetric polyneuropathy, autonomic neuropathy, proximal painful motor neuropathy and cranial mononeuropathy)
- Macrovascular complications including:
Management of Diabetes[edit | edit source]
Management can either be pharmacological or non-pharmacological. To effectively tackle diabetes and its complications, lifestyle adjustments including diet and exercise are often recommended to ensure optimal health. Also patients are encouraged and educated on how to manage their conditions by themselves to achieve optimal results from the lifestyle modifications. Diabetes treatment is mainly aimed at glycaemic control, improving quality of life of patients, preventing complications and ultimately reducing mortality in this patient population.[8]
Pharmacological Interventions[edit | edit source]
- Insulin Therapy: This is an essential treatment in patients with type 1 diabetes as the condition is marked with a dysfunction in β cell function.[9] To achieve best results and to prevent metabolic disturbances, the administration of insulin is recommended to be through injections given on a daily basis or via a continuous subcutaneous pump.[9][10]
- Pramlintide is an adjuvant glucose lowering medication that acts based on the naturally occurring β-cell peptide, amylin and is recommended for use in patients with type 1 diabetes.[9]
- Metformin is the preferred medication for the management of type 2 diabetes.[9]
- Sulfonylureas can either be used instead of metformin if the patient is not overweight or unable to tolerate metformin and it can be administered with metformin if glycaemic control is inadequate.[11]
Non-pharmacological Interventions[edit | edit source]
The non-pharmacological management of diabetes is basically centred on lifestyle changes with exercise and diet being the main stay of the programme. Lifestyle modification is recommended to avoid infusion with insulin.
Nutritional Intake[edit | edit source]
Integrating an individualised meal plan is essential to achieving positive outcomes with these patients. The portion and types of food eaten may affect the balance of insulin and consequently, levels of blood glucose. It has been reported that the quality of the dietary intake rather than the quantity is more important. As such, diets rich in whole grain, fruits, vegetable, nuts; lower in refined grains, red or processed meat and sugar-sweetened beverages; and moderate in alcohol are recommended as they help improve glycaemic control and lipids in patients with diabetes.[12]
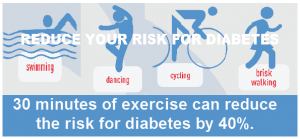
Physical Activity & Exercise[edit | edit source]
Physical activity (PA) is any form of movement that promotes the use of energy, while exercise is any planned and/or structured PA and are both beneficial for all patients with diabetes.[13] Exercise programmes are geared towards improving quality of movement, participation in activities of daily living, managing pain if any, lowering blood sugar and ultimately slowing the progression of the condition and its multi systems complications.
A combination of aerobic and resistance training exercises has been recommended in planning exercise programmes for this population as it has been reported to produce positive effects on blood glucose levels. Flexibility and balance exercises are reported to be beneficial for older patients with diabetes as the former will help in improving range of motion at joints, while the latter can aid in reducing fall risks.[13]
While exercise may be good, precautions should be taken to avoid exercise related complications in patients with diabetes for which the ADA recommends that:[13]
- There should be appropriate progression of exercises to minimise risk of injury
- People, especially older ones, with diabetic complications such as autonomic neuropathy, cardiovascular or pulmonary disease should avoid exercising outdoors on very hot and humid days.
- Doses of medications with tendency to cause hypoglycaemia besides insulin should be adjusted based on exercise training.
- Exercise-induced hyperglycaemia, which is more common in patients with T1D, can be mitigated with either a lower intensity aerobic cooldown or insulin administration.
- Resistance exercise should be performed before aerobic exercise in the same session to prevent exercise-induced hypoglycaemia
Rehabilitation as an Intervention in the Management of Diabetes[edit | edit source]
The prevalence of diabetes is projected to be on the rise and as such, the increasing demand on rehabilitation services to curb the complications the condition presents with.[14] Management of diabetes requires a lifelong multi-faceted treatment approach to achieve set goals. Major goals of diabetic rehabilitation are to: attain glycaemic control, improve quality of life, prevent or delay complications and empower patients with the knowledge of their condition.
Patient education is important to help people with diabetes enhance self care. It involves providing information on the need and importance of PA and exercise as well as encouraging active participation as they are pivotal in the rehabilitation of this population. As such, it is imperative to develop an individualised and structured PA/exercise plan for each patient, while still taking their pharmacological management and dietary change into consideration.
Physical activity is known to improve the uptake of glucose as an increased blood flow to muscles enhances glucose uptake in muscle cells; improve the sensitivity of insulin to excess blood glucose and reduce intra-abdominal fat - a known risk factor for insulin resistance; and prevent cardiovascular complications.[15][16] In those with cardiovascular disease, it helps prolong survival and improve exercise capacity while it postpones the occurrence of diabetes and its complications in non-diabetic individuals[17]. Also, the ADA recommends that people with pre-diabetes should be enrolled in diabetes prevention programmes to gain and sustain a 7% loss of previous body weight and increase moderate-intensity PA to about 150 minutes per week.[10]
Tele-rehabilitation should also be considered when managing individuals with diabetes. In a recent study, tele-rehabilitation which consisted of breathing exercises and calisthenics, three times a week over a six-week period showed improvement in the psychosocial status and exercise capacity of individuals with diabetes.[18] Rehabilitation of diabetes patients can take place in either an in-patient or out-patient setting.
Resources[edit | edit source]
- American Diabetes Association: Standards of Medical Care in Diabetes -2021
- American Diabetes Association: Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association
References [edit | edit source]
- ↑ Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabetic medicine. 1998 Jul;15(7):539-53.
- ↑ 2.0 2.1 2.2 American Diabetes Association. Addendum. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021; 44 (Suppl. 1): S15-S33. Diabetes care.:dc21ad09.
- ↑ World Health Organisation, Diabetes. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed 27 July, 2021).
- ↑ 4.0 4.1 World Health Organisation, Diabetes. Available from: https://www.who.int/health-topics/diabetes#tab=tab_1 (accessed 27 July, 2021).
- ↑ Leon BM, Maddox TM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World journal of diabetes. 2015 Oct 10;6(13):1246.
- ↑ Stanley F, Malamed DDS, Daniel L,
Diabetes Mellitus: Hyperglycaemia and Hypoglycaemia. In Stanley F, Malamed DDS, Daniel L (editors). Medical Emergencies in the Dental Office (seventh Edition). Mosby, 2015. Pg255 -280 - ↑ Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of diabetes 2017. J Diabetes Res. 2018; 2018: 3086167.
- ↑ Pontarolo R, Sanches ACC, Wiens A, Perlin CM et al. Pharmacological Treatments for Type 2 Diabetes. In: Croniger C (Editor). Treatment of Type 2 Diabetes. Online: IntechOpen, 2015 April1:147. Available from: https://www.intechopen.com/books/treatment-of-type-2-diabetes/pharmacological-treatments-for-type-2-diabetes-
- ↑ 9.0 9.1 9.2 9.3 American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: Standards of Medical Care in Diabetes—2021. Diabetes Care. 2021 Jan 1;44(Supplement 1):S111-24.
- ↑ 10.0 10.1 American Diabetes Association. 3. Prevention or delay of type 2 diabetes: standards of medical care in diabetes—2021. Diabetes Care. 2021 Jan 1;44(Supplement 1):S34-9.
- ↑ Packer ME, Crasto W. Type 2 diabetes: pharmacological management strategies. The Pharmaceutical Journal 2015 Available from: https://www.pharmaceutical-journal.com (accessed 17/02/2021)
- ↑ Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. The Lancet. 2014 Jun 7;383(9933):1999-2007.
- ↑ 13.0 13.1 13.2 Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes care. 2016 Nov 1;39(11):2065-79.
- ↑ Schmidt C, Baumert J, Gabrys L, Ziese T. Diabetes Mellitus in the Medical Rehabilitation-Use of Rehabilitation Services During 2006-2013. Die Rehabilitation. 2018 Jul 26;58(4):253-9.
- ↑ Zdrenghea D, Pop DA, Penciu OA, Zdrenghea V, Zdrenghea M. Rehabilitation in diabetic patients. Rom J Intern Med. 2009 Jan 1;47(4):309-17.
- ↑ Sami W, Ansari T, Butt NS, Ab Hamid MR. Effect of diet on type 2 diabetes mellitus: A review. International journal of health sciences. 2017 Apr;11(2):65.
- ↑ Mekonne, HS. Rehabilitative care of adult with diabetes mellitus. Journal of Clinical Case Studies. 2018; 9(2).
- ↑ Duruturk N, Özköslü MA. Effect of tele-rehabilitation on glucose control, exercise capacity, physical fitness, muscle strength and psychosocial status in patients with type 2 diabetes: a double blind randomized controlled trial. Primary care diabetes. 2019 Dec 1;13(6):542-8.