Developing Physically Active and Sporty Kids - Injuries Specific to Children and Teenagers
Top Contributors - Jess Bell, Naomi O'Reilly, Kim Jackson, Wanda van Niekerk, Lucinda hampton and Aminat Abolade
Introduction[edit | edit source]
While physical activity levels in young people have decreased,[1] large numbers of children and teenagers still participate in organised sports.[2] Moreover, training for children is becoming more intense[3] and young people are often specialising in specific sports at younger ages.[4] There are correspondingly high injury rates in these children, including overuse injuries, and some children experience burnout.[4] Children are not, however, “mini-adults” - they tend to present with different injuries to those typically observed in adults.[4] This page discusses some common injuries that are specific to children and teenagers.
Know Your Child’s Age[edit | edit source]
As DiFiori and colleagues state, "chronological age is not a good indicator on which to base sport developmental models because motor, cognitive and social skills progress at different rates, independent of age."[5] There are a number of "ages" which must be considered when working with children, including their:[4]
- developmental Age
- skeletal Age
- general Training Age
- sport-specific Training Age
- relative Age
It is also useful to monitor a child’s growth. This might include regular (e.g. quarterly) height measurements in standing and crook sitting, as well as measuring their arm span. This monitoring can help to identify peak velocity height (i.e. the time when the child is growing the fastest). Table 1 shows typical growth per year for young people aged between 6 and 20 years.[4]
| Age (years) | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Height (cm) | 5 | 4.8 | 5 | 4.8 | 5 | 4.8 | 8.6 | 12 | 7.7 | 3.3 | 2.3 | 1.9 | 1.3 | 0.9 | 0.5 |
Common Injuries in Children[edit | edit source]
Why are Injuries in Children Different to those in Adults?[edit | edit source]
The injuries observed in children are often different to those seen in adults for a number of reasons, including:[4]
- Weak attachment site (causing avulsion fractures):[6]
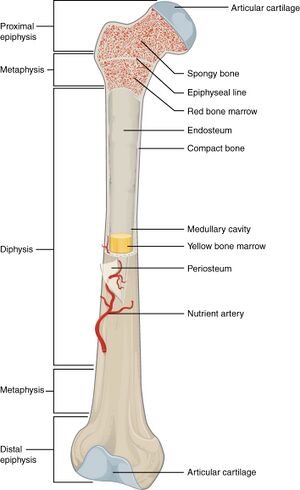
- Growth plate cartilage in children is less able to resist stress when compared to articular cartilage in adults. It is also less resistant to shear and tension forces than the surrounding bone. This can lead to a failure of the physis (see Figures 1 and 2) when increased stress is applied. Thus, in incidents where adults experience a complete tear of a ligament or joint dislocation, children might experience a growth plate separation. Children appear to be more prone to growth plate injuries during periods of rapid growth (see Table 1).[6]
- A mismatch between bone growth and muscle growth, which leads to incoordinated movements, and thus fracture
- Weaker physis, which can lead to fracture (see above)
Types of Injuries[edit | edit source]
Apophysitis:[7]
- Caused by traction injuries to the cartilage and bony attachment of tendons in children and adolescents
- Often related to overuse in children who are growing and have tight / inflexible muscle tendon units
- Occurs in upper and lower extremities, but more common in the lower limb
- Examples include Sinding Larsen Johansson syndrome, Osgood-Schlatter's diseaseand Sever's disease
- Less common than apophysitis, but osteochondroses are a group of conditions that affect the epiphysis (see Figures 1 and 2 to see the epiphysis)[4]
- They occur when there are degenerative changes in the epiphyseal ossification centres of growing bones
- Caused by a temporary disruption of blood supply at the bone-cartilage complex, rather than traction
- The aetiology of this disruption is not known
- "Multiple possible etiologies have been explored, including genetic causes, hormonal imbalances, mechanical factors, repetitive trauma, and vascular abnormalities."[7]
- They tend to resolve spontaneously, but should be monitored (surgery rarely required)
- Examples include Kohler's disease and Legg-Calve-Perthes disease
Metaphyseal Fractures:[4]
- Fractures that affect the metaphysis of tubular bones[8]
- Occur most often in the forearm and lower leg
Avulsion Fractures:
- Occur when there is a failure of the bone - a bone fragment is: “pulled away from its main body by soft tissue that is attached to it.”[9]
During periods of rapid growth in children, bone lengthens before the muscles and tendons have time to stretch and develop the necessary strength and coordination to control this new longer bone. This can lead to awkwardness in a child’s movement patterns.[4]
- Traumatic injuries lead to fractures of the bone or growth plate, such as:
- Greenstick fracture - i.e. a partial thickness fracture - the cortex and periosteum are disrupted on one side of the bone only. They are unaffected on the other side.[10] They are most common in children aged under 10 years, although they can occur at any age.[10]
- Premature growth plate fracture = stress fracture
- Strong incoordinated contractions of the muscles lead to avulsion fractures, rather than a tear of the muscle or tendon[4]
Table 2 lists common growth plate injuries / osteochondroses. These injuries tend to be treated conservatively except for those which affect the hip and the knee.[4] Click the links for more information on these conditions.
| Non-Articular (related to overuse) | Articular | Physeal |
|---|---|---|
| Osgood-Schlatter's Disease:
Tibial tubercle apophysitis. Tends to occur during bone maturation (10-12 years in girls and 12-14 years in boys).[11] |
Legg-Calve-Perthes Disease:
Affects the femoral head. Ocurs in children aged 4 to 10 years. |
Scheuermann’s Disease:
Hyperkyphosis of the thoracic spine. Commonly diagnosed in adolescents aged between 12 and 17 years.[12] |
| Sinding Larsen Johansson Syndrome: Inferior pole of the patella apophysitis.
Tends to occur in active male patients aged 10-13 years.[13] |
Kienbock’s Disease:
Avascular necrosis of the lunate (carpal bone). More common in individuals aged 20 to 30 years. |
Blount’s Diease:
Proximal tibial growth plate. Tends to occur in obese children aged 9 to 10 years.[14] |
| Sever’s Disease:
Calcaneal apophysitis. Commonly occurs during periods of rapid growth in active children aged 9-12 years.[15] |
Kohler's Disease:
Affects the navicular. Occurs in children age 2 to 8 years, but is more common in children aged 4 to 6 years.[16] |
Triangular Fibrocartilage Complex (TFCC) Impingement:
Increasingly recognised in children. Occur after acute rotational injuries or post-distal radius fracture. Cause ulnar-sided wrist pain.[17] |
Osteochondritis Dissecans:
Can affect children and adults, but the majority of patients are in their teens.[18] |
Table 3 lists common fractures found in children.
| Metaphyseal Fracture | Avulsion Fracture | Growth Plate Fractures |
|---|---|---|
| Mostly occur in the forearm and lower leg | Common sites include:
|
Salter-Harris fractures:
Types I and II
Type V[20]
NB: even if an x-ray is normal, a history of severe rotational or shear force with localised swelling, bony tenderness and loss of function can indicate a growth plate fracture.[4] |
Take Home Message[edit | edit source]
When a child presents with a traumatic injury, fracture should be considered. When pain has been present for a longer period or appears related to overuse, growth plate injuries should be considered rather than tendinopathy, ligament sprain, tendon or muscle tear.[4]
Management of Injuries in Children[edit | edit source]
Avulsion Fractures:[4]
- Musculotendinous avulsion fractures are treated conservatively (i.e. the same as a grade III muscle tear)
- Ligamentous avulsion fractures are often treated with surgery, so the child will need to be assessed by a specialist
Metaphyseal Fractures:[4]
- Must be immobilised
- Tend to heal quickly (3 weeks)
Growth Plate Injuries:[4]
- Usually require conservative management / load management, especially in children who present with Osgood-Schlatter's disease and Sever's disease
- If pain levels are high and the child has difficulty weight-bearing, they may require crutches for a time (1 to 2 weeks)
- Load is then gradually reintroduced
- A graded exposure approach to load can be adopted so that the system starts to accommodate and build up a tolerance to load
Osteochondosis / Osteochondritis Dissecans:[4]
- The child should be referred to a specialist who can determine if immobilisation or surgical intervention are required
References[edit | edit source]
- ↑ Frömel K, Groffik D, Mitáš J, Madarasová Gecková A, Csányi T. Physical activity recommendations for segments of school days in adolescents: support for health behavior in secondary schools. Front Public Health. 2020;8:527442.
- ↑ Safe Kids Worldwide. Preventing sports-related injuries. Available from: https://www.safekids.org/preventing-sports-related-injuries (accessed 7 November 2021).
- ↑ Stricker PR, Faigenbaum AD, McCambridge TM; COUNCIL ON SPORTS MEDICINE AND FITNESS. Resistance Training for Children and Adolescents. Pediatrics. 2020;145(6):e20201011.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 Prowse T. Developing Physically Active and Sporty Kids - Injuries Specific to Children and Teens Course. Plus , 2021.
- ↑ DiFiori JP, Benjamin HJ, Brenner J, Gregory A, Jayanthi N, Landry GL, Luke A. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24(1):3-20.
- ↑ 6.0 6.1 Caine D, DiFiori J, Maffulli N. Physeal injuries in children's and youth sports: reasons for concern?. Br J Sports Med. 2006;40(9):749-60.
- ↑ 7.0 7.1 7.2 7.3 Achar S, Yamanaka J. Apophysitis and osteochondrosis: common causes of pain in growing bones. Am Fam Physician. 2019;99(10):610-8.
- ↑ Jones J. Metaphyseal fracture. Reference article, Radiopaedia.org. Available from: https://radiopaedia.org/articles/metaphyseal-fracture-2 (accessed 9 November 2021).
- ↑ McCoy JS, Nelson R. Avulsion Fractures. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559168/
- ↑ 10.0 10.1 Atanelov Z, Bentley TP. Greenstick Fracture. [Updated 2021 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513279/
- ↑ Physiopedia Osgood-Schlatter Disease.
- ↑ Mansfield JT, Bennett M. Scheuermann Disease. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499966/
- ↑ Physiopedia. Sinding Larsen Johansson Syndrome.
- ↑ Dakshina Murthy TS, De Leucio A. Blount Disease. [Updated 2021 Jul 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560923/
- ↑ Smith JM, Varacallo M. Sever Disease. [Updated 2022 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441928/
- ↑ Weerakkody Y, Bell D. Köhler disease. Reference article, Radiopaedia.org. Available from: https://radiopaedia.org/articles/k-hler-disease (accessed 9 November 2021).
- ↑ Lee SJ, Bae DS. Triangular fibrocartilage complex injuries in children and adolescents. Hand Clin. 2021 Nov;37(4):517-526.
- ↑ Wood D, Davis DD, Carter KR. Osteochondritis Dissecans. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526091/
- ↑ Johns K, Mabrouk A, Tavarez MM. Slipped Capital Femoral Epiphysis. [Updated 2021 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538302/
- ↑ Levine RH, Foris LA, Nezwek TA, et al. Salter Harris Fractures. [Updated 2021 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430688/
- ↑ nabil ebraheim. Salter Harris Fracture Classification - Everything You Need To Know - Dr. Nabil Ebraheim. Available from: https://www.youtube.com/watch?v=uQYsagiJi7c [last accessed 10/11/2021]