Degenerative Disc Disease
Original Editor - Amanda E Davidson and Colby Boers, Lisa Pernet
Top Contributors - Lisa Pernet, Gaëlle Vertriest, Admin, Vanbeylen Antoine, Amanda E Davidson, Garima Gedamkar, Candace Goh, Uchechukwu Chukwuemeka, Laura Ritchie, Scott Cornish, Kim Jackson, WikiSysop, 127.0.0.1, De Maeght Kim, Lucinda hampton, Aya Alhindi and Eric Robertson
Search Strategy[edit | edit source]
Internet is a gigantic source of knowledge. Databases such as PubMed, Web of Science, PEDro or Google Scholar can be useful. Use keywords as ‘Degenerative Disc Disease’, Lumbar Disc Disease, exercise therapy degenerative disc, discogenic pain, etc. For specific information you can use ‘AND’ and add ‘physical therapy’, ‘characteristics’, ‘definition’, 'treatment', depending of the need. To find an appropriate physical therapy the use of books is recommended.
Definition/Description[edit | edit source]
Degenerative disc disease (DDD) is a process in which the intervertebral discs, which provide cushioning between the vertebra of the spine, lose height and hydration. When this occurs, the intervertebral discs are unable to fulfill their primary functions: cushioning and providing mobility between the vertebrae.
Although the exact cause of DDD is unknown, it is thought to be associated with the aging process during which the intervertebral discs become dry, lose elasticity, and collapse. Furthermore a degenerative disc disease may develop at any level of the spine, but is most common in the cervical and lower lumbar sections of the spine.[1][2][3]
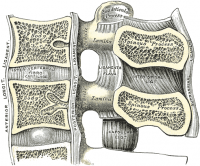
Clinically Relevant Anatomy[edit | edit source]
Lumbar DDD is a condition that can imply lower back pain, this results from the co-existence of two different time scales: on one hand the slow dynamics of disc degeneration and on the other hand the fast dynamics of pain recurrence. [4]
Lumbar DDD can also imply radiating pain from damaged discs in the spine. A lumbar spinal disc acts as a shock absorber between two vertebrae and allows the joints and the spine to move easily. The outer portion, the annulus fibrosis, contains the soft inner core of the disc, the nucleus pulposus. Each person’s spinal discs undergo degenerative changes as they age. But not all people will notice symptoms as a result of these changes. One of the ways DDD causes pain is through inflammation of the nerves. When the outer portion of the disc breaks, the inner part can leak out, releasing proteins that can irritate the nerves surrounding from the disc. Another cause is when degenerated discs can’t properly absorb stress. Leading to abnormal movement around the vertebral segment. Back muscles will hereby spasm painfully in order to stabilize the spine. In some cases the segment may collaps so a nerve root gets compressed, leading to radiculopathy. the pain from DDD often goes away with time because the inflammatory proteins will disappear and the disc collaps in a stable position. [5]
Intervertebral Discs
Dengenerative Disc Disease (DDD) is thought to begin with changes to the annulus fibrosis, intervertebral disc, and subchondral bone. The process of degeneration is divided into three classifications including: early dysfunction, intermediate instability, and final stabilization.
Early dysfunction is the classifed as the beginning of degenerative changes which can occur as early as 20 years. Intermediate instability is classified by a loosening of the annulus fibrosis, which can cause back pain. Fibrosis to the posterior structure and formation of osteophytes denotes the final stabilization classification. Pain decreases, and motion descreases. [6]
Epidemiology /Etiology[edit | edit source]
Degenerative disc disease refers to a condition in which the involved disc causes LBP. Lumbar degenerative disc disease is usually the result of a twisting injury to the lower back, such as when a person swings a golf club or rotates to put an object on a surface to the side of or behind them.[7]
The pain is also frequently caused by simple wear and tear on the spine and comes with the general aging process.
Degenerative disc disease is fairly common, and it is estimated that at least 30% of people aged 30-50 years old will have some degree of disc space degeneration, although not all will have pain or ever receive a formal diagnosis.[7]
The process that leads to DDD begins with structural changes. The annulus fibrosis (outer portion of the disc) loses water content over time which will make it increasingly unyielding toward everyday stress and strain on the spine. The loss of compliance in the discs contributes to forces being redirected from the anterior and middle portions of the facets to the posterior aspect, thus causing facet arthritis. Another result is hypertrophy of the vertebral bodies adjacent to the degenerating disc. The overgrowths are known as bony spurs (or osteophytes.)
Characteristics/Clinical Presentation[edit | edit source]
| [8] |
DDD commonly occurs with other diagnoses such as:
- idiopathic low-back pain
- lumbar radiculopathy
- myelopathy
- lumbar stenosis
- spondylosis[3]
- osteoarthritis
- zygapophydeal joint degeneration [6]
Activities that typically increase pain include:
- Sitting for extended periods of time
- Rotating, bending, or lifting
- Activities that typically decrease pain include:
- Changing positions often
- Lying down
- Staying active [9]
Differential Diagnosis[edit | edit source]
People with DDD will have low back pain[8]; however there are varying levels of severity. Pain is often chronic, but one with DDD can experience varying episodes of exacerbation where pain levels are elevated[9]
There are different degrees of annular disruption[1]. We can classify them into 4 grades, at which grade 0 is added. We differentiate these grades by means of a contrast medium injection.
- Grade 0: no disruption
- Grade 1: the contrast medium passes into the cartilage endplate through tear
- Grade 2: the contrast medium flows into the bony endplate
- Grade 3: the contrast medium is going into the cancellous bone of vertebra under endplate
- Grade 4: the contrast medium leaks completely in the cancellous bone.
Diagnostic Procedures[edit | edit source]
Provocation discography is a diagnostic test to identify a painful disc. To evaluate the degree of disruption, a combination of discogram and CTscan afther discography is used.[1]
Xray findings are used to diagnose DDD. Anterior-Posterior and lateral views are taken; presence of osteophytes, narrowing of the disc joint space, or a “vacuum sign” is noted. [10]
Outcome Measures[edit | edit source]
None of the analyzed literature has reported a uniform system of outcome measuring. The most common form of outcome measure for DDD is Oswestry Disabilty Index (ODI) in combination with other forms of outcome measure: Short Form 36(or SF-12) questionnaire, self-paced walk, timed up-and-go test (TUG),Visual Analogue Scale (VAS), Roland-Morris disability index (RMDI)[11][12] (level of evidence 3A,1B).
A radomized controle trial (Lars G Johnsen et al., 2013, level of evidence:1B ) analysed the difference between the ODI, the SF6D and the EQ5D.
In their research the several outcome measures reached different scores in the Receiver Operator Curve (ROC). The ODI showed a sensitivity of 88% and specificity of 85%, the EQ5D a sensitivity of 73% and specificity of 79% and the SF6D a sensitivity 93% and specificity 78%. But the EQ5D and the SF6D don’t measure the same constructs and therefore cannot be used interchangeably.[13]
A systematic review tried to evaluate wich outcome measure were suitable for DDD. They found out that the Oswestry Disability Index a good primary outcome measure is for lumbar fusion and nonsurgical interventions for various symptomatic degenerative spine disorders (level of evidence: 3A).[14] Although further research is needed.
Examination[edit | edit source]
It is very important to look at the patient’s history, this is a very valuable tool for identifying the intervertebral disc as the nociceptive source. Patients may present with a history of Chronic LBP, and can experience symptoms into the buttock. They may also state a history of spine stiffness that gets worse with activity and tenderness with palpation over involved area. [10]
Mood and anxiety disorders were diagnosed using the Structured Clinical Interview of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition/Clinical Version Mood and anxiety disorders were more commonly seen in patients with lumbar or cervical disc herniation than in those without herniation. No relationship was detected between pain severity and mood or anxiety disorders. However, mood and anxiety disorders were associated with neurological deficits. [15]
Magnetic resonance imaging (MRI) is the most common used method of specifically assessing intervertebral disc degeneration. Based on proton density, water content an chemical environment MR depicts disc hydratation and morphology which can be visualized on MR images with T2 weighting as hypointense signal. Pfirrmann et al devised a grading system for disc degeneration based on MR signal intensity, disc structure, distinction between nucleus and anulus, and disc height.[16] This useful grading system has been accepted and applied clinically
The modified system comprises 8 grades for lumbar disc degeneration (Griffith et al. (2007), Table 1). Sagittal T2-weighted images were used for classification as they provide a comprehensive perception of disc structure and good tissue differentiation.The 8 grades represented a progression from normal disc to severe disc degeneration. Grade 1 corresponds to no disc degeneration while Grade 8 corresponds to end-stage degeneration. Beside the 8-grade table there is also an image reference panel (Griffith et al. (2007), Figure 1).[17]
Medical management
[edit | edit source]
The preferential treatment for patients with chronic low back pain, caused by disc degeneration, is a conservative method consisting of physical therapy and medications (O'Halloran, 2007 (D)). [18]
Conservative treatment (home or hospital) includes rest, adequate program for motoractivity, regime of physical activity, strengthening of musculature, analgetic medication, physiotherapy, rehabilitation programs and lifestyle adjustments such as weight loss. [19]
Medications such as non-steroidal anti-inflammatories (e.g., ibuprofen, naproxen, COX-2 inhibitors) and pain relievers like acetaminophen (such as Tylenol) help many patients feel good enough to engage in regular activities. Stronger prescription medications such as oral steroids, muscle relaxants or narcotic pain medications may also be used to manage intense pain episodes on a short-term basis, and some patients may benefit from an epidural steroid injection. Not all medications are right for all patients, and patients will need to discuss side effects and possible factors that would preclude taking them with their physician. Epidural steroid injections can provide low back pain relief by delivering medication directly to the painful area to decrease inflammation.
Lately, successful outcomes were demonstrated by animal experiments with mesenchymal stem cells.[19][1]
Surgical intervention includes disc arthroplasty and lumbar spinei[1][19] fusion to reduce chronic low back pain due to degenerative disc disease.[21]
In some cases another form of chirurgical management is used for treatment of DDD, it is named: Device for Intervertebral Assisted Motion (DIAM). The DIAM is a polyester-encased silicone interspinous dynamic stabilization device that can unload the anterior column and reestablish the functional integrity of the posterior column. This device is designed for preservation of the functional spinal unit. [22] (Level of evidence 2B)
In some other cases, patients are not responsive to nonsurgical treatment for symptomatic degenerative disc disease (DDD). In that case patients can undergo a lumbar total disc replacement (TDR). Patients presenting with symptomatic single-level lumbar DDD who failed at least 6 months of nonsurgical management were randomly allocated to treatment with an investigational TDR device (also called: TDR activL device) or FDA-approved control devices TDR. After 2 years of research, we can conclude that the single-level activL TDR is safe and effective for the treatment of symptomatic lumbar DDD. Lumbar total disc replacement (TDR) improved mean back back pain. (level of evidence: 2B) [23]
Physical management[edit | edit source]
A part of the physical therapy treatment is aimed at reducing pain. For this purpose, different physical modalities are used, including heat and cold application, traction, spinal manipulations (Beattie P, 2008 (D); Zhang Y (C), 2008; Mirza SK, 2007 (A1))[24][25][26], exercise programs and electrical stimulation such as ‘TENS’ and ‘pulsed radiofrequency (PRF)’ treatment[27] and lifestyle modifications (e.g., weight reduction, smoking cessation).[28] With this PRF treatment, 56% of 76 patients with discogenic pain had more than 50% pain reduction one year after the first treatment. Among exercise approaches, unloaded movement facilitation exercises of McKenzie, core strengthening, and core stabilization exercises are all effective in pain reduction for degenerative disc disease.[29]
Spinal manipulations
The HVLA is a spinal manipulation that includes many different techniques and may involve preliminary preparation of the joint and its surrounding tissues, using stretching, assisted motion and other methods. Loads, both forces and moments, are applied to the joint, and it is moved to its end range of voluntary motion. An impulse is then applied, the effective load is the summation of forces applied by the operator, with the inertial forces generated by the motion of body segments, and the internally generated tensions from client muscle reactions. (Triano et al, 1997 (level of evidence 3A))[30]
The HVLa is a (High-Velocity, Low-amplitude) SM (Spinal Manipulation) in the lumbosacral joint performed on men with degenerative disc disease. This immediately improves self-perceived pain, spinal mobility in flexion, hip flexion during the passive SLR test, and subjects' full height (Vieira-Pellenz F et al, 2014 (level of evidence 1B)) [31](= full height recovery after high-velocity, low-amplitude (HVLA) spinal manipulation (SM) in the Lumbosacral joint (L5-S1)). Before Spinal Manipulation Therapy (SMT) can be considered as a treatment option, patients with LBP need to be screened for possible serious pathology. There are two reasons for this: some conditions, such as a fracture, affect the mechanical integrity of the spine and would make SMT clearly dangerous. In other conditions, a failure to recognize the condition delays commencement of more appropriate care. For example, early detection and treatment of spinal malignancy is important to prevent the spread of metastatic disease and the development of further complications such as spinal cord compression. Application of SMT with the presence of red flags cancer and fracture, should be considered as contraindications to SMT until further investigation has excluded serious pathology. The other red flags would only be contraindications to SMT if more than one were positive. (Hancock MJ et al 2008 (level of evidence 2C))
Core Stability
Other objectives are to enhance the core stability by strengthening and improving the coordination between the abdominal and back muscles through a spinal stabilization program (Brox JI, 2003 (level of evidence A2)).[32] These stabilization exercises can increase the patient’s capacity to resist higher loads in the degenerative discs(Beattie P, 2008 (level of evidence D))[33]. According to studies the load on the vertebral column can be reduced by half thanks to the muscles. The problem is the fact that muscle tissue is reduced with a rate of 1 kg/year after reaching the age of 40.[34] A posterior dynamic stabilization program proved a significant improvement in pain and disability.[35][36] Strength training exercises performed 1-3 times a week for 3 months reduced the pain of 157 patients. Those patients were able to return to their jobs and hobbies and were able to stop the use of pain killers.[37]
Excercises are performed to reduce pain and to ensure stability by strengthening the hip extensors, hip flexors, abdominal muscles and the sacrospinalis muscles.[38] At first the patient has to perform muscle contractions of the abdominal muscles and the m. iliopsoas, this will lead to the relaxation of the paravertebral muscles. These exercises will also help regain some of the lumbar joint suppleness. The movement will also help to feed the disc by absorbing liquid. After two weeks standing excercises can be performed. The previous excercices can still be performed as warming up excercises. Other important excercises include rectification of the pelvis to restore the body symmetry and toning the back extensors and abdominal muscles. By stretching the back extensors and strengthening the abdominal muscles we can redivide some of the pressure placed on the lumbar intervertebral discs.(These excercises are also a part of the Williams method.)[39][40]
Some examples of Williams' Flexion Exercises are:
- Pelvic tilt
The patient lies on his back with bent knees. He presses his back into the ground and holds this position up to 10 seconds.
- Single or double Knee to chest
The patient lies on his back with bent knees. He pulls one of his knees up to his chest and holds this op to 10 seconds. This can be done with one or two knees at a time.
- Partial sit-up.
The patient starts with a pelvic tilt after wich he lifts his shoulders off the floor. He holds this position 2 seconds each time he does this.
- Hamstring stretch.
The patient sits with extended knees and reaches out to touch his toes with his hands. He goes as far as possible. Other ways to stretch your hamstrings:
- Hip Flexor stretch.
The patient starts with one foot in front of the other. The knee of the front foot is flexed. He bends forward untill his front knee touches his chest. Other ways to stretch the hip flexors:
- Squat
The patient is standing with both feet on shoulders width apart. He keeps his back in a neutral position as he bends his knees and hips lowering his body.
In combination with these excercises core stability excercises are recommended. Core stability excercises start with learning how to recruit the abdominal muscles. Abdominal hollowing and branching activates the m. transversus abdominis wich is an important stabilizing muscle. Performing abdominal hollowing and branching excercises prior to abdominal curls facilitates the activation of the transversus abdominis and internal obliques during the abdominal curling excercises.
M. transversus abdominis recruitment excercise:
The patiënt lies on his back and imagines there is a line connecting his two pelvic bones. This is the area he has to focus on. Try contracting the muscles in this area without sucking in or expanding your abdomen. While doing this keep breathing normal. Hold this contraction for at least 10 seconds and repeat this several times.[41]
Once the patient is capable of performing an isolated contraction of the m. transversus abdominis other excercises are allowed. These excercises include the curl up, side plank, prone plank, bridging and performing alternated leg and arm raises in a quadruped position. During these exercises the spine should maintain a neutral position and the pelvis shoud not be tilted. When these excercises are mastered the person can advance to excercises on a physioball. [41]
In the last phase of a core strengthening program emphasis should be placed on balance and coördination excercises. Various unstable surfaces can be used. Before performing any of the standing balance and coördination excercises abdominal branching techniques should be performed to warm up the abdominal muscles. The excercises should be functional and should involve acceleration, deceleration and dynamic stabilisation. Reflexive control and postural regulation excercises should also be included. Examples of these excercises are controlled falling lunges in different directions and jumps on one or two legs. To help create automatic postural control we can blindfold or distract the patient by giving him additional tasks.[41][42]
In patients with degenerative disc disease it is also advised to add behavioral therapy to the usual treatment since it has been shown that the addition of behavioral therapy gives better results (Brox JI, 2003 (level of evidence A2))[6]. This is related to the fact that the diagnosis of degenerative disc disease also entails many psychological effects. Many patients assume that degeneration means that their spine is becoming weaker, associated with constant pain. These erroneous thoughts often cause fear of movement (kinesiophobia) and lead to the avoidance of movements of the spine (Beattie P, 2008 (D))[33].
The task of the physical therapists includes giving information and advice to improve the compliance rate.(Mirza SK, 2007 (A1))[43]. Good communication with patients is of great importance, they have to realize that degeneration of the intervertebral disc is a normal aging process. The physiotherapist must help the patients to identify and overcome their fears and to adapt their coping strategies (Mirza SK, 2007 (A1))[43]. It is important that patients understand that they must stay active and that activities of daily life and other moderate physical activity will not cause additional damage or have adverse effects (Brox JI, 2003 (A2))[6]. Patients must be encouraged to perform low impact aerobic exercises, such as walking and water aerobics. Low impact aerobic conditioning ensures adequate flow of nutrients and blood to spine structures, and decreases pressure on the discs. They should avoid prolonged static postures as much as possible (Beattie P, 2008 (D); Brox JI, 2003 (A2)).[33][6]
Extension exercises are given to displace the pressure on the discus intevertebralis anteriorly. Some exercises are:
- Hollow the back
- Make a sphinx posture
- Lie with the upper body prone on a table, the legs hang off. Lift the legs against the force of gravity. This is a back strengthening exercise.
- The last exercise can also be carried out on a ball.[44][45][46]
Physical therapies should aim to promote healing in the disc periphery, by stimulating cells, boosting metabolite transport, and preventing adhesions and re-injury. Such an approach has the potential to accelerate pain relief in the disc periphery, even if it fails to reverse age-related degenerative changes in the nucleus. [47]
The use of low-level laser therapy is a viable option in the conservative treatment of discogenic back pain, with a positive clinical result of more than 90% efficacy, not only in the short-term but also in the long-term, with lasting benefits. In the research, a wavelength of 810 nm wavelength emitted from a GaAIAs semiconductor laser device with 5.4 J per point and a power density of 20 mW/cm(2) was employed. The treatment regimen consisted of three sessions of treatment per week for 12 consecutive weeks. All (50) but one patient had significant improvement in their Oswestry Disability Index score. This means their disability decreased. [48]
Resources
[edit | edit source]
add appropriate resources here
Clinical Bottom Line[edit | edit source]
DDD is a is a condition in which the intervertebral discs lose height and hydration. As result the intervertebral discs are unable to fulfill their primary functions. Although the exact cause of DDD is unknown, it is thought to be associated with the aging process. The most common location of this process is situated in the cervical and lower lumbar sections of the spine.
To diagnose DDD the use of X-rays is needed. To identify the painful disc, the provocation discography test should be used.
The common outcome measure for DDD is the Oswestry Disability Index, mostly in combination with another questionnaire like VAS or SF-36.
Multiple concepts of medical management are used to treat DDD.
Surgical techniques are:
● The DIAM,
● Disc arthroplasty
● Lumbar spinei fusion
● Total disc replacement
But the preferential treatment is conservative technique. This consists of physical therapy and medications (analgesic medication).
The aim of physical therapy for DDD is to reduce pain, to enhance the core stability, provide information and advise about the disease and teach behavioral therapy.
For pain reduction heat and cold application, traction, spinal manipulations, electrical stimulation (TENS, pulsed radiofrequency (PRF)) and exercise therapy are the used modalities.
To improve stabilization of the back and abdominal muscles, coordination exercises like core stability are the most suitable (see Physical Management: core stability).
With the use of behavioral therapy we expect that the patient rejects erroneous thoughts concerning his pathology and enhance his lifestyle.
Low-level laser therapy can be used for conservative treatment, but further research is needed.
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1pMPQVclnMMdhoCVXc_6QwikGZ1oJDfw8DH__4CDKu4nrbvM0x: Error parsing XML for RSS
</div>
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 Peng B., Pathophysiology, diagnosis, and treatment of discogenic low back pain, World J Orthop 2013 April 18; 4(2): 42-52 LEVEL OF EVIDENCE 1
- ↑ Dr Vanaclocha V., et al, Degeneratieve ziekte van het disc, Clinica Neuros Neurochirurgie, 2010fckLR(http://neuros.net/nl/algemene_degenerative_ziekte_van_disc.php) LEVEL OF EVIDENCE 5
- ↑ 3.0 3.1 McCormack BM, Weinstein PR. Cervical spondylosis. An update. West J Med 1996; 165(1-2): 43-51 (Level of evidence: 1A)
- ↑ Chang-jiang Zheng et al.; Disc degeneration implies low back pain; Theoretical Biology and Medical Modelling (2015) (Level of evidence: 2C)
- ↑ Spine-health, Degenerative Disc Disease Health Center, http://www.spine-health.com/conditions/degenerative-disc-disease (asseced 18-05-2016) (level of evidence 5)
- ↑ 6.0 6.1 6.2 6.3 6.4 Dutton M. Orthopaedic Examination, Evaluation, and Intervention. 2nd ed. New York, NY: McGraw-Hll; 2008.
- ↑ 7.0 7.1 Ullrich, P. F. (2006 11 6). Lumbar Degenerative Disc Disease. Retrieved 06 02, 2009, from Degenerative Disc Disease: http://www.spine-health.com/conditions/degenerative-disc-disease/lumbar-degenerative-disc-disease
- ↑ 8.0 8.1 7SecretsMedical. Degenerative Disc Disease. Available from: http://www.youtube.com/watch?v=UTBrVj7F6kI [last accessed 03/05/13]
- ↑ 9.0 9.1 O'Halloran DM, Pandit AS. Tissue-engineering approach to regenerating the intervertebral disc. Tissue Eng 2007; 13(8):1927-1954.
- ↑ 10.0 10.1 Thompson, J.C. MD. Netter's Concise Atlas of Orthopaedic Anatomy. (2002) Saunders Elsevier. p.36-7
- ↑ Bono, C. M., & Lee, C. K.; Critical Analysis of Trends in Fusion for Degenerative Disc Disease Over the Past 20 Years: Influence of Technique on Fusion Rate and Clinical Outcome; Spine Volume; 2004; vol. 29; p455-463. (level of evidence: 3A)
- ↑ Malhar N. Kumar, F. J. (2001); Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease; European Spine Journal volume 10; p309-313. (level of evidence: 1B)
- ↑ Lars G Johnsen, Christian Hellum, Øystein P Nygaard, Kjersti Storheim, Jens I Brox , Ivar Rossvoll, Gunnar Leivseth and Margreth Grotle; Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease; BMC Musculoskeletal Disorders; 2013; vol. 14; p148-157. (level of evidence: 1B)
- ↑ LY Carreon, S. G.; Fusion and nonsurgical treatment for symptomatic lumbar degenerative disease: a systematic review of Oswestry Disability Index and MOS Short Form-36 outcomes; The spine journal; 2007 (Level of evidence: 3A)
- ↑ Kayhan F, Albayrak Gezer İ, Kayhan A, Kitiş S, Gölen M. Mood and anxiety disorders in patients with chronic low back and neck pain caused by disc herniation. Int J Psychiatry Clin Pract. 2015 Nov 2:1-5. (level of evidence 1B)
- ↑ Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001;26:1873–8 (Level of evidence 2A)
- ↑ Griffith JF et al; Modified Pfirrmann grading system for lumbar intervertebral disc degeneration; Spine (Phila Pa 1976). 2007 Nov 15;32(24):E708-12. ( Level of evidence: 2C)
- ↑ O'Halloran DM, Pandit AS. Tissue-engineering approach to regenerating the intervertebral disc. Tissue Eng 2007; 13(8):1927-1954.
- ↑ 19.0 19.1 19.2 Drazin D., Rosner J., Avalos P., Acosta F., Stem cell therapy for degenerative disc disease, Advances in orthopedics, volume 2012, 8pg LEVEL OF EVIDENCE = 1
- ↑ uwaterloo. Waterloo's Dr. Spine, Stuart McGill. Available from: http://www.youtube.com/watch?v=033ogPH6NNE [last accessed 03/05/13]
- ↑ Phillips F.M., Slosar P.J., Youssef J.A., Andersson G., Papatheofanis F., Lumbar spine fusion for chronic low back pain due to degenerative disc disease, SPINE Volume 38, Nr 7, Pp. E409-E422, 2013 LEVEL OF EVIDENCE = 1
- ↑ Jean Taylor, M., Patrick Pupin, M., Stephane Delajoux, M., & Sylvain Palmer, M.; Device for Intervertebral Assisted Motion: Technique and Initial Results; Neurosurg Focus; 2007; p1-22. (Level of evidence 2B)
- ↑ Garcia R, Yue JJ, Blumenthal S, Coric D, Patel VV, Leary SP, Dinh DH,fckLRButtermann GR, Deutsch H, Girardi F, Billys J, Miller LE. Lumbar Total DiscfckLRReplacement for Discogenic Low Back Pain: Two-year Outcomes of the activL Multicenter Randomized Controlled IDE Clinical Trial. Spine (Phila Pa 1976). 2015 Nov 27 (2B)
- ↑ Beattie P. Current understanding of lumbar intervertebral disc degeneration: a review with emphasis upon etiology, pathophysiology, and lumbar magnetic resonance imaging findings. fckLRJOSPT 2008; 38(6):329-340
- ↑ Zhang Y. Biological treatment for degenerative disc disease: Implications for the field of Physical Medicine and Rehabilitation. Am J Phys Med Rehabil 2008, fckLR87(9): p.694-702
- ↑ Mirza SK, Deyo RA. Systematic Review of Randomized Trials Comparing Lumbar Fusion Surgery to Nonoperative Care for Treatment of Chronic Back Pain. Spine 2007; 32(7): 816-823
- ↑ Rohof O., Intradiscal pulsed radiofrequency application following provocative discography for the management of degenerative disc disease and concordant pain: a pilot study, Pain practice, 2012, Volume 12, Issue 5, Pg 342-349 LEVEL OF EVIDENCE 2
- ↑ Zhang Y, An HS, Tannoury C, Thonar EJ, Freedman MK, Anderson DG. Biological treatment for degenerative disc disease: implications for the field of physical medicine and rehabilitation. Am J Phys Med Rehabil. 2008 Sep;87 (level of evidence: 1A)
- ↑ lade SC, Keating JL: Unloaded movement facilitation exercise compared to no exercise or alternative therapy on outcomes for people with nonspecific chronic low back pain: a systematic review. J Manipulative Physiol Ther 2007;30:301–11(level of evidence: 1A)
- ↑ JJ Triano et al, „Use of chiropractic manipulation in lumbar rehabilitation”, Journal of RehabilitationResearch and Development, 1997. (level of evidence 3A)
- ↑ Vieira-Pellenz F et al„Short-Term Effect of Spinal Manipulation on Pain Perception, Spinal Mobility, and Full Height Recovery in Male Subjects With Degenerative Disk Disease: A Randomized Controlled Tria”l, American Congress of Rehabilitation Medicine, 2014 (http://www.ncbi.nlm.nih.gov/pubmed/24862763) (level of evidence 1B)
- ↑ Brox JI, Sorensen R, Friis A. Randomized Clinical Trial of Lumbar Instrumented Fusion and Cognitive Intervention and Exercises in Patients with Chronic Low Back Pain and Disc Degeneration. Spine 2003; 28(17):1913-1921
- ↑ 33.0 33.1 33.2 12.3 Beattie P. Current understanding of lumbar intervertebral disc degeneration: a review with emphasis upon etiology, pathophysiology, and lumbar magnetic resonance imaging findings. fckLRJOSPT 2008; 38(6):329-340
- ↑ Adam Gąsiorowski et al, Strength training in the treatment of degeneration of lumbar section of vertebral column, Annals of Agricultural and Environmental Medicine, Vol 20, No 2, 203–205, 2013 (level of evidence 3A)
- ↑ Zagra A., et al; Prospective study of a new dynamic stabilisation system in the treatment of degenerative discopathy and instability of the lumbar spine, Eur Spine J, 2012, 21, suppl 1: S83-S89 LEVEL OF EVIDENCE 2
- ↑ Canbay S., et al, Posterior dynamic stabilization for the treatment of patients with lumbar degenerative disc disease: long-term clinical and radiological results, Turkish Neurosurgery 2013, vol. 23, No. 2, 188-197 LEVEL OF EVIDENCE 2
- ↑ 41. Adam Gąsiorowski et al, Strength training in the treatment of degeneration of lumbar section of vertebral column, Annals of Agricultural and Environmental Medicine, Vol 20, No 2, 203–205, 2013 (level of evidence 3A)
- ↑ Johnson Olubusola E. Therapeutic Exercises in the Management of Non-Specific Low Back Pain, Low Back Pain, ISBN: 978-953-51-0599-2, 2012 (level of evidence 5)
- ↑ Lee M.,The effects of core muscle release technique on lumbar spine deformation and low back pain.J Phys Ther Sci.;27(5):1519-22, 2015 (level of evidence 1B)
- ↑ Mircea MOLDOVAN, Therapeutic Considerations and Recovery in Low Back Pain: Williams vs McKenzie, Timisoara Physical Education and Rehabilitation Journal. Volume 5, Issue 9, 2012 (level of evidence 5)
- ↑ 41.0 41.1 41.2 AKUTHOTA V., Core Stability Exercise Principles Akuthota, Curr. Sports Med. Rep., Vol. 7, No. 1, pp. 39Y44, 2008 (level of evidence 5)
- ↑ COSIO-LIMA, Effects of Physioball and Conventional Floor Exercises on Early Phase Adaptations in Back and Abdominal Core Stability and Balance in Women. J Strength Cond Res.17(4):721-5. 2003 (level of evidence 1B)
- ↑ 43.0 43.1 Mirza SK, Deyo RA. Systematic Review of Randomized Trials Comparing Lumbar Fusion Surgery to Nonoperative Care for Treatment of Chronic Back Pain. Spine 2007; 32(7): 816-823
- ↑ Extremiteiten, www.fysio.net, Extensieoefening voor de lumbale wervelkolom in buikligging, 29-10-2009fckLR(http://www.youtube.com/watch?v=SNamjanZttM&feature=youtube_gdata) LEVEL OF EVIDENCE 5
- ↑ Kielbaso J., Hardcore abs training, Fit4Less4Info, 19oktober2012fckLR(http://fit4lessamsterdam.wordpress.com/2012/10/) (http://fit4lessamsterdam.files.wordpress.com/2012/10/crunchleg-raise.jpg) LEVEL OF EVIDENCE 5
- ↑ Canbay S., et al, Posterior dynamic stabilization for the treatment of patients with lumbar degenerative disc disease: long-term clinical and radiological results, Turkish Neurosurgery 2013, vol. 23, No. 2, 188-197 (level of evidence 2)
- ↑ Adams MA, Stefanakis M, Dolan P. Healing of a painful intervertebral discfckLRshould not be confused with reversing disc degeneration: implications forfckLRphysical therapies for discogenic back pain. Clin Biomech (Bristol, Avon). 2010fckLRDec;25(10):961-71. (level of evidence 2B)
- ↑ Ip D, Fu NY. Can intractable discogenic back pain be managed by low-level laser therapy without recourse to operative intervention? J Pain Res. 2015 May 26;8:253-6 (level of evidence: 1B)