Deep Brain Stimulation
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Joseph Ayotunde Aderonmu and Pacifique Dusabeyezu
Introduction[edit | edit source]
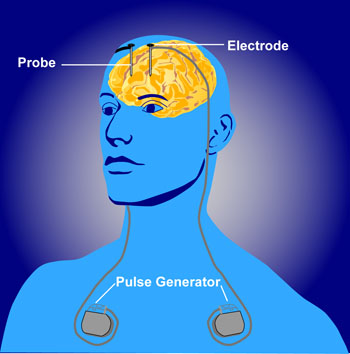
DBS involves the placement of electrodes into deep brain structures. Current is administered through these electrodes by an implanted power pack, which can be remotely controlled by the subject and adjusted by physicians. In essence, DBS is like a pacemaker for the brain[1].
Deep brain stimulation (DBS) is used in a variety of clinical settings, predominantly in patients with poorly controlled movement disorders. Although effective, its exact mode of function continues to be poorly understood[2] .
DBS is designed to alter the function of circuits in the brain. It has been used with varying degrees of success in the treatment of Parkinson’s disease, dystonia, epilepsy, obsessive-compulsive disorder and even depression.
Careful patient selection and target selection are essential if the procedure is to have good efficacy[2].
Anatomy[edit | edit source]
The DBS apparatus consists of electrodes implanted adjacent to specific deep brain structures, which are then connected to a pacemaker-like machine (pulse generator) that is implanted on the chest wall, via a subcutaneous wire. Stimulation parameters are then relayed by a computer to the pulse generator, appropriating proper amplitudes, frequencies, and pulse width. Common structures targeted by DBS include the subthalamic nucleus (STN), globus pallidus interna (GPi), and the ventral intermediate nucleus of the thalamus (VIM).
The precise mechanism of the resultant therapeutic effects of deep brain stimulation remains unclear. Imaging and physiologic studies corroborate the hypothesis that the ultimate effect of deep brain stimulation is the increase of the firing of the targeted neurons.[3]
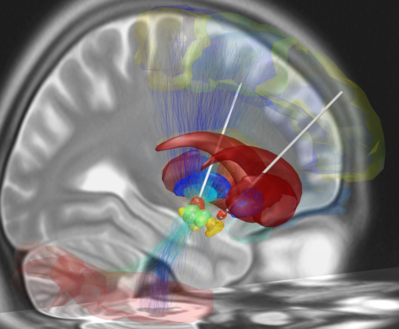
Image 2: Depicted is a reconstruction of bihemispheric DBS electrodes that have been surgically placed into the most common target structure for treatment of Parkinson's Disease, the subthalamic nucleus (orange). Other subcortical structures include the red nucleus (green), the substantia nigra (yellow), the internal (cyan) and external (blue) pallidum and the striatum (red). A stimulation volume is modeled by applying 2V (at 1000Ω impedance) to the second-uppermost contact of the left electrode. Structural fibertracts traversing through this volume are visualized and cortical regions that they connect with the stimulation volume are selected from an automatic anatomical labeling atlas and visualized.
Indications[edit | edit source]
- subthalamic nucleus
- pedunculopontine nucleus
- globus pallidus (pars interna)
- Severe essential tremor
- ventral intermediate nucleus
2. Dystonia (cervical dystonia and tardive dystonia)
- globus pallidus (pars interna)
- Cluster headaches
- hypothalamus
3. Chronic pain
- thalamus
- periaqueductal grey matter
4. Neuropsychiatric disorders: largely experimental[2]
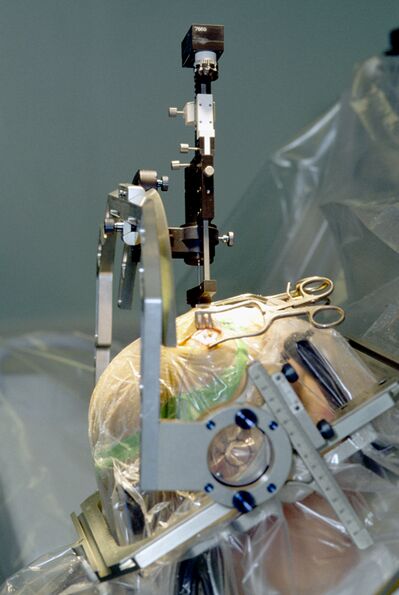
Image 3: Stereotactic procedure for inserting an electrode for deep brain stimulation in a patient with Parkinson's disease.
Significance[edit | edit source]
DBS has the potential for many applications, and has specifically been heralded as offering "a new life for people with Parkinson disease."
- DBS has already been awarded FDA approval for essential tremor, dystonia, Parkinson disease, and treatment-refractory obsessive-compulsive disease. Ongoing studies are investigating the possible off-label use in addiction, autism, anorexia nervosa, anxiety disorders, and schizophrenia[3].
- DBS has been a life-restoring therapeutic technique for thousands of patients with Parkinson’s disease with severely impaired motor and cognitive function, and it promises to dramatically improve the lives of people suffering from some other psychological and neurological disorders, including obsessive compulsive disorder, treatment-resistant depression, and Tourette’s syndrome.
- DBS can in seconds restore normal function to a person virtually paralyzed by a dopamine deficiency, contorted by uncontrollable tremor and muscular contraction. The transformation is miraculous. However, stimulation may result in unanticipated side-effects, altering mood, preferences, desires, emotion or cognition. .[1]
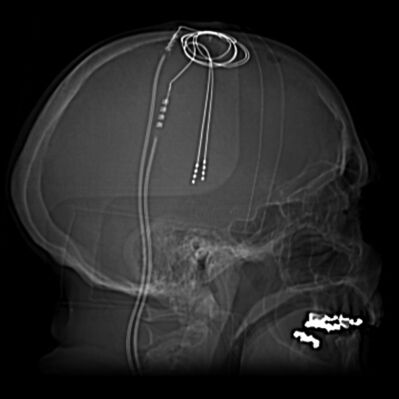
Image 4: Scout and CT images demonstrate bilateral deep brain stimulation electrodes extending to the region of the subthalamic nuclei. NB Scout is an preliminary film taken of a body region before a definitive imaging study–eg, an SF of the chest before a CT; 'scouts' serve to establish a baseline and are used before angiography, CT, MRI
With neurodegenerative movement disorders like Parkinson’s disease, the ability to deliver the right dose of stimulation where it is needed can make a remarkable difference in controlling an individual patient’s symptoms.
The latest DBSs (an upgrade to earlier systems available for years in both the U.S. and Europe) is approved as an add-on treatment for levodopa-responsive Parkinson’s patients, for whom levodopa alone is insufficient. It is approved for stimulation of both sides of the subthalamic nucleus and the internal globus pallidus, which are brain regions that play key roles in motor function.
Newest DBS system[edit | edit source]
The new DBS System’s pulse generator stimulates the brain with a pre-determined program of mild electrical impulses.
- The new device is based on cochlear implant technology, which precisely stimulates auditory nerves to replicate hearing. Earlier models, in contrast, rely upon pacemaker technology.
- Using Bluetooth wireless technology, individual DBS stimulation programs can be fine-tuned and adjusted as needed, to address changes in symptoms that occur throughout Parkinson’s progression by targeting different brain regions. In this way, physicians and patients can work together to better optimize therapy for each individual[4].
It is estimated that 208,000 deep brain stimulation (DBS) devices have been implanted to address neurological and neuropsychiatric disorders worldwide[5]
References[edit | edit source]
- ↑ 1.0 1.1 The Conversation Do brain interventions to treat disease change the essence of who we are? Available from: https://theconversation.com/do-brain-interventions-to-treat-disease-change-the-essence-of-who-we-are-45943 (accessed 19.5.2021)
- ↑ 2.0 2.1 2.2 Radiopedia Deep Brain Stimulation Available from: https://radiopaedia.org/articles/deep-brain-stimulation(accessed 19.5.2021)
- ↑ 3.0 3.1 Fariba K, Gupta V. Deep Brain Stimulation. StatPearls [Internet]. 2020 May 17.Available from: https://www.ncbi.nlm.nih.gov/books/NBK557847/ (accessed 19.5.2021)
- ↑ PD news today First US Patient Receives New Vercise Genus Deep Brain Stimulation Device Available from:https://parkinsonsnewstoday.com/2021/02/23/first-vercise-genus-deep-brain-stimulation-device-parkinsons-disease-implanted-us-patient/ (accessed 19.5.2021)
- ↑ Vedam-Mai V, Deisseroth K, Giordano J, Lazaro-Munoz G, Chiong W, Suthana N, Langevin JP, Gill J, Goodman W, Provenza NR, Halpern CH. Proceedings of the Eighth Annual Deep Brain Stimulation Think Tank: Advances in Optogenetics, Ethical Issues Affecting DBS Research, Neuromodulatory Approaches for Depression, Adaptive Neurostimulation, and Emerging DBS Technologies. Frontiers in Human Neuroscience. 2021 Apr 19;15:169.Available from: https://www.frontiersin.org/articles/10.3389/fnhum.2021.644593/full(accessed 19.5.2021)