Crohn's Disease
Original Editors - Sarah Bailey from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Sarah Bailey, Laura Ritchie, Lucinda hampton, Admin, Kim Jackson, Dave Pariser, Elaine Lonnemann, WikiSysop, Sehriban Ozmen, Wendy Walker, Manisha Shrestha and 127.0.0.1
Definition/Description[edit | edit source]
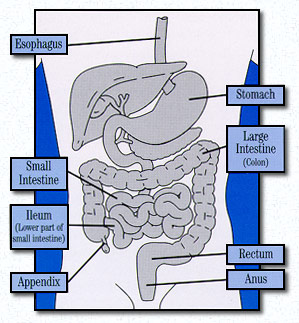
Crohn’s disease is a form of inflammatory bowel disease (IBD) that causes inflammation to the lining of the digestive or gastrointestinal (GI) tract [1] and may be a result of an immune system malfunction. The immune system sees the bacteria and organisms that lie within the GI tract and intestines and mistakes them for outside invaders to the body. In response to this, the body produces extra white blood cells to the GI tract to fight off the invaders, which creates inflammation within the lining of the tract. Chronic inflammation may result in ulcerations within the layers of the tract [2]. The inflammation can occur to any portion of the GI tract, from mouth to anus and can affect all layers of the intestinal tract while healthy bowel layers may be interspaced between the diseased portions of the bowel.[3]
The most commonly affected portion of GI tract affected is the lower portion of the small intestine, or ileum [1]. Due to the inflammation, abdominal pain, diarrhea and malnutrition can be a result [4]. Crohn’s disease is also referred to as granulomatous enteritis or colitis, ileitis, regional enteritis, or terminal ileitis. This disease is similar in some aspects to ulcerative colitis, but the difference lies in the fact that ulcerative colitis produces inflammation only within the colon or rectum while Crohn’s disease produces inflammation within the colon, rectum, small intestine, stomach, mouth and esophagus. The inflammation caused by Crohn’s disease has the potential to affect the deeper layers more than ulcerative colitis [5]. While these two conditions are very similar, approximately 10 percent of individuals are unable to pinpoint whether the disease process is ulcerative colitis or Crohn’s disease. For these individuals, they are then diagnosed with indeterminate colitis [6].
Prevalence[edit | edit source]
Crohn’s disease affects approximately 500,000 to two million people in the United States, equally affecting men and women [5]. This disease may occur in individuals of all age, but has characteristically affected adolescents and young adults between 15-35 of age. It is estimated that 10 percent of individuals affected are under the age of 18. Crohn’s has been found to affect American Jews of European descent four to five times more than the general population. The prevalence among whites is 149 per 100,000 with a steady increase in incidence among African Americans. Hispanics and Asian have a lower prevalence than do African Americans and whites. There has been a potential link between living environment and the incidence of Crohn’s disease, where there are more reports amongst urban and northern climates than rural and southern climates. Similarly, this disease tends to be more predominant in the US and Europe [6].
Characteristics/Clinical Presentation[edit | edit source]
There is no cure for this condition and Crohn’s disease alters between periods of remission and relapse. Crohn’s typically appears around adolescence and early adulthood and there is potential of Crohn’s disease to run in families [5]. About 20-25% of individuals affected with Crohn’s disease have a close relative who is affected with ulcerative colitis or Crohn’s disease. If an individual has a relative with Crohn’s, the risk of this individual is 10 times higher than the general population, while a brother or sister link increases the risk to 30 times higher than the general population. Current researchers have identified an abnormal genetic mutation on gene NOD2/CARD 15 which reduces the ability of the body to distinguish harmful bacteria. This mutation is found twice as often in individuals affected with Crohn’s versus the general population [6].
| [7] |
Symptoms of Crohn’s Disease[edit | edit source]
While Crohn’s is a chronic disease, the patients will experience bouts of flare ups and remission with the absence of symptoms [6]. About 50% of individuals with Crohn’s Disease will have mild symptoms. The other half may experience more severe symptoms and pain that appears to come and go. These patients undergo painful exacerbations and potentially symptom free remissions. The remissions might last for months to years but the symptoms will eventually return[6]. This unpredictable nature is part of what makes Crohn's so complicating. Typical symptoms include:
- Diarrhea
- Abdominal cramping generally in the right lower quadrant [1]
- Fever
- Potential rectal bleeding. The rectal bleeding is potentially due to tears or fissures within the anus lining.
- Fistulas or tunnels leading from the intestines to the bladder, vagina or skin may also occur, while most occur around the anal area. The fistula has potential to produce drainage, pus, mucus or stool being excreted from the opening. These symptoms may vary between individuals and may not all be present at the same time.
- Weight loss
- Fatigue [6]
- Perianal lesions
- Stunted growth in children
- Extraintestinal manifestations [8]
Types of Crohn's Disease[edit | edit source]
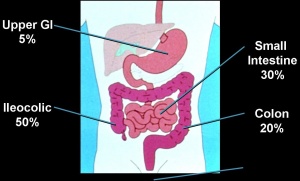
There are different types of Crohn’s Disease dependent upon the location and disease pattern within the GI tract. The different locations of Crohn’s Disease include:
Gastroduodenal Crohn’s Disease[edit | edit source]
Located in the upper gastrointenstinal tract and affects the stomach and first part of the small intestine (duodenum). This is uncommon and symptoms occur in 5% of those diagnosed with Crohn’s. Associated symptoms include:
- Nausea
- Loss of appetite
- Weight loss
- Vomiting
- Pain in upper abdomen
Jejunoileitis[edit | edit source]
This is also uncommon in the general population of those diagnosed with Crohn’s disease. Inflammation is located in the Jejunum or Second part of small intestines. Associated symptoms include:
- Diarrhoea
- Abdominal pain (after eating)
- Malnutrition due to malabsoprtion of nutrients
- Weight loss
Ileitis[edit | edit source]
Inflammation located in the last part of small intestine or ileum and affects 30% of individuals diagnosed with Crohn’s disease. Associated symptoms include:
- Diarrhoea
Ileocolitis[edit | edit source]
This is the most common form of Crohn’s disease and affects 50% of those diagnosed with inflammation located in the ileum and colon. Associated symptoms include:
- Diarrhoea
- Abdominal pain (right lower quadrant)
- Weight loss
Crohn’s Colitis[edit | edit source]
This affects 20% of individuals diagnosed with Crohn’s disease with inflammation located in the colon. The perianal disease and extraintestinal complications are more commonly associated in these individuals. Associated symptoms include:
- Diarrhoea
- Rectal bleeding
- Abdominal pain
Perianal Disease[edit | edit source]
This occurs in 1/3 of individuals diagnosed with Crohn’s disease. These individuals can have fistulae, fissures, abscesses or skin tags (fleshy growths outside the anus) [8]
Associated Co-morbidities[edit | edit source]
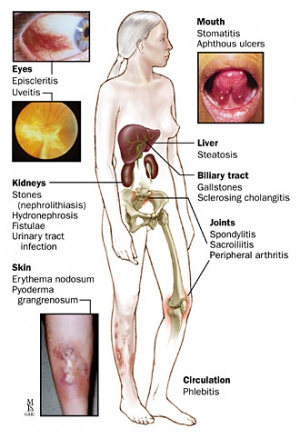
While commonly Crohn’s disease affects the GI tract, there have been instances where additional complications include arthritis, skin conditions, inflammation of the eyes and/or mouth, joints, kidney stones, gallstones and liver/biliary conditions were also reported. The most common associated comorbidity is a blockage of the intestines. Continual blockage tends to thicken the walls of the intestine with scar tissue which further reduces the size of the passageway [1]. Fistulas are also common due to sores or ulcers that develop into deep ulcers or tracts connecting[6] into the bladder, vagina, skin or anal area. These fistulas are then exposed to infection[1].
It has been discovered that individuals with Crohn’s disease have referred pain to the low back. Approximately 25% of individuals with Crohn’s and/or irritable bowel disease have sacroilitis, polyarthritis, monarthritis of ankle, knee, elbows and/or wrists [10], as well as migratory arthralgias. At times, these joint conditions may even present initially before the other GI related symptoms[11].
Since this disease affects the absorption of nutrients, chronically involved individuals commonly have deficiencies of protein, calories and vitamins. This may be due to the malabsorption or overall inadequate dietary intake secondary to the patient’s attempt to limit the pain produced with eating [1].
There is a risk of colorectal cancer that tends to increase with an increased length of time with the disease. There is a 2% incidence of colorectal cancer after 10 years diagnosis, 9% incidence after 20 years diagnosis, and 19% incidence after 30 years of diagnosis of Crohn’s disease. A 20% mortality rate lies within the first 10 years of diagnosis in the presence of complications. Surgical removal of the Crohn’s bowel does not prevent colorectal cancer, thus putting importance on prevention and screening for early detection of colorectal cancer[11].
Osteopenia can occur in 50% of patients diagnosed with Crohn’s Disease and osteoporosis can occur in 15% of those diagnosed. It is thought these complications may be due to the steroid therapy , smokers, those with a more active disease as well as those individuals with low calcium and vitamin D intake. Due to this, all patients diagnosed with Crohn’s Disease should be informed of this potential complication and should be advised to take supplemental calcium and vitamin D.
Stones of the kidney and gallbladder are potential comorbidities. Kidney stones may occur due to the fat malabsorption and diarrhea in individuals with Crohn’s Disease. These patients may experience extreme flank or lower lateral back pain as well as blood in the urine. Gallstones may occur due to the bile acid malabsoprtion. These patients may experience right sided abdominal pain[8].
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
The diagnosis of Crohn’s disease is made by ruling out other potential causes to explain the patient’s signs and symptoms. Some of the tests include blood tests, fecal occult blood test (FOBT), colonoscopy, flexible sigmoidoscopy, barium enema or small bowel imaging, CT of the GI tract, or a capsule endoscopy.
The blood tests are used to check for anemia[4] which would indicate inflammation within the body[1], infection, and antibodies that might be present with individuals with inflammatory bowel disease.
The FOBT assesses an individual’s stool sample for the presence of blood.
A colonoscopy allows the doctor to take a biopsy or tissue sample to determine if there is a presence of any granulomas which are common with Crohn’s disease and not ulcerative colitis.
The flexible sigmoidoscopy allows the doctor to assess the last portion of the colon for any biopsy samples[4]. This allows the doctor to determine if there is any inflammation or bleeding amongst the intestines[1].
Barium enemas allow the doctors to assess the intestines via x-ray. The barium coats the inner lining of the GI tract to allow the lining to be visible on the x-ray.
A CT of the GI tract allows a quick look at the entire bowel in a way that cannot be seen in other diagnostic tests. This helps to assess for blockages, abscesses or fistulas.
The capsule endoscopy consists of a capsule with a small camera inside that is swallowed by the individual. The camera takes pictures every second as it travels along your GI tract. The pictures are then sent to a wireless computer belt worn by the patient that can then be taken into the doctor and downloaded for view[4].
Causes[edit | edit source]
The initial cause of Crohn’s disease is unknown, but was previously thought to be caused by a person’s stress and diet. Now, it is believed that factors such as these are just aggravating components while hereditary and a malfunctioning immune system may be a part of the development of Crohn’s disease. The immunological explanation believes that immune system attempts to fight off organisms while inflaming the GI tract. In those affected with Crohn’s disease, there may be an abnormal response to the bacteria that produces the large extent of inflammation. The hereditary explanation believes there is a genetic mutation that has been found in those individuals affected with Crohn’s. Crohn’s disease produces small, shallow, scattered and crater-like erosion along the inner surface of the GI tract. As this disease progresses, the erosions become deeper and larger ulcerations that will eventually scar and create stiffness along the tract. With this stiffness, the bowel can easily become obstructed. Along the deep ulcerations, the bacterium that travels along the GI tract is diffused into adjacent organs and abdominal cavity[5].
Some research has indicated that Crohn’s disease is very similar to a condition called Johne’s disease that occurs in cattle. The difference between the two is that Johne’s disease has a known etiology which is a bacterium called Mycobacterium avium subspecies paratuberculosis or MAP. It is believed that MAP’s presence in the intestines of individuals with Crohn’s disease could be a common characteristic. It is believed that the MAP comes from the pasteurized milk consumed from cows that are infected with Johne’s disease. The pasteurization does not remove this organism and potentially is reasoning for the connection. Individuals with Crohn’s disease do not have high amounts of MAP, so the direct cause of inflammation is still unknown if the bacterium directly influences the inflammation. Some theorize that the elimination of MAP may help to improve Crohn’s disease[12].
Systemic Involvement[edit | edit source]
Crohn’s disease may have extraintestinal symptoms, or symptoms that occur outside of the intestines. This can occur in up to 25% of patients diagnosed with Crohn’s Disease. These can include any or all of the following:
Musculoskeletal[edit | edit source]
- Osteoporosis
- Arthritis (most commonly peripheral joints)
- Low back pain[6]
Integumentary[edit | edit source]
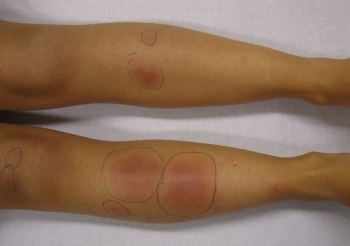
- Erythema nodosum or painful red bumps on the skin surface
- Pyoderma gangrenosum or skin ulcerations [8]
Genitourinary[edit | edit source]
- Kidney stones
- Liver involvement:
Oral[edit | edit source]
- Sores within the mouth
Ophthalamic[edit | edit source]
- Redness and itching of the eyes
- uveitis, eye pain and/or vision changes
Psychiatric[edit | edit source]
- Emotional distress [6]
Medical Management[edit | edit source]
The main goal of medical therapy is to better regulate the patient’s immune system[6]. Additional goals for treatment in Crohn’s Disease include: inducing remission, maintain remission, improve the patient’s quality of life and minimize toxicity. The specific treatment of Crohn’s Disease is dependent upon several factors, including the location, severity of disease, type of disease, complications of Crohn’s and the individual’s response to prior medical treatments. There is a current “step up” therapy that is used for individuals with Crohn’s disease.
This approach involves:
- Patients first treated with medications with fewer side effects that may not be as effective as the stronger medications
- As the disease progresses, the treatment becomes more intense involving medications that are more powerful with potentially more toxicity levels[8].
Medications[edit | edit source]
There are a few classifications of drugs that can be used to help relieve the symptoms of Crohn’s disease. These include anti-inflammatory, cortisone or steroids, immune system suppressors, Infliximab (Remicade), antibiotics and anti-diarrheal/fluid replacements.
Anti-inflammatory drugs are generally the initial step in relieving the symptoms, which can include Sulfasalazine, which is better for conditions within the colon[4] and is the most common. An additional type includes 5-ASA agents such as Mesalamine which has fewer side effects but is not as effective at treating the small intestine[1].
Cortisone or corticosteroids can be very effective by reducing inflammation within the body, but their side effects are vast including night sweats, high blood pressure, osteoporosis, bone fractures, excessive facial hair, increased susceptibility for infection and cataracts[4]. Prednisone is typically prescribed when the disease is beginning and typically worse[1].
Immune system suppressors suppress the immune system which targets the immune system to reduce the inflammation within the body. Some types include Imuran or Azathioprine and Purinethol which are the most commonly used for IBD and conditions. These may also help to heal the fistulas [4]. It should be noted that the use of immunosuppressive drugs may increase the effectiveness of corticosteroids[1].
Infliximab (Remicade) is the first medication to block the inflammation response by the body. This was approved by the FDA for the treatment of moderate to severe Crohn’s disease that has failed to respond to prior conservative treatments. This medication is an anti-TNF substance or anti-tumor necrosis factor[1] and neutralizes this protein that is produced by the immune system. The TNF is targeted and removed before there is the chance for inflammation to occur in the GI tract. The FDA has declared a warning to children and adolescents taking this medication or other TNF inhibitors are at an increased risk for developing cancer[4][13].
Antibioticsare used to treat and heal fistulas and abscesses associated with Crohn’s disease. Medications such as these may also reduce the amount of harmful bacteria within the GI tract that suppresses the intestinal immune system. Common antibiotics include Flagyl and Cipro.
Additional medications that are used to help relieve symptoms in individuals with Crohn’s disease include: anti-diarrheals to relieve the diarrhea, laxatives, pain relievers, iron supplements, vitamin B-12 shots, calcium and vitamin D. Nutrition supplements are also very important, especially in children whose growth may be slowed. This nutrition might be in the form of high-calorie liquid formulas, feedings tube or parenteral nutrition injected into the vein. This will help to overall improve the nutrition of the individual and allow their bowel to rest which may reduce inflammation for a short period of time[4].
It is estimated that 2/3 of individuals affected with Crohn’s will need surgery at some point within their lives. This becomes a necessary treatment plan when medications and conservative treatment has failed. The surgery is used either to relieve the symptoms or correct complications secondary to perforation, abscess, blockage, or bleeding into the intestines. The surgery can often times improve the symptoms but may never treat or heal the condition. Crohn’s disease often reoccurs after surgery, so the benefits and complications should be weighed appropriately by the patient when choosing the course of action[1].
Surgical Intervention[edit | edit source]
Some indications for surgery include:
- Perforation of intestines
- Fistula that cannot be medically managed
- Abcess
- Uncontrollable bleeding from intestine
- Cancer or precancer
- Toxic magacolon – a potentially lethal form of acute colitis
- Failure of medical therapy
There are multiple surgical processes that can be used for individuals with Crohn’s Disease. These include:
- Bowel resection in which the affected parts of the intestines are removed and the healthier portions are then reattached.
- Proctocolectomy and Ostomy where the individual may need the whole colon and rectum removed. These patients will need a stoma where the stool can then exit the body via pouch or bag.
- Stricturoplasty is the removal of the strictures or scarred narrowing of the intestines. This will widen the portions and will allow intestinal contents to pass through[8].
Physical Therapy Management[edit | edit source]
Crohn’s disease is associated with periumbilical pain and referred low back pain. Individuals may also experience pain in the lower right quadrant and potential associated iliopsoas abscess due to an inflammatory mass that may create hip, buttock, thigh, or knee pain. When a patient presents to physical therapy with unknown origin of low back, sacroiliac or hip pain, it is vital for the therapist to screen for potential organic sources of the pain and is even more important in patients with a history of inflammatory bowel disease.
Since individuals with Crohn’s disease might also have associated low bone mineral content and a high potential for osteoporosis, it is important for the therapist to provide education on osteoporosis and its prevention.
Hydration is very important in patient’s with Crohn’s disease so the therapist should be aware of signs of dehydration, including headache, dry lips, brittle nails and hair, dry hands and disorientation.
Due to the complexity of Crohn’s Disease, patients might be predisposed to emotional stress that could exacerbate the prior symptoms. In knowing this, the therapist has the availability to accept the patient’s feelings, validate the disease to the patient as well as prescribing an exercise program to better the outcome for the patient. These exercises have the ability to boost the immune system, reduce depression, and improve the body image of the patient. In addition to providing this exercise program, therapists can better create coping mechanisms as well as techniques to manage the unexpectedness of Crohn’s Disease[11].
Outcome Measures[edit | edit source]
An outcome measure has been created to track the progress or lack of progress for individuals affected with Crohn’s disease called Crohn’s Disease Activity Index (CDAI). A score below 150 indicates a better prognosis than higher scores. This measure helps to track an individual’s progress from week to week to determine if the symptoms are better or worse. This is more of a gauge of progress and not a prognosis tool[14].
Dietary Management[edit | edit source]
An elemental diet that includes food broken down into basic components like amino acids, vitamins, sugars, etc can help improve the symptoms associated with Crohn’s disease. There has also been improvements found in individuals who are placed on diets free of dairy, gluten and yeast products. Herbs have also been studied to determine effectiveness of relief of symptoms.
Additional ways to better manage the symptoms may include changes to your diet. Some key points include:
- Eating smaller meals and at more frequent intervals
- Reducing the amount of greasy, fatty foods that may produce diarrhoea and gas
- Limit consumption of milk and dairy products
- Reduce the amount of carbohydrates that are poorly digested that may cause diarrhoea, gas, bloating, cramps
- Restrict the intake of high-fiber foods such as nuts, seeds, corn, and popcorn[6].
Differential Diagnosis[edit | edit source]
The symptoms above are not specific to Crohn’s disease and have potential to be seen in other conditions. Differential diagnoses can include the following:
- Infectious causes – bacterial, viral, or parasitic infection.
- Ischemia – low blood flow to the small intestine or colon, usually seen in older patients
- Medication – non-steroidal anti-inflammatories, antibiotics, birth control pills
- Diverticulitis – infection of a diverticulum (outpouching of colon) that can present with left lower quadrant pain and fever
- Appendicitis – usually presents with right lower quadrant abdominal pain and fever
- Irritable bowel syndrome – can cause severe diarrhea and abdominal pain
- Lactose intolerance – can cause diarrhea, bloating, and abdominal pain. Patients with Crohn’s disease can also have lactose intolerance.
- Celiac disease – sensitivity to gluten (wheat) which can cause diarrhea and bloating.
- Gallstones
- Cancer, lymphoma
- Diseases that affect other organs in the abdomen also need to be considered such as:
- Endometriosis, pelvic inflammatory disease, ectopic pregnancy, ruptured ovarian cyst
- Kidney stones, bladder or kidney infections[8]
Case Reports[edit | edit source]
- Crohn's Disease Case Study
- Barlow S. Case study: A 16 year old male with bone density losses resulting from Crohn's disease. Synergy [serial online]. January 2003;21. Available from: ProQuest Nursing & Allied Health Source. Accessed April 6, 2010, Document ID: 347682641. Case study:A 16 year old male with bone density losses resulting from Crohn's disease
- Arumugam R, Brandt ML, Jaksic T, Gilger M. Crohn's disease presenting as chronic constipation: A case report. Clinical Pediatrics [serial online]. 2000;39:369-71. Available from: Health Module. Accessed April 6, 2010, Document ID: 55518839. Crohn's disease presenting as chronic constipation: A case report
- Holaday M, Smith KE, Robertson S, Dallas J. An atypical eating disorder with Crohn's disease in a fifteen-year-old male: A case study. Adolescence [serial online]. 1994;29:865-73. Available from: Research Library Core. Accessed April 6, 2010, Document ID: 1499994.An atypical eating disorder with Crohn's disease in a fifteen-year-old male: A case study
- Ogram AE, Sobanko JF, Nigra TP. Metastatic cutaneous Crohn's disease of the face: a case report and review of the literature. Cutis. 2010;85:25-7. Available from: Pubmed. Acessed April 6, 2010. Metastatic cutaneous Crohn's disease of the face: a case report and review of the literature
Resources[edit | edit source]
Crohn's & Colitis Foundation of America: Crohn's & Colitis Foundation of America
Living with Crohn's Disease: Living with Crohn's Disease
National Digestive Diseases Information Clearinghouse (NDDIC): Crohn's Disease
CDAI Calculator: Crohn's Disease Activity Index Calculator
Presentations[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 National Digestive Diseases Information Clearinghouse (NDDIC). Crohn’s disease. http://digestive.niddk.nih.gov/ddiseases/pubs/crohns/ (accessed 4 March 2010).
- ↑ Living with Crohn’s Disease. Inside Crohn’s disease. https://www.livingwithcrohnsdisease.com/livingwithcrohnsdisease/crohns_disease/inside_crohns.html (accessed 4 March 2010)
- ↑ Crohn's Disease Answers. What is Crohn's Disease. http://crohnsdiseaseanswers.com/1.-what-is-crohns-disease-what-is-crohns-disease.HTM (accessed 5 April 2010).
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 MayoClinic. Crohn’s Disease. http://mayoclinic.com/health/crohns-disease/DS00104/DSECTION=causes (accessed 4 March 2010)
- ↑ 5.0 5.1 5.2 5.3 MedicineNet. Crohn’s Disease. http://www.medicinenet.com/crohns_disease/page2.htm (accessed 4 March 2010)
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 Crohn’s and Colitis Foundation of America (CCFA). About Crohn’s Disease. http://ccfa.org/info/about/crohns (accessed 4 March 2010)
- ↑ Thomas Craig. A Frank discussion on Crohn's Disease. Available at http://www.youtube.com/watch?v=Npda8xr2G-Y (last accessed 4/510)
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 Cheifetz Adam, Moss Alan, Peppercorn Mark. Crohn’s Disease. Knol Beta. Available at http://knol.google.com/k/crohn-s-disease#. Accessed 5 April 2010.
- ↑ Crohn’s Disease: Introduction. John Hopkins Medicine. Available at http://www.hopkins-gi.org/GDL_Disease.aspx?CurrentUDV=31&GDL_Disease_ID=291F2209-F8A9-4011-8094-11EC9BF3100E&GDL_DC_ID=D03119D7-57A3-4890-A717-CF1E7426C8BA (accessed 5 April 2010).
- ↑ Goodman CC, Snyder TEK. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th ed. St. Louis, MO: Saunders-Elsevier; 2007
- ↑ 11.0 11.1 11.2 Goodman CC, Fuller KS. Pathophysiology: Implications for the Physical Therapist. 3rd ed. St. Louis, MO: Saunders-Elsevier; 2009.
- ↑ Bone K. Using Herbs and Diet to Beat Crohn’s Disease. Dynamic Chiropractic. 2008;4(2) 26-27.
- ↑ Susman E.. SONIC gives boost to infliximab for Crohn's. Medical Post [serial online]. November 2008;44:14. Available from: Health Module. Accessed March 4, 2010, Document ID: 1616171171.
- ↑ Crohn’s Disease Activity Index (CDAI) calculator. CDAI Online Calculator. <ref="http://www.ibdjohn.com/cdai/"Crohn's Disease Activity Index, CDAI (accessed 4 March 2010)