Coronary Artery Disease (CAD)
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton and Kim Jackson
Introduction[edit | edit source]
Coronary artery disease (CAD) is the most common form of heart disease. It is the result of atheromatous changes in the vessels supplying the heart. CAD is used to describe a range of clinical disorders from asymptomatic atherosclerosis and stable angina to acute coronary syndrome (unstable angina, NSTEMI, STEMI). NB for terminology used see end of article.
- CAD is asymptomatic in most of the population. When severe enough it can cause angina or an acute coronary syndrome including myocardial infarction. CAD may also present with heart failure or sudden cardiac death.
- In the US, it is still one of the leading causes of mortality. Initial evaluation of risk factors is the first step in the prevention of CAD[1]
- CAD epidemic peaked in the 1960s. Since that time age-adjusted mortality declined steadily in the United States and many other industrialized countries1. Hospitalization for CAD also fell, particularly in the past two decades with CAD severity decreasing as NSTEMIs increased, indicating milder forms of CAD. Also lifestyle factors and associated risk factors improved such as smoking, hypertension and cholesterol.[2]
Etiology[edit | edit source]
Risk factors of coronary artery disease are as follows:
Non-Modifiable
- Age
- Gender
- Race
- Family history
Modifiable
- Type 2 diabetes mellitus
- Hypertension
- Smoking
- Hyperlipidemia
- Chronic kidney disease
- Obesity and metabolic syndrome
Risk enhancing factors
- Premature menopause
- Preeclampsia
- Chronic inflammatory conditions (for example rheumatoid arthritis, HIV, psoriasis)
- Persistently elevated triglycerides[1]
Epidemiology[edit | edit source]
Coronary artery disease is a leading cause of death worldwide. The World Health Organization (WHO) reported that CAD was responsible for approximately nine million deaths in 2016.
Developed and developing countries show opposite trends in mortality due to CAD.
- Developed countries: Although death rates from CAD have decreased in most high- and middle-income countries in the past 2 decades, there are worrying signs of a lessening trend in the United States (dramatic increases of world-wide obesity and diabetes mellitus1 prevalences emphasize the need for improved preventive and therapeutic strategies to battle these major public health problems).[3]
- Developing countries; status of CAD in is worsening with increasing trends of mortality[1].
Increased implementation of primary and secondary prevention methods of cardiovascular disease is responsible for the decline in mortality in developed countries.
- Primary prevention methods are intended to prevent cardiovascular events for people with high risks but no previous history.
- Secondary prevention methods are therapies that prevent any further cardiac damage to those with a history of CAD[1].
Pathology[edit | edit source]
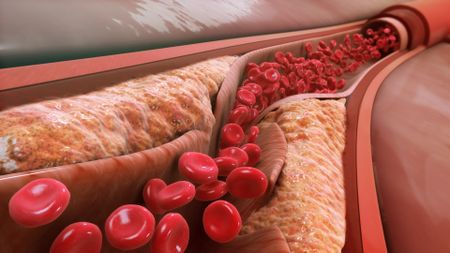
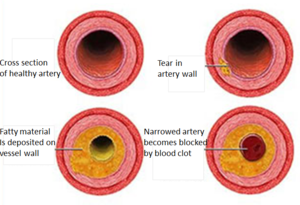
CAD is primarily due to atherosclerosis, an inflammatory process that leads to atheroma development and remodelling/stenosis of the coronary arteries. Image at R: As atheroma enlarges, the arterial wall ruptures and releases blood clots that lead to narrowing of the artery.
- A stenosis of >50% of diameter or >75% cross-section diameter reduction can lead to angina.
- Thrombus formation after plaque disruption can lead to acute coronary syndrome[2]
Evolving plaque Complications:
- Thin cap or large lipid atheroma (greater than 40% of plaque volume) increases the chances of coronary plaque disruption followed by thrombotic occlusion plaque
- Thrombus in the lumen caused by endothelial erosion
- Intra-plaque hemorrhage causing expansion of plaque volume
- Lumen thrombus caused by protruding calcific nodules from complex fibro–lipid–calcific architecture and calcified shell[1]
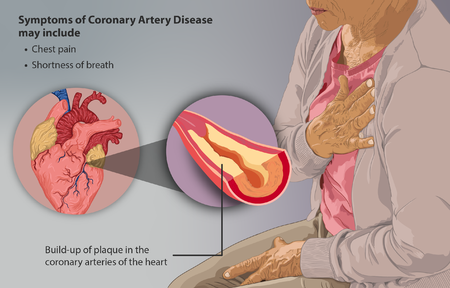
Signs and Symptoms[edit | edit source]
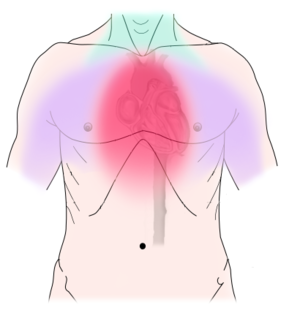
An acute coronary event, such as a heart attack, may cause the following symptoms:
- Angina, which can feel like pressure, squeezing, burning, or tightness during physical activity. The pain or discomfort usually starts behind the breastbone, but it can also occur in the arms, shoulders, jaw, throat, or back. The pain may feel like indigestion.
- Cold sweats
- Dizziness
- Light-headedness
- Nausea or a feeling of indigestion
- Neck pain
- Shortness of breath, especially with activity
- Sleep disturbances
- Weakness
Image R: Diagram of discomfort caused by coronary artery disease. Pressure, fullness, squeezing or pain in the center of the chest. Can also feel discomfort in the neck, jaw, shoulder, back or arm
Women are somewhat less likely than men to experience chest pain. Instead, they are more likely to experience:
- Dizziness
- Fatigue
- Nausea
- Pressure or tightness in the chest
- Stomach pain
- Women are also more likely than men to have no symptoms of coronary heart disease.
Chronic (long-term) CAD can cause symptoms such as the following:
- Angina
- Shortness of breath with physical activity
- Fatigue
- Neck pain[4]
Diagnosis[edit | edit source]
Coronary artery disease diagnosis starts on medical and family histories, risk factors, and diagnostic tests.
Diagnostic Tests and Procedures
- Blood Tests to examine the level of fats, cholesterol, glucose, and proteins in the blood. Any abnormal levels may indicate risk factors for Coronary heart disease.
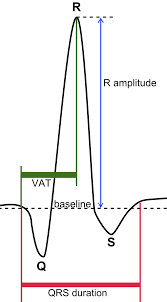
- EKG (Electrocardiogram) record hearts electrical pulses its strength and timing, helps to find previous or current heart attack and risk of Coronary heart disease.
- Chest X-ray is the picture of heart, lungs, and blood vessels. It helps to reveal indication of a hear failure.
- Computer tomography (CT) scans – produces images of the heart. It helps to identify hardening and narrowing of arteries.
- Stress Testing designed to find out if one or more of the coronary arteries feeding the heart contain plaques that block a blood vessel 70% or more[5].
- Other stress tests use a radioactive dyes, positron emission tomography, or cardiac magnetic resonance imaging (MRI) to get pictures of the heart during hard working and at rest.
- Coronary angiography
- Electron-Beam Computed Tomography measures calcium deposits in and around the coronary arteries. If more calcium detected, then more chances to have coronary heart disease. However, its accuracy is still not provable[6].
Treatment[edit | edit source]
Treatment of coronary artery disease depends upon the symptoms and clinical presentation of the patient.
It can range from medical management for controlling angina symptoms to acute intervention by coronary artery stenting.
- Patients, who present with unstable angina and NSTEMI, require urgent evaluation.
- If the patients present with STEMI, urgent revascularization is necessary, in addition to the initial stabilization.
- Patients with unstable angina and NSTEMI with significant risk factors, the decision should be made on whether cardiac catheterization is warranted based on risk assessment.
- On the other end of the spectrum, for patients who present as an outpatient with stable angina, the main goals of treatment are to help relieve the symptoms of the disease and prevent further complications associated with coronary artery disease.
Prevention plays a major role in the management of coronary artery disease.[1]
Primary Prevention[edit | edit source]
Early recognition of risk factors and primary prevention have significantly decreased the morbidity and mortality associated with CAD. Lifestyle modification with diet, exercise, and smoking cessation is crucial to reduce cardiovascular risk factors. Further control of hypertension, diabetes, and hyperlipidemia is essential to reduce the risk of CAD
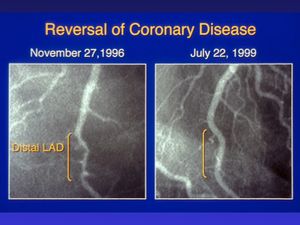
- Diet - Diet is a significant contributing factor to reduce the risk of coronary artery disease. According to ACC/AHA 2019, the plant-based Mediterranean diet (high in vegetables, fruits, legumes, nuts, whole grains, and fish) is highly recommended. Image R: Coronary angiograms of the distal left anterior descending artery before (left) and after (right) 32 months of a plant-based diet without cholesterol-lowering medication, showing profound improvement.
- Exercise, physical activity, and weight loss Physical activity is also equally beneficial for CAD risk reduction. At least 150 minutes per week of moderate-intensity activities and greater than 75 minutes a week of vigorous-intensity physical activities are helpful. Weight loss if BMI indicates a need.
- Tobacco Use - Using tobacco is among the leading causes of preventable deaths in the U.S. and also a significant risk factor of CAD.
- Hypertension management
- Non-pharmacological interventions are lifestyle modifications that include changes in diet and exercise.
- Weight loss also has a positive impact on lowering blood pressure.
- Reducing alcohol consumption also has blood-pressure-lowering effects.
- Type 2 Diabetes mellitus (DM) - Initially, dietary modifications using a heart-healthy diet (like Mediterranean and DASH diet as mentioned above) and physical activities (at least 150 minutes/week of moderate to vigorous) are encouraged. Weight loss is recommended if the individual is overweight or obese.
- Statin use - A moderate-intensity statin is recommended to any patient aged between 40 to 75 years with type 2 DM, regardless of cholesterol levels and ASCVD risk.
- Aspirin
Secondary Prevention[edit | edit source]
Secondary prevention is the therapy to prevent further damage and progression of the disease after the patient has a diagnosis of cardiovascular disease, including coronary artery, cerebrovascular, or peripheral arterial disease. The guidelines are somewhat similar to that of primary prevention, including diet, exercises, and smoking cessation as discussed above.
A large part of secondary prevention also includes pharmacological therapy. [1]
A favorable lifestyle is associated with around 40% reduced relative and 10-year cumulative risk of CAD across strata of non-modifiable risk factors, including age, gender, educational level and parental history of MI. This supports the usefulness of lifestyle-targeted CAD prevention among subgroups at higher non-modifiable risk within the overall healthy population[7].
Differential Diagnosis[edit | edit source]
Differential diagnosis is made based on the presenting signs and symptoms. Other conditions presenting as chest pain and mimicking CAD could be musculoskeletal pains, pleural inflammation, diaphragmatic symptoms, GERD, dysphagia, panic attacks, and neuralgia from neck and shoulder. A careful initial evaluation should be done with these differentials in mind as other non-cardiac causes, as mentioned above, could be the reason for the patient’s presentation.[1]
Physiotherapy[edit | edit source]
- Cardiovascular diseases are the leading cause of disability globally and despite the advances in clinical care and medicine, continue to be the principal cause of morbidity and mortality.
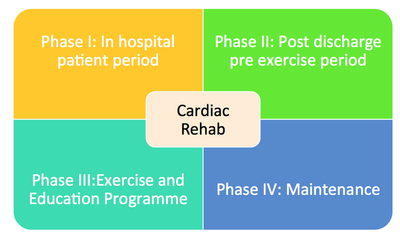
- Cardiac Rehabilitation is a complex intervention which requires the input of a multidisciplinary team to deliver the recommended seven core components.
- Physiotherapists have the appropriate training, knowledge and skills to deliver the exercise component of cardiac rehabilitation and help patients return to their activities of daily life.
- However, cardiac rehabilitation remains underutilized due to poor referral and enrollment post discharge. Evidence have demonstrated the beneficial role of physiotherapy in cardiac rehabilitation.[8]
For Physiotherapy intervention/techniques etc see
- Cardiac Rehabilitation
- Physical Activity and Cardiovascular Disease
- https://www.physiospot.com/research/exercise-prescription-in-patients-with-different-combinations-of-cardiovascular-disease-risk-factors/
Summary[edit | edit source]
CVD is a major cause of disability and premature death throughout the world.
- The underlying pathology of atherosclerosis develops over many years and is usually advanced by the time symptoms occur, generally in middle age.
- The risk of developing CAD increases with age, and includes age >45 years in men and >55 years in women.
- A family history of early heart disease is also a risk factor, such as heart disease in the father or a brother diagnosed before age 55 years and in the mother or a sister diagnosed before age 65 years.
- Acute coronary and cerebrovascular events frequently occur suddenly, and are often fatal before medical care can be given.
Many traditional risk factors for CAD are related to lifestyle
- Preventative treatment can be tailored to modifying specific factors. It is very important to know these risks to reduce disability and premature deaths from CAD[9]
Education and Exercise play an important preventative role in CAD treatment: Physiotherapists have the appropriate training, knowledge and skills to deliver the exercise component of cardiac rehabilitation and help patients return to their activities of daily life.
Terminology[edit | edit source]
Acute coronary syndrome - encompasses a spectrum of conditions which include unstable angina, and myocardial infarction with or without ST-segment elevation. Patients with different acute coronary syndromes may present similarly; definitive diagnosis is made on the basis of clinical presentation, ECG changes, and measurement of biochemical cardiac markers[10]
Unstable angina - A severe and dangerous form of ANGINA PECTORIS due to breakdown of atherosclerotic plaque in the coronary arteries and the formation of blood clot (thrombosis). There may also be coronary artery spasm from products derived from blood platelets. Pain becomes more frequent and prolonged and may occur at rest. The accurate predictability of pain in terms of its relation to a given amount of exertion is lost. The risk of a heart attack is high[11]. Partial or incomplete coronary occlusion[12]
STEMI - ST Elevation Myocardial Infarction is a very serious type of heart attack during which one of the heart’s major arteries (one of the arteries that supplies oxygen and nutrient-rich blood to the heart muscle) is blocked. ST-segment elevation is an abnormality detected on the 12-lead ECG[13]. Complete coronary occlusion
NSTEMI - stands for non-ST segment elevation myocardial infarction, which is a type of heart attack. Compared to the more common type of heart attack known as STEMI, an NSTEMI is typically less damaging to your heart. Partial or incomplete coronary occlusion.
ECG - Each heartbeat shows a visible waveform on an electrocardiogram. Although the clinical presentation and symptoms of NSTEMIs and STEMIs are the same, their waves look very different on an ECG[14].
CAD - also known as coronary heart disease (CHD), ischemic heart disease.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Regmi M, Siccardi MA. Coronary Artery Disease Prevention. InStatPearls [Internet] 2019 Sep 24. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK547760/ (last accessed 6.8.2020)
- ↑ 2.0 2.1 Luepker RV. Falling coronary heart disease rates: a better explanation?.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4768868/ (last accessed 6.8.2020)
- ↑ Quertermous T, Ingelsson E. Coronary artery disease and its risk factors: leveraging shared genetics to discover novel biology.Available from:https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.115.307937 (last accessed 7.8.2020)
- ↑ NIH CHD Available from:https://www.nhlbi.nih.gov/health-topics/coronary-heart-disease (last accessed 7.8.2020)
- ↑ Mayo clinic Stress test Available from:https://www.health.harvard.edu/heart-disease-overview/cardiac-exercise-stress-testing-what-it-can-and-cannot-tell-you (last accessed 9.8.2020)
- ↑ Healthy ojas CAD Available from:http://healthy-ojas.com/cholesterol/cad-diagnosis.html (last accessed 8.8.2020)
- ↑ Dimovski K, Orho-Melander M, Drake I. A favorable lifestyle lowers the risk of coronary artery disease consistently across strata of non-modifiable risk factors in a population-based cohort. BMC public health. 2019 Dec 1;19(1):1575. Available from:https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7948-x (last accessed 8.8.2020)
- ↑ Themistocleous, Irene-Chrysovalanto & Stefanakis, Manos & Douda, Helen. (2017). Coronary Heart Disease Part II: Role of Physiotherapy. The Journal of Physical Activity, Nutrition and Rehabilitation.Available from:https://www.researchgate.net/publication/316715625_Coronary_Heart_Disease_Part_II_Role_of_Physiotherapy/citation/download (last accessed 7.8.2020)
- ↑ Hajar R. Risk factors for coronary artery disease: historical perspectives. Heart views: the official journal of the Gulf Heart Association. 2017 Jul;18(3):109.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5686931/ (last accessed 8.8.2020)
- ↑ Physiopedia Acute Coronary Syndrome (last accessed 8.8.2020)
- ↑ Collins Dictionary of Medicine © Robert M. Youngson 2004, Available from: https://medical-dictionary.thefreedictionary.com/unstable+angina2005 (last accessed 8.8.2020)
- ↑ Echo learning STEMI Available from: https://ecgwaves.com/topic/nstemi-non-st-elevation-myocardial-infarction-unstable-angina-criteria-ecg-diagnosis-management/ (last accessed 8.8.2020)
- ↑ ECG STEMI Available from:https://www.ecgmedicaltraining.com/what-is-a-stemi/ (last accessed 8.8.2020)
- ↑ Healthline NSTEMI Available from:https://www.healthline.com/health/nstemi#nstemi-vs-stemi (last accessed 8.8.2020)