Congenital Heart Disease
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Franca Ebomah, Naomi O'Reilly, Shaimaa Eldib and Mila Andreew
Introduction[edit | edit source]
Congenital heart diseases (CHD), are problems with the heart’s structure that are present at birth. They may change the normal flow of blood through the heart. Congenital heart defects are the most common type of birth defect.
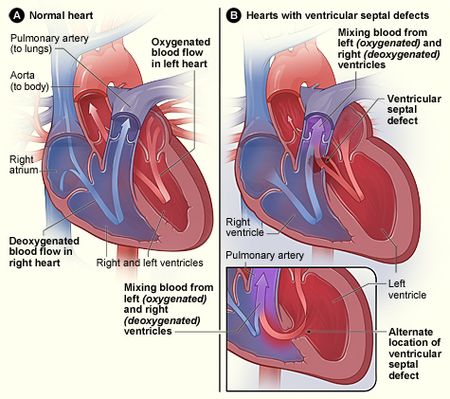
- Ventricular septal defects (VSDs) are the most common congenital cardiac anomaly in children and the second most common congenital abnormality in adults[1].
Image 1: Figure A shows the structure and blood flow in the interior of a normal heart. Figure B shows two common locations for a ventricular septal defect. The defect allows oxygen-rich blood from the left ventricle to mix with oxygen-poor blood in the right ventricle.
There are many types of congenital heart defects. The most common defects involve the inside walls of the heart, the valves of the heart, or the large blood vessels that carry blood to and from the heart. Some defects require no treatment, but some require treatment soon after birth. Because diagnosis and treatment of congenital heart defects has improved, more babies are surviving and now many adults are living with congenital heart defects[2].
Congenital heart disease
- Is an important contributor to morbidity and mortality in both children and adults, and large disparities exist throughout the world in access to care and outocomes[3],
- Is the most common congenital malformation diagnosed in newborns, with birth prevalence reported to be 10‰ of live births worldwide.
- Is the most common reason babies are admitted to paediatric intensive care and is a leading cause of infant death, and one of the leading causes of disease-related disability in children under the age of five[4].
Early diagnosis and advances in cardiac surgery and interventional cardiology have significantly increased survival of patients with CHD over the past several decades. The number of people with CHD who reach adulthood has also risen, which is estimated to be >1 million in the United States and 1.2 million in Europe. Although there have been tremendous advancements in the diagnosis and management of congenital heart disease over the past several decades, much of what is known about congenital heart disease care comes from regions that have a high Socio-demographic Index (SDI)[3]
Despite remarkable success in the surgical and medical management of CHD, many interventions are palliative rather than curative, and some survivors still have significant residual hemodynamic and electrical conduction abnormalities and experience cardiovascular complications over the long term. Surgical and medical interventions for CHD, including intervention with stents, frequent catheterization, long‐term medication, and so on, have been confirmed to increase the risk of cardiovascular disease.[5]
Disease Burden[edit | edit source]
Important findings include
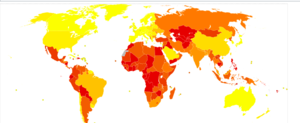
- Global estimate of nearly 12 million people living with congenital heart disease in 2017, an 18·7% increase from 1990.
- The number of deaths attributed to congenital heart disease in 2017 was estimated at 261 247, a decline of 34·5% from the estimated number of deaths in 1990.
- CHD is a leading cause of infant mortality, ranking 6th globally and 2nd in regions with a high Socio-demographic Index (SDI).
- As top-ranking causes of mortality continue to shift from communicable diseases to non-communicable diseases, the importance of CHD as a cause of global infant mortality is likely to continue to increase in the years to come.
- Children are surviving with congenital heart disease and complex forms of congenital heart disease, understanding the comorbidities and potential disabilities faced by individuals living with congenital heart disease is of crucial importance. [3]
Image 2: (DALY) lost from Congenital heart anomalies in 2012 per million persons lightest yellow 72-869 though to darkest colour 4,915-11,321
Causes/Risk Factors and Diagnosis[edit | edit source]
Congenital heart defects happen because the heart does not develop normally while the baby is growing in the womb. Doctors often do not know why congenital heart defects occur. Researchers do know that genetics can sometimes play a role.
- Often we do not know why congenital heart defects occur. Researchers do know that the risk of having a baby with a congenital heart defect is influenced by family history and genetics, the mother’s health, sex (slightly higher in males), and exposure during pregnancy to environmental factors eg Smoking during pregnancy or exposure to secondhand smoke.Taking angiotensin-converting enzyme (ACE) inhibitors for high blood pressure and retinoic acids for acne treatment—in the first trimester. Other medical conditions can also raise your risk for having a baby with a congenital heart defect eg diabetes, rubella.
Diagnosis: Some congenital heart defects are diagnosed during pregnancy or soon after birth. Others may not be diagnosed until adulthood. - Congenital Heart Defects. Almost all newborns in the 1st world countries are screened for congenital heart defects in the first few days after birth. However, babies at high risk for a congenital heart defect may have screening before the baby is born or strategies to help prevent a congenital heart defect.[2]
Treatment[edit | edit source]
Treatment will depend on which type of congenital heart defect. Treatments for congenital heart defects include medicines, surgery, and cardiac catheterization procedures. Many congenital heart defects do not require treatment at all. However, children with critical congenital heart defects will need surgery in the first year of life. Some people with congenital heart defects may need treatment, including repeated surgery, throughout their lives. All people with congenital heart defects should be followed by a cardiologist throughout their whole life[2].
Physiotherapy[edit | edit source]
Lifestyle Education
- Being physically active (PA) Most people with congenital heart defects can be physically active. Physical activity can improve physical fitness and lower many heart disease risk factors, including high blood pressure. The amount or type of physical activity you or your child can do depends on the type of congenital heart defect, the medicines you may be taking, and the devices that may be implanted. Some people with congenital heart defects may need to avoid competitive sports. Most people with CHD can participate in recreational sports, physical education classes, or general physical activity. Ask your doctor how much and what kinds of physical activity are safe for you or your child. Remember to ask the doctor for a note that describes any limits on your child's physical activities. Schools and other groups may need this information.
- Heart-healthy eating. Following a heart-healthy eating pattern, which includes consuming plenty of vegetables, fruits, and whole grains, reduces the risk of high blood pressure and obesity.
- Aiming for a healthy weight. After treatments and surgery, growth and development may improve. Children and adults with congenital heart defects are at risk for obesity, which can lead to high blood pressure and other conditions that can increase the risk for heart problems[2].
Specific Physical Activity Information
There is emerging consensus that children and adolescents with CHD should be encouraged to adopt a physically active lifestyle, and consequently, current sports recommendations for the majority of patients with simple and moderate CHD include participation in competitive sports, leisure sports and PA unrestricted following the World Health Organisation (WHO) recommendations for healthy children, i.e., daily participation of 60 min in moderate-to-vigorous PA that is developmentally appropriate and enjoyable. Children with complex CHD or other risk factors (for example pacemaker, cardioverter-defibrillator, channelopathies) frequently need specific individualized solutions. This can be covered by preventive cardiac rehabilitation groups organized by local pediatric heart centers or alternatively by individualized training programs[6].
PA is markedly reduced in children with CHD, at least in part due to an unexpected high number of physician-recommended PA restrictions. As sedentary lifestyle may have negative implications on cardiovascular risk profile and prognosis, efforts should be directed toward facilitating the access to PA for all CHD patients.
References[edit | edit source]
- ↑ Dakkak W, Oliver TI. Ventricular septal defect. StatPearls [Internet]. 2020 Nov 20.Available:https://www.ncbi.nlm.nih.gov/books/NBK470330/ (accessed 22.4.2021)
- ↑ 2.0 2.1 2.2 2.3 NIH CHD Available from:https://www.nhlbi.nih.gov/health-topics/congenital-heart-defects (accessed 22.4.2021)
- ↑ 3.0 3.1 3.2 Rossano JW. Congenital heart disease: a global public health concern. The Lancet Child & Adolescent Health. 2020 Mar 1;4(3):168-9.Available: https://www.thelancet.com/journals/lanchi/article/PIIS2352-4642(19)30429-8/fulltext (accessed 22.4.2021)
- ↑ The Conversation Childhood heart disease has a profound impact and is under-recognisedAvailable: https://theconversation.com/childhood-heart-disease-has-a-profound-impact-and-is-under-recognised-84377(accessed 22.4.2021)
- ↑ Wang T, Chen L, Yang T, Huang P, Wang L, Zhao L, Zhang S, Ye Z, Chen L, Zheng Z, Qin J. Congenital heart disease and risk of cardiovascular disease: a meta‐analysis of cohort studies. Journal of the American Heart Association. 2019 May 21;8(10):e012030.Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6585327/ (accessed 22.4.2021)
- ↑ Siaplaouras J, Niessner C, Helm PC, Jahn A, Flemming M, Urschitz MS, Sticker E, Abdul-Khaliq H, Bauer UM, Apitz C. Physical Activity Among Children With Congenital Heart Defects in Germany: A Nationwide Survey. Frontiers in Pediatrics. 2020;8.Available: https://www.frontiersin.org/articles/10.3389/fped.2020.00170/full (accessed 22.4.2021)