Assessment and Management of Concussion
Original Editor - Siobhán Cullen
Top Contributors - Siobhán Cullen, Rasha Moghanam, Robert Quick, Mathius Kassagga, Admin, Laura Ritchie, Jonathan Wong, Kim Jackson, Nikhil Benhur Abburi, Carina Therese Magtibay, Rucha Gadgil, Candace Goh, Kalyani Yajnanarayan, Nupur Smit Shah, Naomi O'Reilly, WikiSysop, Karen Wilson, Vidya Acharya, Claire Knott, Wanda van Niekerk, 127.0.0.1 and Lauren Lopez
What is a Concussion?
[edit | edit source]
| [1] |
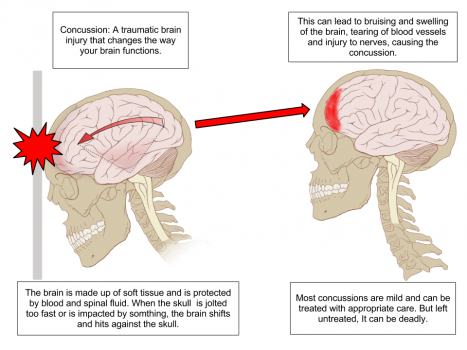
A concussion is a subcategory of traumatic brain injury. In the literature ‘mild traumatic brain injury’ and the term ‘concussion’ are often used interchangeably. The consensus statement on concussion defines it as ‘a complex pathophysiological process affecting the brain induced by biomechanical forces[2].
80-90% of concussions resolve with 7-10 days. If concussion lasts longer than 10 days other potential diagnoses should be reconsidered and the players care managed by the MDT. It should be noted that in some cases duration of recovery may be prolonged, particularly in children and adolescents. The information that follows applies to persons aged 13+. Below this age symptoms reported by children are different to those over 13. Hence, the following information does not apply to under 13s-a more age-appropriate symptom checklist would be required by this population.
Mechanism of Injury
[edit | edit source]
Concussion can be caused by a number of different biomechanical means including a blow to the face, neck or head. Indeed a concussion can result from any blow to the body in which the force is resultantly transmitted to the head [2].
Clinical Presentation[edit | edit source]
The clinical presentation of a concussion can vary greatly, from significant changes in balance to less obvious changes such as sleep disturbances. Clinical, neurological, behavioural, physical and/or cognitive symptoms may present.It is important to note that symptoms can appear instantly at the time of the incident, or some minutes or hours after the event.
The 2012 consensus statement lists the following signs and symptoms of concussion:
1. Symptoms—somatic (eg, headache), cognitive (eg, feeling like in a fog) and/or emotional symptoms (eg, lability);
2. Physical signs (eg, loss of consciousness (LOC) Although published findings in concussion describe LOC associated with specific, early cognitive deficits, it has not been noted as a measure of injury severity.77 78, amnesia); A variety of immediate motor phenomena (eg, tonic posturing) or convulsive movements may accompany a concussion. Although dramatic, these clinical features are generally benign and require no specific management beyond the standard treatment of the underlying concussive injury.
3. Behavioural changes (eg, irritability);
4. Cognitive impairment (eg, slowed reaction times);
5. Sleep disturbance (eg, insomnia)[2].
However, this list is not exhaustive and the following additional signs and symptoms have been cited elsewhere in the literature
chronic headaches,
dizziness and vertigo,
difficulty concentrating,
word-finding problems,
depression,
impulsiveness
(DeKosky et al 2010)
The existence of only ONE of these symptoms is enough for a concussion to be suspected.
Post Concussion Syndrome:
This occurs when concussion symptoms persist for longer than the usual 7-10 days. Symptoms can last for weeks to months, but generally resolve within 3 months. However, cases have been reported of symptoms lasting up to a year.
It is uncertain what causes post concussion syndrome to develop in some players and not in others. There is no proven correlation between injury severity and an increased likelihood of developing concussion. Some researchers have suggested that this syndrome results from structural damage to the brain or disruption to neurotransmitter systems. However, others argue that it is more likely that symptoms are related to psychological factors. Treatment usually involves pharmacological intervention and education.
Risk Factors for Developing a Concussion[edit | edit source]
A number of different factors associated with higher risk of experiencing a concussion have been outlined in the literature. These are outlined below.
Sex:
A higher rate of concussion has been recorded for males in all sports. However, it appears likely that this is a result of the larger number of males participating in the sports investigated. In an evidence based guideline update by Giza et al in 2013[3], it was suggested that the association of a certain sex with higher rates of concussion varies across different sports, with a higher rate of concussion for females in both soccer and basketball. Other studies have suggested that the higher incidence of concussion noted in females may be a result of greater reporting of concussive symptoms by female athletes, and as a result of their smaller head size and neck strength relative to their male counterparts [4].
Type of Sport:
As stated above, the risk of concussion associated with sports varies across different sports. Australian rugby and American football are associated with the highest incidence of concussion, while a lower risk is associated with sports such as baseball, softball, volleyball and gymnastics. Several high quality studies have associated soccer with the greatest concussion risk for female athletes [3].
Position:
The athlete’s playing position can also be associated with higher/lower concussion risk. In American football greater risk has been associated among linebackers, offensive linemen, and defensive backs compared to receivers. Currently there is insufficient evidence to associate player position with greater/lesser concussion risk in other sports [3].
Athlete-related Factors:
Several factors specific to the individual athlete have been associated with greater concussion risk, including a body mass index greater than 27 kg/m2.
Training time of less than 3 hours alos weekly likely increase the risk of concussion[3].
Currently in the literature, there is insufficient evidence to determine links between age and competition level and risk of concussion.
Assessment[edit | edit source]
According to the 2012 consensus statement[2], when a player shows ANY features of a concussion, management should progress as follows:
A. The player should be evaluated by a physician or other licensed healthcare provider onsite using standard emergency management principles and particular attention should be given to excluding a cervical spine injury. Symptom, cognitive, cranial nerve and balance assessments should all be included in the examination.
B. The appropriate disposition of the player must be determined by the treating healthcare provider in a timely manner. If no healthcare provider is available, the player should be safely removed from practice or play and urgent referral to a physician arranged.
C. Once the first aid issues are addressed, an assessment of the concussive injury should be made using the SCAT3 or other sideline assessment tools.
D. The player should not be left alone following the injury and serial monitoring for deterioration is essential over the initial few hours following injury[2].
As with all potentially serious injuries, if concussion is suspected, sufficient time for assessment should be allowed. The final decision in a diagnosis of concussion and the player’s ability to return to play lies with the clinician, based on their clinical judgement.
Outcome Measures[edit | edit source]
Difficulties arise in diagnosing a concussion as a result of the hugely variable presentations of each individual injury. Matters can be further complicated by the time pressures clinicians find themselves under in sporting events. It is therefore important that the clinician is aware of tools available to them to assist them in making an accurate diagnosis of concussion.
Cognitive Function:
Assessment of cognitive function is an essential component of assessment. A number of short neuropsychological tests assessing memory and attention are available. These include the Maddocks’ questions, Sport Concussion Assesment Tool 3 (SCAT 3) and Standardised Assesment of Concussion (SAC).
Maddocks’ Questions:
This is a list of 8 standardised memory assessment questions. These have been proven to be more reliable than the use of general orientation questions[2].
Benefits:
• Relatively short to administer
• More sensitive than standard orientation questions
Limitations:
• There is no guideline indicating the cut off for return to play-for example if a player answers only 1 of the 8 questions incorrectly should they be removed from the field of play/ do all 8 questions have to be asked?
• There is a dearth of literature investigating the reliability and validity of these widely used questions.
• Cannot be used as a stand alone tool-need to be used in conjunction with the clinicians’ judgement.
SCAT 3:
A concussion assessment tool suitable for use for people aged 13+. The test includes assessment of the player’s Glasgow Coma Scale, Maddocks’ questions, symptom evaluation, cognitive, physical, balance, coordination, delayed recall and neck examination. Pre season baseline measurements can be used as useful comparisons to help in the identification of a concussion.
Benefits:
• Incorporates a number of different concussion assessments into one tool.
• Available as a phone app
Limitations:
• The SCAT 3 takes between 15-20 minutes to complete
• The SCAT 3 is newly published and as such has not yet been assessed for reliability and validity. Its forerunner the SCAT 2 has also not had its’ reliability and validity assessed in any large scale studies.
• Despite its’ wide scale use in sport, the SCAT2 has its critics, with a meta-analysis in 2013 criticising its’ design and scoring[5]. A study by Chan et al 2013[6] found the test to have low test-retest reliability and thus questioned its suitability for use in diagnosing a concussion.
• A high score on the SCAT does not necessarily mean that a player is not concussed, as symptom onset can be delayed.
• It must be noted that there have been reports of athletes purposefully scoring a low baseline measurement to avoid being taken off the pitch when concussed
Standardised Assessment of Concussion (SAC):
Assesses orientation, immediate memory, concentration and delayed recall. It takes ~6 minutes to administer.
Sensitivity: 80-94% Specificity: 76-91%[3]
Benefits:
• Relatively short time to administer
• Assess a number of different functions commonly affected by concussion
Limitations:
• Certain studies have reported the sensitivity of the SAC to be only 80%, meaning that a large number of concussed players would not be identified using the tool[7]
• No cut-off scores to determine the diagnosis of a concussion, have been established for the SAC
Post-Concussion Symptom Scale/Graded Symptom Checklist:
Consist simply of a list of symptoms of concussion that must be checked for in the athlete either by trained personnel or the athlete themselves. A baseline must be established prior to use. Studies calculate a sensitivity of between 64–89%, and a specificity of between 91– 100%[3].
Benefits:
• Simple to use
• Relatively short time to administer
Limitations:
• Poor sensitivity means that a number of athletes with a concussion would not be identified using this assessment alone.
Balance Error Scoring System (BESS):
Balance assessment tool. Takes ~ 5 minutes to complete. Assesses postural stability in a number of different stances on both firm and foam surfaces. Scores range from 0-60 with lower scores indicating better balance.
Benefits:
• Postural stability testing has been shown to be a reliable and valid tool for objectively assessing the motor domain of neurological functioning[2].
• Relatively short time to administer
• Simple administration-consists of standardised instructions and requires no training
• Examines the effects of mild head injury on postural stability without the need for expensive equipment
• Can be performed in almost any environment
Limitations:
• Does not assess any other functions commonly affected in concussion
• Very poor sensitivity of between 34–64%, specificity of 91%[3]
Sensory Organization Test:
Uses a force plate to test a player’s ability to maintain their balance while orientation information available to somatosensory and/or visual inputs are altered.
Limitations:
• Requires use of a force measuring plate and is therefore impractical for sideline use.
• Expensive test as equipment required for assessment.
• Low sensitivity of between 48-61% reported. Specificity found to be between 85-90%[3]
Canadian CT Head Rule
This measure consists of a list of signs and symptoms used to decide whether a head injury or concussion warrants a scan.
Benefits:
• Simple to use
• High risk factors were seen to be 100% sensitive when predicting the need for neurological intervention.
• Medium risk factors were 98.4% sensitive for predicting clinically important brain injury[8].
• A cross-sectional study which compared the use of Canadian CT head rule which compared its use to the gold standard in the detection of head injury the Computed Tomography (CT) Scan and agreed that it is an excellent decision making tool.
Limitations:
• Low specificity (49-60%) means that a number of patients without concussion will be recommended for a scan if using the tool. However, it is more important that the tool has a high sensitivity and thus that no patients with a concussion are missed using the tool.
As can be seen above a number of different diagnostic tools are available to the clinician to assist them in recognising a concussion. Each has its advantages and disadvantages as discussed above. None of these tools should be used in isolation. Rather, they should be used in conjunction with the clinician’s clinical judgement. Combining diagnostic tests is likely to increase the accuracy of concussion diagnosis, when compared to using individual tests. However, at present the best combination of tests to improve concussion identification has not been established.
Diagnostic Procedures[edit | edit source]
The 2012 consensus statement recommends the following with regard to determining the need for further investigations into mild head injury:
A. A medical assessment including a comprehensive history and detailed neurological examination including a thorough assessment of mental status, cognitive functioning, gait and balance.
B. A determination of the clinical status of the patient, including whether there has been improvement or deterioration since the time of injury. This may involve seeking additional information from parents, coaches, teammates and eyewitnesses to the injury.
C. A determination of the need for emergent neuroimaging in order to exclude a more severe brain injury involving structural abnormality[2]
There are a number of different investigations that may be conducted to assist in diagnosing/excluding a concussion. Most commonly structural neuroimaging is performed. Brain CTs and MR brain scans have been found to add little to concussion evaluation, but should be performed if there is ever suspicion of an intracerebral or structural lesion (eg skull fracture)[2].
fMRIs have been found to show activation patterns that correlate with symptom severity in concussion, and with recovery. However, they are not part of routine assessment.
Other forms of imaging are still in the early stages of development and cannot be recommended presently.
Management[edit | edit source]
| [1] |
If a concussion is suspected, a player should NOT be allowed to return to play on the same day[2].
Management of a concussion is mainly by way of physical and cognitive rest. The literature suggests that rest may be beneficial in the immediate symptomatic stages of concussion. However evidence is sparse, particularly in terms of assessing the long-term benefits of rest and how much rest is needed[2].
Despite this the consensus developed the graded return to play protocol for use in sports. This uses a sensible approach to gradual return to sport once acute symptoms have been cleared. This is discussed later.
Pharmacological Therapy[edit | edit source]
In sports concussion pharmacological therapy is usually applied if patients have specific/prolonged symptoms (eg sleep disturbance) OR to modify the pathophysiology of the concussion in order to shorten the length for which concussion symptoms are experienced.
Return to Play (RTP)[edit | edit source]
RTP decisions continue to be made on an individual basis based upon the clinician’s clinical judgement.
A player suspected of suffering a concussion should not RTP on the same day. Studies have shown that athletes allowed to return to play on the same day are more likely to have delayed neurophysiological symptoms that may not be evident on the sidelines[2].
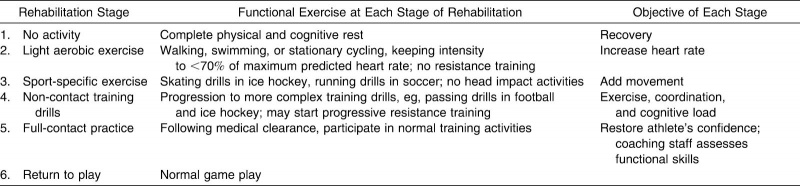
The Consensus 2012 statement[2] suggests the use of a graduated return to play protocol for players post concussion. This is outlined below.
Using this protocol the athlete should gradually progress through the different levels before fully returning to play. The athlete may only progress to the next level of the protocol if they remain asymptomatic on the current level for 24hours.
Following completion of this protocol the athlete should not have any symptoms at rest or with provocative exercise.
If at any point during the protocol the athlete displays/reports concussive symptoms they must drop back to the previous symptom-free level. Progression can begin once more after the athlete has a further 24hr rest period.
NOTE: A previously concussed athlete should only return to play when they are symptom free AND not taking any medications that could mask/alter the symptoms of concussion.
Pre Screening[edit | edit source]
Pre screening for concussion is a valuable tool when working with a team. Not only does it help to identify players with a past history of concussion, but also helps to identify those at a greater risk. It also provides an opportunity to educate the players on the signs and symptoms of a concussion as well as the risks of continuing to play with a concussion.
Any concussion pre-screening should include specific symptom questions as well as questions regarding the duration of any previous concussions. It should be noted that relying on the recall of other players/coaches for concussive injuries has been shown to be unreliable[2].
Post-Concussion Syndrome[edit | edit source]
Please see this page for information on Post-Concussion Syndrome
Long-term Consequences of Concussion[edit | edit source]
The seriousness of a concussion injury is best understood by looking at the long-term consequences of the injury. This is a growing area of research.
It has been found that a single-incident of traumatic brain injury is present in the history of between 20-30% of Alzheimer’s/Parkinsonism patients. This is compared to only 8-10% of controls[9].
Belanger et al (2010)[10] found that multiple concussions were associated with poorer performance in tests of delayed memory and executive functioning.
Chronic Traumatic Encephalopathy (CTE) is a progressive degenerative disease of the brain[11]. It is associated with a history of repetitive brain trauma and results in memory loss, confusion, depression, aggression, impulse control difficulties, impaired judgement and progressice dementia. It has been most commonly linked with sports such as American football, boxing and hockey. Symptoms may begin years after the cessation of brain trauma.
Useful Linksand Resources
[edit | edit source]
- Consensus statement and return to play guidelines: bjsm.bmj.com/content/47/5/250.full
- SCAT 3: bjsm.bmj.com/content/47/5/259.full.pdf
- http://www.parachutecanada.org/concussion
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1bEX5bJHyhtyg3F2OvMSRzOp6Ahv9jQRTxIeRzTL5-x5gfJEw2
References[edit | edit source]
- ↑ 1.0 1.1 Dr. Mike Evans.Concussion 101, a Primer for Kids and Parents. Available from: http://www.youtube.com/watch?v=zCCD52Pty4A [last accessed 14/6/13]
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 McCrory P, MeeuwisseWH, Aubry M, Cantu B, Dvorak J, Echemendla RJ, Engebretsen L, Johnston K, Kutcher JS, Raftery M, Sills A, Benson BW, Davis GA, Ellenbogen RG, Guskiewicz K, Herring SA, Iverson GL, Jordan BD, Kissick J, McCrea M, McIntosh AS, Maddocks D, Makdiss M, Purcell L, Putukian M, Schneider K, Tator CH, Turner M. Consensus Statement on Concussion in Sport: the 4th International Conference on Concussion in Sport. Br J Sports Med. 2013; 47(1): 250-258
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Giza CC, Kutcher JS, Ashwal S, Barth J, Getchius TS, Gloia GA, Gronseth GS, Guskiewickz K, Mandel S, Manley G, McKeag DB, Thurman DJ, Zavonte R. Summary of evidence-based guideline update: Evaluation and management of concussion in sports: Report of the guideline development subcommittee of the American academy of neurology. Neurology [Internet]. 2013 Mar 18 [cited 2013 Jun 1]; 80(24). 2250-2257. Available from: http://neurology.org/content/early/2013/03/15/WNL.0b013e31828d57dd
- ↑ Lincoln AE, Caswell SV, Almquist JL, Dunn RE, Norris JB, Hinton RY. Trends in concussion incidence in high school sports: a prospective 11-year study. Am J Sports Med. 2011; 39(5): 958-63.
- ↑ McCrea M, Barr WB, Guskiewicz K, Randolph C, Marshall SW, Cantu R, Onate JA, Kell JP. Standard regression-based methods for measuring recovery after sport-related concussion. J Int Neuropsychol Soc. 2005; 11(1): 28-69.
- ↑ Chan M, Vielleuse JV, Vokaty S, Wener MA, Pearson I, Gagnon I. Test-retest reliability of the sport concussion assessment tool 2 (SCAT 2) for uninjured children and young adults. Br J Sports Med. 2013; 47.
- ↑ The Lancet Neurology. Time for a game changer in the management of concussion. Lancet. 2013; 12(5), 415.
- ↑ Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, McKnight RD, Verbeek R, Brison R, Eisenhauer ME, Greenberg G, Worthington J. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001; 357(9266): 1391-1396.
- ↑ DeKosky ST, Ikonomovic MD, Gandy S. Traumatic brain injury-football, warfare and long term effects. N Engl J Med. 2010; 363(14), 1293-6.
- ↑ Belanger HE, Spiegel E, Vanderploeg RD. Neuropsychological performance following a history of multiple self-reported concussions: a meta-analysis. J Int Neuropsychol Soc. 2010; 16(2), 262-7.
- ↑ Boston University. What is Chronic Traumatic Encephalopathy? [Internet]. Boston: Boston University [undated]. Available from: http://www.bu.edu/cste/about/what-is-cte/