Comprehensive Geriatric Assessment
Purpose[edit | edit source]
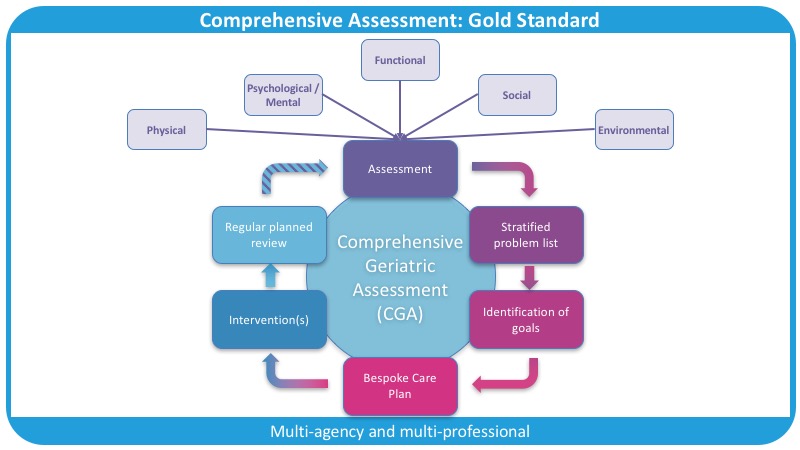
Comprehensive geriatric assessment (CGA) is an iterative collaborative multidimensional framework and process of assessment used to assess people living with frailty. These people often have complex, multiple and interdependent problems (multimorbidity) which make their care more challenging than in younger people, or those with just one medical problem.[1]. This process is considered the best way to evaluate the health status and care needs of older adults[2]. The strength of the CGA lies in the fact it is a multidimensional holistic assessment of an older person that takes into consideration health and wellbeing. As a result of the assessment, a problem list is created and plan is created to address issues. The emphasis of the plan is to improve quality of life and ability to cope for the individual with particular importance placed on what matters most to the patient[3].
The CGA differs from a standard evaluation as it emphasizes quality of life and functional status, prognosis, and outcome, entailing greater depth and breadth. The hallmarks of CGA are the employment of interdisciplinary teams and the use of any number of standardized instruments to evaluate aspects of patient functioning, impairments, and social supports.[4]
The Centre of The CGA[edit | edit source]
There are five domains at the centre of the CGA which form the framework for the assessment. By ensuring each domain is considered during each assessment the patient and their needs are considered as a whole. The benefits gained by performing the CGA are only realised when all of the domains are covered[3].
- Physical health and nutritional status (e.g. COAD, osteoarthritis, urinary incontinence, hearing or visual impairments)[6]
- Mental and emotional health (e.g. depression, cognition, vascular dementia)
- Functional (e.g. unable to shower herself, or do the cleaning)
- Social (e.g. lives alone, family far away)
- Environmental (e.g. stairs to the bedroom [fall risk], poor lighting)
From the assessment, using validated and reliable outcome measures, a list of problems is formulated and recorded. This allows problems identified to then be addressed. This problem-solving draws on the expertise of the multidisciplinary (MDT) team.
Each expert in a multidisciplinary team (MDT) assesses their domain. The physician (usually a geriatrician or GP) assesses physical and mental health; the pharmacist may undertake a medication review; the nurse assesses various aspects of personal care (for example hygiene and continence); the physiotherapist, balance and mobility; the occupational therapist, activities of daily living; and the social worker, social aspects of the case. If needed others may be involved in the MDT assessment eg speech therapist, dietician[1].
This is not to say that different professions can assess different domains, it is about considering who is the best places that is best equipped to do the best thing for the patient at that time[3].
Frailty is the lack of inbuilt reserve. The accumulation of deficits leads to an inability to deal with new insults or new changes in people with long-term conditions. Using the CGA is a whole-body perspective that ensures the patient is assessed holistically with considerations to the biopsychosocial approach to enable the individual to cope with their problem[3].
Physiotherapists' Role in the CGA[edit | edit source]
The Physiotherapists' involvement in the delivery of a CGA can be incredibly varied and ultimately depends on your speciality, which setting you work in, and the reasons for the patient being referred to you. If there has been a problem identified and you are able to act upon it then you should, if not a referral or signposting to an appropriate clinician is recommended.
Below is a classic list of traditional areas of assessment and treatment a physiotherapist may be involved in during a patients care.
Functional status — Functional status refers to the ability to perform activities necessary or desirable in daily life. Functional status is directly influenced by health conditions, particularly in the context of an elder's environment and social support network.
Activities of daily living —including basic activities of daily living (BADLs) eg bathing, dressing, instrumental or intermediate activities of daily living (IADLs) eg shopping, telephoning, taking medicine, and advanced activities of daily living (AADLs) eg being able to partake in social activities.
Gait speed — In addition to measures of ADLs, gait speed alone predicts functional decline and early mortality in older adults. Assessing gait speed in clinical practice may identify patients who need further evaluation, such as those at increased risk of falls.
Falls/balance — Approximately one-third of community-dwelling persons age 65 years and one-half of those over 80 years of age fall each year[7]. Patients who have fallen or have a gait or balance problem are at higher risk of having a subsequent fall and losing independence. An assessment of fall risk should be integrated into the history and physical examination of all geriatric patients.[8]
As physiotherapists' roles and scopes of practice are expanding, we might be involved in the management of Frailty Syndrome on a number of levels, Physiotherapists could be the starters or part of the iterative process of the Comprehensive Geriatric Assessment. Connecting the patient with other clinicians is key in obtaining the Comprehensive Geriatric Assessment[3].
Outcome Measures[edit | edit source]
Examples of outcome measures that could be employed include:
- Patient-Specific Functional Scale
- Barthel index
- Katz ADL
- FIM
- Elderly Mobility Scale
- BOOMER
- Romberg test
- TUG
- Functional Reach
- 10 metre walk test
Evidence[edit | edit source]
The evidence base for performing a Comprehensive Geriatric Assessment for an inpatient frail population is conclusive. As a summary statement of the evidence: it can be said that compared to usual or standard models of care, which focused on single conditions by a single clinician, without that iterative reviewing approach, the Comprehensive Geriatric Assessment shows significant benefits to both increased independence and reduction of mortality[3].
A 2017 Cochrane review found that older people are more likely to be alive and in their own homes at follow-up if they received CGA on admission to hospital. [9]
A 2017 study on physical fitness of the frail elderly is enhanced by the use of a CGA. It found that in their acute care a CGA unit showed superior results (cf conventional care) in terms of preserving physical fitness at 3 months follow-up. CGA management may positively influence the outcomes of great importance for these patients, such as mobility, strength, and endurance.[10]
The Number Needed to Treat, a statistical value used to assess beneficial and harmful effects of medical interventions[11], of CGA is 13 to avoid 1 unnecessary death or deterioration compared with general medical care[3]. This is a significant number when compared to Statin, a drug that has a high impact in the prevention of strokes and heart attacks.
There is inconclusive evidence [3] of the use of Comprehensive Geriatric Assessment on patients who had a hip fracture. A 2018 review showed it had the following benefits [12]:
- Reduces the risk of mortality
- Reduces the required post-discharge level of care
- Reduces length of stay and overall cost of the overall health needs
However, the same systematic review suggests that readmission rates and delirium rates are not reduced[3].
Frailty Screening[edit | edit source]
Patients' screening can help primary care services and unplanned admissions to plan their caseload and prioritize their resources. However, there is no evidence to suggest systematic screening for frailty could have a positive impact in terms of cost-effective treatment or patients' health.
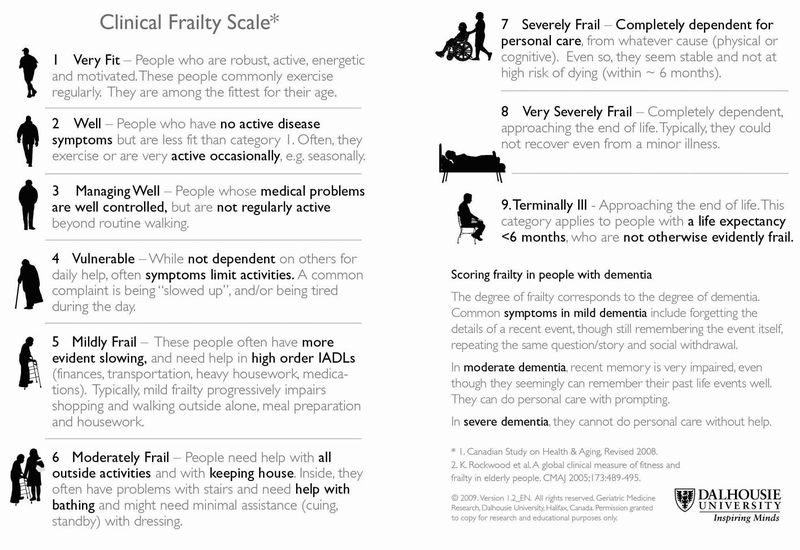
Some scales could be used to diagnose frailty such as Fried's phenotype, clinical frailty scale and the electronic frailty index. The CGA should be performed when a person has a clinical frailty scale score of 5 or more[3].
References[edit | edit source]
- ↑ 1.0 1.1 Wikipedia. Comprehensive Geriatric Assessment. Available from: https://en.wikipedia.org/wiki/Comprehensive_geriatric_assessment (last accessed 4.5.2019)
- ↑ Ouslander JG, Reyes B. Clinical problems associated with the aging process. In: Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 20th ed. New York, NY: McGraw-Hill Education; 2018.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Buxton S. Comprehensive Geriatric Assessment and the Role of a Physiotherapist Course. Physioplus 2020
- ↑ CGA toolkit. Comprehensive geriatric assessment. Available from: https://www.cgakit.com/cga (last accessed 4.5.2019)
- ↑ thehealthline.ca Information Network. Introduction to the Comprehensive Geriatric Assessment Toolkit. AVailable from: https://www.youtube.com/watch?v=ni2FaEboCZU&app=desktop (last accessed 4.5.2019)
- ↑ Lee H, Lee E, Jang IY. Frailty and comprehensive geriatric assessment. Journal of Korean medical science. 2019 Dec 20;35(3).
- ↑ GOV.UK. Guidance, Falls: Applying all our health. Jan 2020. Available from: https://www.gov.uk/government/publications/falls-applying-all-our-health/falls-applying-all-our-health (last accessed:15/09/2020)
- ↑ Ward KT, Reuben DB. Comprehensive geriatric assessment. 2016 Available from: https://www.uptodate.com/contents/comprehensive-geriatric-assessment (last accessed 15.09.2020)
- ↑ Ellis G, Gardner M, Tsiachristas A, Langhorne P, Burke O, Harwood RH, Conroy SP, Kircher T, Somme D, Saltvedt I, Wald H. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane database of systematic reviews. 2017(9). Available from: https://www.cochrane.org/CD006211/EPOC_comprehensive-geriatric-assessment-older-adults-admitted-hospital (last accessed 4.5.2019)
- ↑ Åhlund K, Bäck M, Öberg B, Ekerstad N. Effects of comprehensive geriatric assessment on physical fitness in an acute medical setting for frail elderly patients. Clinical interventions in aging. 2017;12:1929. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5691905/ (last accessed 4.5.2019)
- ↑ Mendes D, Alves C, Batel-Marques F. Number needed to treat (NNT) in clinical literature: an appraisal. BMC medicine. 2017 Dec 1;15(1):112.
- ↑ Eamer G, Taheri A, Chen SS, Daviduck Q, Chambers T, Shi X, Khadaroo RG. Comprehensive geriatric assessment for older people admitted to a surgical service. Cochrane Database of Systematic Reviews. 2018(1).