Claudication
Original Editor - Hetvi Gala
Top Contributors - Hetvi Gala, Oyemi Sillo and Aminat Abolade
Definition[edit | edit source]
Claudication refers to an aching, tired, cramp like and sometimes burning pain mainly in the legs unilaterally or bilaterally, which typically occurs with exercise and walking a certain distance for certain amount of time and subsides with rest.[1]This is termed as intermittent claudication. Rest pain can also occur in severe conditions and can hamper the activities of daily living of the patient.
Claudication is mainly a symptom of an underlying vascular or neurogenic condition. It causes decrease in Functional capacity of an individual. Hence, it is important to categorise the pain as claudication so that one can come to a definite diagnosis and treat it accordingly.
Causes & Pathophysiology[edit | edit source]
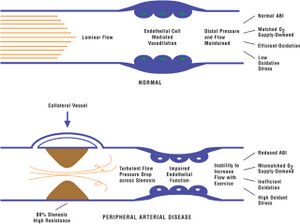
- Peripheral Arterial Disease (PAD) due to atherosclerosis or plaque formation is the most common cause of Intermittent Claudication[2].This narrowing of arteries makes it difficult for the oxygen rich blood to reach the region it supplies. As a result there is imbalance between the demand and supply of oxygen and nutrients especially during activities which increase this demand eg. walking,causing altered aerobic muscle metabolism , resulting in pain.
Clinical features[edit | edit source]
- Patient usually complains of Pain in one or both legs after walking for a particular distance after which the patient needs to sit. The pain is usually burning or cramp like mainly in the calves and buttocks.[2]The site of pain is usually distal to the site of Arterial occlusion.
- Rest pain is due to severe occlusion. Pain is more severe at night.
- Shiny, hairless skin of the legs
- Absent pulse mainly of the lower limbs
- Pallor
- Reduced skin temperature of the region
- Trophic changes of nails
- The limb becomes pale on elevation
Grades for Classifiction of Claudication[edit | edit source]
According to European Society of Cradiovascular Surgery the symptoms of Claudication presented by the patient can help in determining the severity of occlusion
Fontaine classification[3]
| Grade | Symptoms |
|---|---|
| Stage I | Asymptomatic, incomplete blood vessel obstruction |
| Stage II | Mild claudication pain in limb |
| Stage IIA | Claudication at a distance > 200 m |
| Stage IIB | Claudication at a distance < 200 m |
| Stage III | Rest pain, mostly in the feet |
| Stage IV | Necrosis and/or gangrene of the limb |
Diagnosis[edit | edit source]
The following tools can be used for diagnosis of claudication
- Doppler Ultrasound
- Angiogram
- Palpation of peripheral pulses
Differential Diagnosis[edit | edit source]
- Delayed onset of muscle soreness
- Bone lesion causing extrinsic compression of an artery[4]
- Muscle strain
- Arthritis
Assessment of Claudication Distance[edit | edit source]
This is mainly done to assess the severity of occlusion and to monitor the improvement of the patient Post Surgical or Non-Surgical Intervention. [5][6]
Patient is asked to walk on a treadmill. The Distance at which the patient starts feeling pain is marked. This distance is termed as Initial Claudication Distance. However, the patient can walk further for a certain distance, after which the pain is maximum interfering with the patients ability to walk. This distance is termed as Maximum Claudication distance.
The difference in the Initial claudication distance and the Maximum Claudication distance is due to the formation of collateral blood vessels which compensate the occluded blood vessel. However, with increased demand on further walking these collateral vessels become incompetent leading to cessation of walking.
Physiotherapy Management[edit | edit source]
- Treadmill exercises 30-60 mins a day 3 times a day for atleast 3 months.[7]
- Bicycle training
- Upper limb exercises- eg. Biceps curls to increase the endurance
- Plantar flexion resistance exercises[8]
For more details refer Peripheral arterial disease
References[edit | edit source]
- ↑ Medical Definition of Intermittent claudication [Internet]. Medicinenet.com. [cited 2021 Nov 28]. Available from: https://www.medicinenet.com/intermittent_claudication/definition.htm
- ↑ 2.0 2.1 Claudication [Internet]. Hopkinsmedicine.org. [cited 2021 Nov 28]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/claudication
- ↑ Hardman RL, Jazaeri O, Yi J, Smith M, Gupta R. Overview of classification systems in peripheral artery disease. Semin Intervent Radiol. 2014;31(4):378–88.
- ↑ Sutcliffe JB 3rd, Bui-Mansfield LT. AJR Teaching File: intermittent claudication of the lower extremity in a young patient. AJR Am J Roentgenol. 2007;189(3 Suppl):S17-20.
- ↑ Labs KH, Nehler MR, Roessner M, Jaeger KA, Hiatt WR. Reliability of treadmill testing in peripheral arterial disease: a comparison of a constant load with a graded load treadmill protocol. Vascular Medicine. 1999 Nov;4(4):239-46.
- ↑ Kruidenier LM, Nicolaï SPA, Willigendael EM, de Bie RA, Prins MH, Teijink JAW. Functional claudication distance: a reliable and valid measurement to assess functional limitation in patients with intermittent claudication. BMC Cardiovasc Disord. 2009;9(1):9.
- ↑ Spannbauer A, Chwała M, Ridan T, Berwecki A, Mika P, Kulik A, et al. Intermittent claudication in physiotherapists’ practice. Biomed Res Int. 2019;2019:2470801.
- ↑ Mays RJ, Regensteiner JG. Exercise therapy for claudication: latest advances. Curr Treat Options Cardiovasc Med. 2013;15(2):188–99.