Childhood Obesity
Top Contributors - Andrea Civitarese, Rachael Le Page, Lynne Turner, Kim Jackson, Lucinda hampton, Courtney Ferguson, Alison O' Brien, Alexander Dow and Rachael Lowe
Introduction[edit | edit source]
In recent years childhood obesity has risen[1]. In adults, body mass index (BMI) is the method that is most commonly used to diagnose obesity. This method uses an individual's height and weight to establish whether or not they fall within a healthy weight range, the formula is kg/m2. BMI ranges are listed below:
- Healthy weight: BMI = 18.5-24.9
- Overweight: BMI = 25-29.9
- Obese: BMI = 30-39.9
- Severely Obese: BMI = ≥40
In children, it is not just BMI alone that is used to diagnose obesity as children's bodies are constantly changing. To diagnose childhood obesity, paediatricians take into consideration multiple additional factors. Along with BMI, the paediatrician also take into consideration how your child is growing and developing, your family's history of obesity and related health problems (such as diabetes and heart disease), and your child's eating habits, activity levels, and general health.[2]
Why Does This Matter?[edit | edit source]
==The Benefits Of Physical Activity Physical activity and inactivity can have a big effect on a child's health and development in many ways. It is important to know and understand the benefits of regular activity and the risk of inactivity for a child between the ages of 5 - 12 years old.
Regular Activity[edit | edit source]
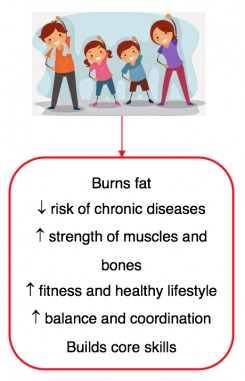
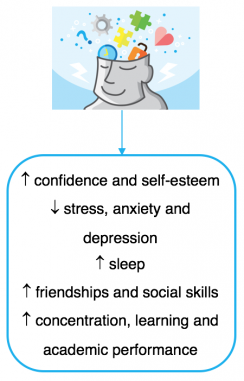
Encouraging a child participate in regular physical activity between the ages of 5 - 12 years old will benefit their body and mind health in a variety of ways including mentally, physically and academically [4][5][6][7][8]. These benefits are detailed below:
The video below provides more details of the top 5 benefits of physical activity for children.
Inactivity[edit | edit source]
It is common to find children playing video games and watching television, however, this leads to a lot of sitting and therefore to an inactive lifestyle which can have a detrimental effect on on children's future health[6][7]. These effects may not show until later life but it is important to be aware of the higher risk of developing the below major diseases due to childhood inactivity[7] and encourage regular physical activity to help reduce and prevent a child developing them in adulthood.
- Obesity
- Heart disease eg coronary heart disease
- Stroke
- Diabetes
- Cancer
- Mental health disease eg anxiety, depression and dementia
- Earlier death
Physical Activity Guidelines for Children (Age 5-12)[edit | edit source]
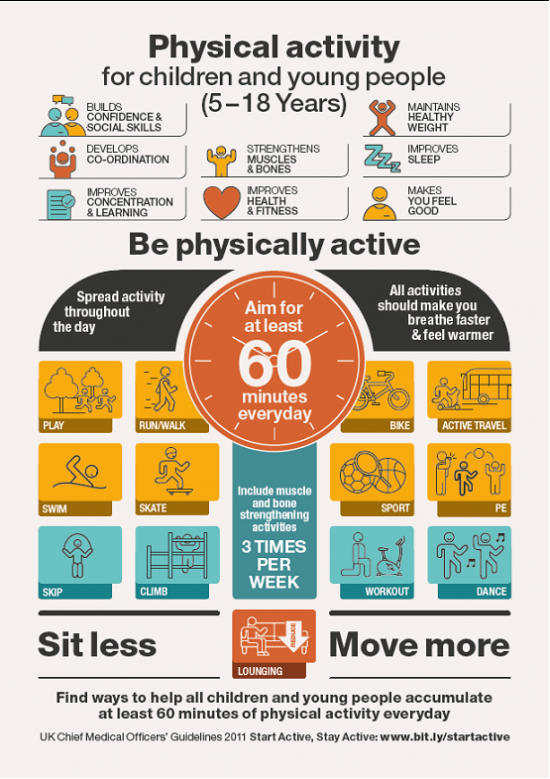
Children (aged 5-12) should partake in at least 60 minutes of physical activity a day - this should range from moderate activity to vigorous activity[10]. Amounts of physical activity greater than 60 minutes, provides additional heath benefits to your child[11].
Moderate Activity[edit | edit source]
Moderate activity raises the heart rate and can make a person sweat. Examples of activities which involve moderate exertion for children include:
- Cycling on flat ground
- Walking to school
- Playing in the playground
- Walking the dog
- Riding a scooter
- Rollerblading[10]
Vigorous Activity[edit | edit source]
Vigorous activity is known to improve general health, bone and muscle strength and self-esteem. Vigorous activity can bring health benefits over and above that of moderate activity. Every one-minute of vigorous activity provides the same health benefits as two-minutes of moderate activity [10]. Examples of activities which involve vigorous exercise for children include:
- Swimming
- Running
- Gymnastics
- Football
- Karate
- Rugby[10]
Bone Strengthening Activities[edit | edit source]
Children should include bone and muscle strengthening exercises at least 3 days a week. Many vigorous activities can help to build strong muscles and bones in children. This can include anything involving running and jumping, such as football or gymnastics[10]. Examples of suitable bone strengthening activities for children:
- Body weight lifting exercises
- Jumping and climbing activites
- Hopscotch
- Rope Skipping
Examples of suitable muscle-strengthening activities for children:
- Sit-ups and Press-ups
- Gymnastics
- Resistance band exercises
- Rock Climbing[10]
Click here to download a helpful fact sheet on physical activity guidelines for children [12].
Barriers and Facilitators to Managing Childhood Obesity[edit | edit source]
One of the key roles of health visitors and health professionals is to effectively present parents with the most up to date evidence on childhood obesity and interventions. Factors such as race, ethnicity, lifestyle, genetics, culture, socio-economic status, and the environment tend to have great influence on dietary choices[13]. Dealing with obesity is a complicated process, which involves a broad sociological awareness and understanding. It also requires tactful and compassionate communication skills that can influence behaviour and bring about positive lifestyle changes by breaking down barriers and identifying facilitators.
Resources Barriers[edit | edit source]
- Financial resources - This can be a massive barrier to physical fitness especially for large families.
- Limited time - long working hours for parents can be a barrier to family exercise, especially if having to work during evenings or on weekends.
- Access and availability of programs - access to exercise programs and activities can often be limited in areas or for certain age groups.
- Knowledge gap - incomplete knowledge surrounding healthy eating[14] [15], regular activity benefits and risk of inactivity.
Social Barriers[edit | edit source]
- Cultural practices and expectations - cultural differences can contribute to difficulty in maintaining a healthy diet and activity levels.
- Interpersonal dynamics: challenging family dynamics, such as shared custody, can make maintaining a healthy eating and exercise routine very challenging[16].
Emotional Barriers[edit | edit source]
- Lack of confidence - uncertainty over the ability to control their child’s weight.
- Defeat - feelings of defeat related to previous failed attempts at weight management.
- Loneliness - young adolescents in particular often describe feelings of isolation and loneliness related to their overweight and obese status.
- Denial - unwillingness of most parents in accepting their child has a weight issue is a big barrier despite their involvement in the medical system [14] [15]
- Negative attitudes - these attitudes from parents, staff and peers can hinder your child’s interest in physical activity[17]
- Embarrassment - vulnerability, disappointment and shame at appearing physically incapable are just some of the emotions your child may experience
Facilitators - Building Partnerships[edit | edit source]
- The importance of building strong partnerships between patients, families, schools and health care providers is essential[18]
- Specifically discussion and collaboration in goal setting with providers is a helpful element for weight management[19].
- Engagement as an entire unit so parents and children can work better in partnership to achieve goals around healthy living.
- GP or practice nurse can refer you to a local weight management programme for children, such as MEND and More Life.
Facilitators - Access to Resources[edit | edit source]
- Primary care centres directly providing programs, including fitness classes, nutrition courses, and cooking classes.
- Showing parents and children how to create a healthy snack that not only looks good but tastes good.
- Access to support groups could be a helpful resource and nutrition education classes
- Access to free local community programmes and after school clubs
- Clearer signposting to available resources
Facilitators - Consistent Encouragement[edit | edit source]
- The use of consistent encouragement by providers needs to be a key component of successful weight management.
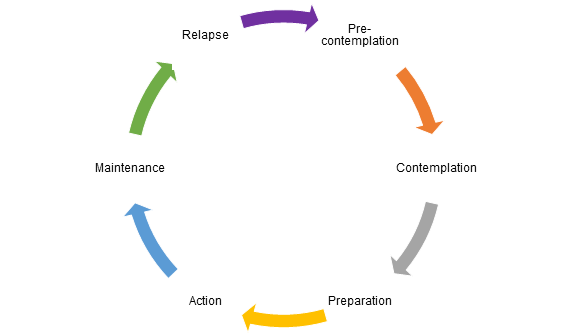
Stages of Change Model [edit | edit source]
Before change can be implemented it is completely normal to go though stages to making these changes a reality, this is referred to as the Stages of Change.
The stages of change are:
- Pre-contemplation (Not yet acknowledging that there is a problem behaviour that needs to be changed)
- Contemplation (Acknowledging that there is a problem but not yet ready or sure of wanting to make a change)
- Preparation/Determination (Getting ready to change)
- Action/Willpower (Changing behaviour)
- Maintenance (Maintaining the behaviour change) and
- Relapse (Returning to old behaviours and abandoning the new changes)
Managing Childhood Obesity[edit | edit source]
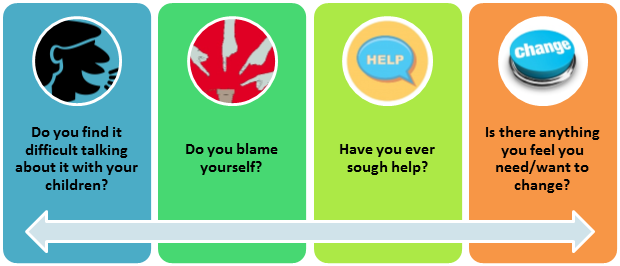
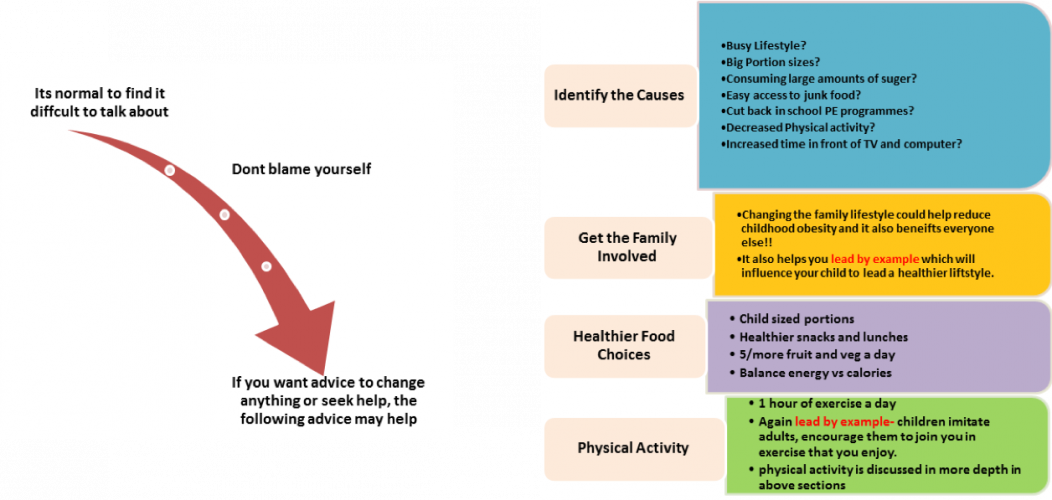
It is important to encourage parents to take proactive steps in managing their child's weight. Below are some useful tips and resources that can be used when talking to parents. Ask parents to reflect on how they currently manage their child's weight.[20].
Reflection alone is not enough, once they have identified problems it is important to take steps to effect change. Encourage parents to follow the steps below:
And remind parents they are not alone, they can consult their General Practitioner and other health professionals for advice.
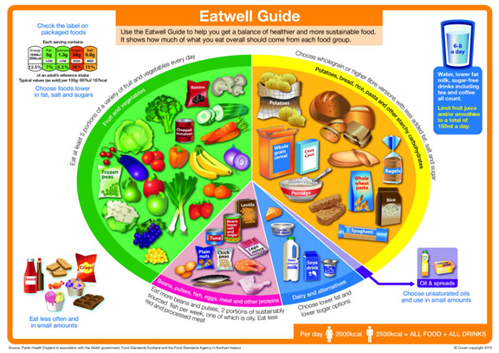
This is a useful image you can share with parents to help guide them on how much food their child should be eating from each food group[21] [22]:
Apps[edit | edit source]
We are in the age of technology and it may be easier to encourage children to get active by the use of free online Apps. Below is a list of free apps online that may help parents to engage their child in physical activity and also provide ideas of activities. This is not an exhaustive list and there is a wide variety and many more apps available.
- HOOP: Find and book fun things to do in your local area for children aged 0-11 years old. (iOS & Android)
- Kiddy Keep Fit by Scotty & Lulu: Uses music and games to get children moving and exercising. (iOS)
- 7-minute workout for kids: High intensity workouts with rests to develop strength, stability and balance. (iOS)
- Habitz: Set up by Health Professionals to help parents to inspire their children to develop healthy habits and lifestyles. (iOS)
- Sworkit Kids – Fitness Meets Fun (7-14 year olds): Wide variety and duration of fun exercises to develop and enhance strength, agility and flexibility. (iOS & Android)
- Appu’s Yoga for Kids: Easy yoga poses for children to enhance and refresh your child's body and mind. (iOS & Android)
- Wuf Shanti Yoga Fun Machine: Yoga app using games and music to promote health and happiness for your child through yoga, meditation and mindfulness. (iOS)
Physical Activities That Involve Minimal Cost[edit | edit source]
Walking, Hiking, Playing catch, Frisbee, Football, Biking, Running, Skipping, Hopscotch, Tug-of-war and Rounders are just some activities that are fun and cost effective.
Conclusion[edit | edit source]
Childhood obesity between the ages of 5-12 years old is rising and is a current global concern and challenge. Unfortunately, in this present age the growing popularity in the daily use of technology in children, among the many other barriers mentioned above, is enhancing an inactive lifestyle. It is important to recognise and understand childhood obesity and how to encourage children to become more active and make changes to help manage a child’s weight and maintain a healthy lifestyle.
Useful Links[edit | edit source]
- NHS Choices: What can I do if my child is very overweight?
- Article: TV in bedroom 'risk factor' for child obesity
- BBC: What to do if your child is overweight
- NHS: Change 4 Life
- NHS Livewell: advice for children health ages 6-15
- Families online: child-wellbeing
- CDC Government: Obesity causes
- MEND Foundation
- More Life
- Childhood Obesity and Weight Problems Help Guide
- Kids eat right: How to Talk to Kids about Weight and Obesity
- Tips for Parents – Ideas to Help Children and Maintain a Healthy Weight: Centers for Disease Control and Prevention
- Healthy Kids' Lunchbox Recipe Ideas
References[edit | edit source]
- ↑ Han, J. C., Lawlor, D. A., & Kimm, S. Y. (2010). Childhood obesity. The Lancet, 375(9727), 1737–1748
- ↑ Mayo Clinic. Childhood Obesity Diagnosis. https://www.mayoclinic.org/diseases-conditions/childhood-obesity/diagnosis-treatment/drc-20354833 (accessed 31 March 2018).
- ↑ Childhood Obesity in the UK Available from: https://www.youtube.com/watch?v=5Km1fFLX6T8 [last accessed 15/03/18]
- ↑ Gov.UK. Publication: Start active, stay active: infographics on physical activity. Available from:https://www.gov.uk/government/publications/start-active-stay-active-infographics-on-physical-activity (accessed 02 April 2018)
- ↑ SSEHS Active. Interpreting the UK physical activity guidelines for children. Available from:http://www.ssehsactive.org.uk/young-people-resources-and-publications-item/39/443/index.html (accessed 02 April 2018)
- ↑ 6.0 6.1 Great Ormond Street. Exercise for children and young people. Available from: https://www.gosh.nhs.uk/medical-information/general-health-advice/leading-active-lifestyle/exercise-children-and-young-people (accessed 02 April 2018)
- ↑ 7.0 7.1 7.2 Kohl III, H. W., and CooK, H. D. Educating the Student Body: Taking Physical Activity and Physical Education to School. Washington: The National Academies Press. Available from: https://www.ncbi.nlm.nih.gov/books/NBK201497/(accessed 02 April 2018)
- ↑ SSEHS Active. Children and young people evidence briefing. Available from:http://www.ssehsactive.org.uk/resources-and-publications-item/40/475/index.html (accessed 02 April 2018)
- ↑ 5 Reasons Why Physical Activity is Important for Children Available from: https://www.youtube.com/watch?v=nD-0Wc6eSUE [last accessed 28/03/18]
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 NHS., 2015. Physical Activity Guidelines for Children and Young People [online]. [viewed 9th April 2018]. Available from: https://www.nhs.uk/Livewell/fitness/Pages/physical-activity-guidelines-for-young-people.aspx
- ↑ World Health Organization., 2016. Physical Activity and Young People [online]. [viewed 9th April 2018]. Avaiable from: http://www.who.int/dietphysicalactivity/factsheet_young_people/en/
- ↑ GOV.UK. 2011. UK Physical Activity Guidelines [online]. [viewed 9th April 2018]. Available from: https://www.gov.uk/government/publications/uk-physical-activity-guidelines
- ↑ El-Sayed, A.M.; Scarborough, P.; and Galea, S. (2011) Ethnic Inequalities in Obesity Among Children and Adults in the UK: A Systematic Review of the Literature. Obesity Review. 12 (5).
- ↑ 14.0 14.1 Keenan, J.; and Stapleton, H. (2010) Bonny Babies? Motherhood and Nurturing in Age of Obesity. Health, Risk&Society, 12 (4).
- ↑ 15.0 15.1 Redsell, S.A.; Atkinson, P.; Nathan, D.; Siriwardena, A.N.; Swift, J.A.; and Glazebrook, C. (2010) Parents’ Beliefs about Appropriate Infant Size, Growth, and Feeding Behaviour: Implications for the Prevention of Childhood Obesity. BMC Public Health, 10 (711).
- ↑ Barriers and Facilitators of Pediatric Weight Management Among Diverse Families Lauren Brown, BA1,2, Sarah-Bianca Dolisca, BS3 , and Jennifer K. Cheng, MD, MPH3,4 Clinical Pediatrics 2015, Vol. 54(7) 643–651 © The Author(s) 2014 Reprints and permissions:
- ↑ Larsen, L.M.; Ledderer, L.; Jarbøl, D.E. (2015) Management of Overweight during Childhood: A Focus Group Study on Health Professionals’ Experiences in General Practice International Journal of Family Medicine. Volume 2015, Article ID 248985
- ↑ Shields N, Synnot A. Perceived barriers and facilitators to participation in physical activity for children with disability: a qualitative study. BMC pediatrics. 2012 Jan 19;16(1):1.
- ↑ Redsell, S.A.; Atkinson, P.; Nathan, D.; Siriwardena, A.N.; Swift, J.A.; and Glazebrook, C. (2013) UK Health Visitors’ Role in Identifying and Intervening with Infants at Risk of Developing Obesity. Maternal and Child Nutrition, 9 (3).
- ↑ TURNER, K.M., SALISBURY, C. AND SHIELD, J.P., 2011. Parents’ views and experiences of childhood obesity management in primary care: a qualitative study. Family Practice, 29(4), pp.476-481.
- ↑ ACADEMY OF NUTRITION AND DIETETICS., 2017. How to Talk to Kids about Weight and Obesity [online]. [viewed 30 March 2018]. Available from: https://www.eatright.org/health/weight-loss/overweight-and-obesity/how-to-talk-to-kids-about-weight-and-obesity.
- ↑ CENTER FOR DISEASE CONTROL AND PREVENTION., 2017. Tips for Parents-Ideas to Help Children and Maintain a Healthy Weight [online]. [viewed 29 March 2018]. Available from: https://www.cdc.gov/healthyweight/children/index.html.