Chikungunya Fever
Original Editor - - Vanessa Rhule
Top Contributors - Vanessa Rhule, Lucinda hampton, Evan Thomas, Rishika Babburu, WikiSysop and Kim Jackson
Chikungunya (CHIK-V) Fever
[edit | edit source]
- An acute febrile illness associated with polyarthralgias, caused by the infection of the arthropod-borne alpha-virus, Chikunguyna virus (CHIK-V).
- The virus is transmitted to humans primarily through the bite of an infected mosquito
- The term Chikungunya is derived from the Makinde word meaning “that which bends up” [1]
- The first discovery of the CHIK-V was in 1952 in Tanzania, Africa with the first outbreak noted in 1999 in Malaysia affecting 27 people [2].
- The virus re-emerged in 2004 in countries of the Indian Ocean and has since then, spread to new locations leading to millions of cases throughout countries globally.
Aetiology[edit | edit source]
- The Aedes Aegypti and Aedes Albopictus mosquitos are the main vectors of the virus.
- The human being becomes the reservoir of infection and transmitted from human to human via the infected mosquito.
- These mosquitos bite mainly in the daytime and are also known to transmit the dengue virus [3]
Risk Factors
[edit | edit source]
- There has been increased prevalence in densely populated, urbanized areas, since humans are the only reservoir of the virus.
- Poor living conditions and maintenance of peridomestic environment including pooling of water in water recipients or tyres and inappropriate waste disposal.These are all sources of Aedes mosquito species.[4]
- Migration and Travelling; the Center for Disease Control estimated approximately 9 million people travel between the United States and the Caribbean each year, increasing the risk of transmission [3]
Clinical Features [1][edit | edit source]
- The incubation period for Chikunguyna fever is noted to be between 3-7 days starting with fevers greater than 38.9°C which can last up to 2 weeks and are biphasic in nature
- Following the fever, majority of infected people develop severe polyarthralgias which are usually symmetric
- Pains are most commonly in the wrists, elbows, fingers, knees and ankles but are not limited to these.
- Pain and Joint swelling are often incapacitating and result in severe disabilities which can last for months.
- The development of a maculopapular rash is often associated
- Additionally, the individual may experience cervical lymphadenopathy, headaches, fatigue, nausea, vomiting, conjunctivitis and myalgia.[5]
- In the acute stage of infection, blood tests may reveal abnormalities such as leukopenia, thrombocytopenia, hypocalcemia and moderate increase in liver function test results
- Asymptomatic cases have also been reported
Maculopapular Rash
[edit | edit source]
[edit | edit source]
Musculoskeletal Implications [edit | edit source]
- In the chronic phase of the infection, individuals may experience musculoskeletal symptoms for several weeks to months
- Joint manifestations such as joint effusions, hygromas, bursitis and axial pain can be identified in areas with previously occurring injuries
- Carpal Tunnel syndrome and Raynaud phenomenon in chronic phase have been noted [6]
- Carpal or Cubital Tunnel syndromes are often a result of hypertrophic tenosynovitis of the anterior wrist [6]
Other Complications[7][edit | edit source]
- Cardiac complications were also reported in a number persons infected with the chikunguyna virus resulting in cases of myocarditis and cardiomyopathy. In many cases, these conditions have been noted to resolve spontaneously
- Chikungunya fever is rarely fatal however there are cases of death has been reported resulting from severe complications or by a weakened immune system
Diagnosis[edit | edit source]
- Chikungunya virus infection should be considered in patients with acute onset of fever and polyarthralgia
- Testing of the serum or plasma detects the virus, viral nucleic acid or virus-specific immunoglobulin and neutralizing antibodies[3]
Differential Diagnosis[edit | edit source]
Dengue fever
Malaria
Rheumatic fever
Leptospirosis
Group A Streptococcus
Rubella
Measles
Parovovirus
Enteroviruses
Adenovirus
Other alphavirus infections
Treatment [3][edit | edit source]
There is no specific antiviral therapy for CHIK-V however treatment is usually centered on symptom reduction.
Includes:
- Non-steroidal Anti-Inflammatory drugs (NSAIDs) to relieve pain and fever
- Rest
- Increased fluid in-take
- Paracetamol
Persistent joint pains may benefit from NSAIDs, Corticosteroids and Physical therapy.However, Aspirin should be avoided because of the increased risk of bleeding
Physical Therapy management[edit | edit source]
The main role of the physiotherapist is to provide supportive care.
Disability level is assessed using a standard disability index and plan of care is based on the patient's presentation.
Joint pain from CHIKV is said to respond to mild exercise. Stretches, passive and active exercises will also assist in the prevention or reduction of contractures and deformities
Global Health Issue[edit | edit source]
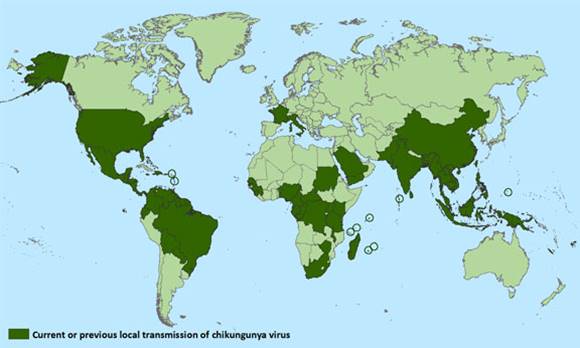
Map of local Transmission of Chikunguyna virus as of March, 2015 [3]
The global expansion of the virus demonstrates the effortlessness with which the virus can spread and infect the human population.
This will in effect can directly reduce productivity and place a burden on the economy on a global level given the long period of illness.
Preventative Measures[edit | edit source]
Vector control through spraying and fogging of chemical insecticides as well as removal of breeding sites on a community level will reduce the rate of infection and transmission
Large mass media coverage, campaigns and educational literature have been put in place with aims to increase awareness on the disease and promote the physical elimination of mosquito breeding sites
References[edit | edit source]
- ↑ 1.0 1.1 Staples J, Breiman R, Powers A. Chikungunya Fever: An Epidemiological Review of a Re‐Emerging Infectious Disease. Clinical Infectious Diseases. 2009;49(6):942-948.
- ↑ Selvaraj I. Chikungunya. Presentation presented at; New Delhi.
- ↑ 3.0 3.1 3.2 3.3 3.4 Cdc.gov. Chikungunya outbreak progresses in Caribbean, Central and South America| CDC Online Newsroom | CDC [Internet]. 2015 [cited 20 June 2015]. Available from: http://www.cdc.gov/media/releases/2014/p1106-chikungunya-outbreak.html
- ↑ Sissoko D, Moendandze A, Malvy D, Giry C, Ezzedine K, Solet J et al. Seroprevalence and Risk Factors of Chikungunya Virus Infection in Mayotte, Indian Ocean, 2005-2006: A Population-Based Survey. PLoS ONE. 2008;3(8):e3066.
- ↑ Rhule V. Chikungunya. Presentation presented at; 2015; Utica, New York and Kingston,Jamaica.
- ↑ 6.0 6.1 Parola P, Simon F, Oliver M. Tenosynovitis and Vascular Disorders Associated with Chikungunya Virus-Related Rheumatism. Clinical Infectious Diseases. 2007;45(6):801-802.
- ↑ Obeyesekere I, Hermon Y. Myocarditis and cardiomyopathy after arbovirus infections (dengue and chikungunya fever). Heart. 1972;34(8):821-827.