Cervicitis
Original Editors - Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Rachael Lewin, Victoria Loving, Lucinda hampton, Elaine Lonnemann, Kim Jackson, 127.0.0.1 and WikiSysop
Definition/Description[edit | edit source]
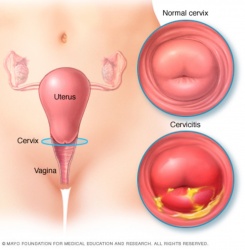
- Cervicitis is defined as the inflammatory response of the cervix to a particular stimuli[1]
- Can be acute or chronic; with chronic occurring due to inadequate treatment or recurrent inflammation[1]
- Non-specific cervicitis is the most common; meaning that it is unrelated to an STI like chlamydia or gonorrhea [2]
- A single instance or acute cervicitis is usually due to an infection like chlamydia or gonorrhea, while chronic is typically due to a non-infectious source[3]
- If left untreated cervicitis can lead to pelvic inflammatory disease[2]
Prevalence[edit | edit source]
Cervicitis is currently rarely reported to epidemiologists making true numbers for prevalence roughly estimated from about 8%-40% [1]
- About 61% of cervicitis cases are of unknown etiology [4]
Characteristics/Clinical Presentation[edit | edit source]
In many case cervicitis remains asymptomatic
- If symptomatic, person may experience vaginal discharge, dyspareunia, intermenstrual bleeding, or postcoital bleeding [1]
- Occasionally will present in an abnormal fashion, such as a cervical growth or uterovaginal prolapse, but that is rare and usually due to delayed or no treatment [1]
Associated Co-morbidities[edit | edit source]
In many cases, Mycoplasma Genitalium bacteria occurs simultaneously with cervicitis [4]
Medications[edit | edit source]
Antibiotics are frequently given once cervicitis is found
- No other medications are usually prescribed to help with this condition[6]
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
In order to diagnose a culture is taken to look for mucopurulent discharge [7]
- A culture is taken to look for specific bacteria like chlamydia, gonorrhea, or mycoplasma genitalium [7]
Etiology/Causes[edit | edit source]
- Cervicitis can be associated with preterm childbirth and pelvic inflammatory disease[7]
- Chlamydia, gonorrhea, trichomonas, bacterial vaginosis and mycoplasma genitalium are all seen to contribute to acute, infectious cervicitis [7]
- Decreased use of condoms with sexual activity are shown to increase the risk for acquiring cervicitis [2]
- Lower education and multiple sexual partners were also seen to contribute to the condition [2]
- Cytomegalovirus has recently been shown to lead to cervicitis as well [8]
Systemic Involvement[edit | edit source]
Untreated, cervicitis can lead to pelvic inflammatory disease (PID) [5]
- Postcoital bleeding is also a common occurrence when cervicitis in inadequately or not treated[9]
Medical Management (current best evidence)[edit | edit source]
Best evidence, is currently antibiotic therapies [4]
- Complementary and Alternative Medicine is now being introduced to treat this diagnosis [6]
Physical Therapy Management (current best evidence)[edit | edit source]
The evidence for PT management of Cerivicitis is low level. Theoretical options have been proposed to include the following but research has not substanitated their use:
- Electrotherapy [6]
- Magnet therapy[6]
- Heat therapy[6]
- Light therapy[6]
- External high frequency calorimetry[6]
- Low frequency pulsed ultrasound therapy [6]
- Iontophoresis[6]
- Shortwave ultrasound combined with intermediate frequency electrical stimulation[6]
- Ozone therapy[6]
- Shortwave diathermy[10]
Differential Diagnosis[edit | edit source]
Case Reports/ Case Studies[edit | edit source]
Case study of a 55 year old female with an ongoing case of untreated cervicitis which produced a growth that mimicked a cervical tumor online.liebertpub.com/doi/abs/10.1089/gyn.2014.0070
Resources
[edit | edit source]
https://www.plannedparenthood.org
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 Singh N, Arora A. An Extreme Case of Chronic Cervicitis Mimicking Cervical Cancer and Causing Third-Degree Prolapse. Journal Of Gynecologic Surgery [serial online]. December 2014;30(6):380-382. Available from: Academic Search Complete, Ipswich, MA. Accessed February 23, 2017.
- ↑ 2.0 2.1 2.2 2.3 Pollett S, Calderon M, Heitzinger K, Solari V, Montano S, Zunt J. Prevalence and predictors of cervicitis in female sex workers in Peru: an observational study. BMC Infectious Diseases [serial online]. April 30, 2013;13:195. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.
- ↑ Efosa O, Uwadiegwu A. Cytopathological Examination and Epidemiological Study of Cervicitis in Commercial Sex Workers (Csws) in Coal City (Enugu), Nigeria. Ethiopian Journal Of Health Sciences [serial online]. July 2015;25(3):225-230. Available from: Academic Search Complete, Ipswich, MA. Accessed April 4, 2017.
- ↑ 4.0 4.1 4.2 4.3 4.4 Taylor S, Lensing S, Lee J, et al. Prevalence and treatment outcome of cervicitis of unknown etiology. Sexually Transmitted Diseases [serial online]. May 2013;40(5):379-385. Available from: CINAHL with Full Text, Ipswich, MA. Accessed February 23, 2017.
- ↑ 5.0 5.1 Sheeder J, Stevens-Simon C, Lezotte D, Glazner J, Scott S. Cervicitis: To Treat or Not To Treat? The Role of Patient Preferences and Decision Analysis. Journal Of Adolescent Health [serial online]. December 2006;39(6):887-892. Available from: PsycINFO, Ipswich, MA. Accessed March 22, 2017
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Liu C, Zhang Y, Kong S, Tsui I, Yu Y, Han F. Applications and therapeutic actions of complementary and alternative medicine for women with genital infection. Evidence-Based Complementary And Alternative Medicine: Ecam [serial online]. 2014;2014:658624. Available from: MEDLINE, Ipswich, MA. Accessed April 4, 2017.
- ↑ 7.0 7.1 7.2 7.3 Lusk M, Garden F, Rawlinson W, Naing Z, Cumming R, Konecny P. Cervicitis aetiology and case definition: a study in Australian women attending sexually transmitted infection clinics. Sexually Transmitted Infections [serial online]. May 2016;92(3):175-181. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.
- ↑ 8.0 8.1 8.2 Abou M, Dällenbach P. Acute cervicitis and vulvovaginitis may be associated with Cytomegalovirus. BMJ Case Reports [serial online]. April 19, 2013;2013 Available from: MEDLINE, Ipswich, MA. Accessed March 22, 2017.
- ↑ Liu H, Chen C, Pai L, Hwu Y, Lee H, Chung Y. Comorbidity profiles among women with postcoital bleeding: a nationwide health insurance database. Archives Of Gynecology & Obstetrics [serial online]. April 2017;295(4):935-941. Available from: Academic Search Complete, Ipswich, MA. Accessed March 22, 2017.
- ↑ Lamina S, Hanif S, Gagarawa Y. Short wave diathermy in the symptomatic management of chronic pelvic inflammatory disease pain: a randomized controlled trial. Physiotherapy Research International [serial online]. March 2011;16(1):50-56. Available from: CINAHL with Full Text, Ipswich, MA. Accessed February 23, 2017.
- ↑ Oliveto J, Muinov L. Cystic Cervicitis: A Case Report and Literature Review of Cystic Cervical Lesions. Journal Of Computer Assisted Tomography [serial online]. July 2016;40(4):564-566. Available from: MEDLINE, Ipswich, MA. Accessed February 23, 2017.