Cardiovascular Disease
Original Editor - Rachael Lowe
Top Contributors - Lucinda hampton, Kim Jackson, Admin, Catriona O'Brien, Evan Thomas and Oyemi Sillo
Introduction[edit | edit source]
The cardiovascular system consists of the heart and blood vessels.
Cardiovascular disease (CVD) or heart disease refer to the following 4 entities
- Coronary artery disease (CAD): Sometimes referred to as Coronary Heart Disease (CHD), results from decreased myocardial perfusion that causes angina, myocardial infarction (MI), and/or heart failure. It accounts for one-third to one-half of the cases of CVD.
- Cerebrovascular disease (CVD): Including stroke and transient ischemic attack (TIA)
- Peripheral artery disease (PAD): Particularly arterial disease involving the limbs that may result in claudication
- Aortic atherosclerosis: Including thoracic and abdominal aneurysms[1]
CVD is the main cause of death globally.
- Measures aimed to prevent the progression of atherosclerosis are the hallmark for primary prevention of CVD.
- Risk factor and lifestyle modification are paramount in the prevention of CVD[1].
- Behavioural risk factors such as physical inactivity, tobacco use and unhealthy diet explain nearly 80% of the CVD burden [2].
Epidemiology[edit | edit source]
- CVD is the number 1 cause of death globally with an estimated 17.7 million deaths in 2015, according to the World Health Organization (WHO).
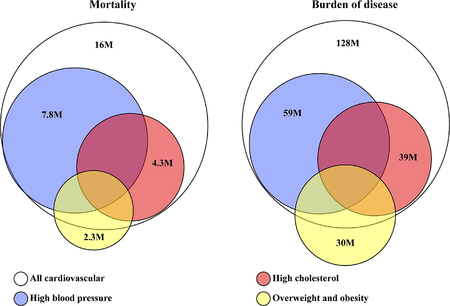
- Image:Global burden of cardiovascular disease with risk factors. The Worldwide Distribution of Cardiovascular Disease Risks
- Over the past decade, CVD has become the single largest cause of death worldwide, representing nearly 30% of all deaths and about 50% of non-communicable diseases (NCD) deaths.[3]
- The burden of CVD further extends as it is considered the most costly disease even ahead of Alzheimer disease and diabetes with calculated indirect costs of $237 billion dollars per year and a projected increased to $368 billion by 2035.
- Cardiovascular diseases (CVD) remain among the 2 leading causes of death in the United States since 1975 with 633,842 deaths or 1 in every 4 deaths (Heart disease occupied the leading cause of death in 2015 followed by 595,930 deaths related to cancer)[1].
What Are Cardiovascular Diseases?[edit | edit source]
CVDs include a wide range of conditions, such as the following:
- Coronary Heart Disease (CHD)
- Cerebrovascular Disease
- Peripheral Arterial Disease
- Rheumatic Heart Disease
- Congenital Heart Disease
- Deep Vein Thrombosis (DVT)
- Pulmonary Embolism
85% of CVD deaths are due to heart attacks and strokes[3]. These are generally acute events caused by a blockage, preventing blood flow to the heart or brain. The most common cause for these blockages is due to a process called atherosclerosis.
Clinically Relevant Anatomy[edit | edit source]
Who Is at Risk?[edit | edit source]
Modifiable risk factors[4] of CVD include
- Unhealthy diet
- Physical inactivity
- Smoking
- Increased consumption of alcohol
Individuals with such behaviours may present with increased blood pressure, lipids and glucose levels, as well as being overweight or obese.
Non-Modifiable risk factors[4] include
- Family history
- Age
- Gender - men at greater risk than pre-menopausal women; post-menopausal women are at similar risk as men
- Ethnicity
- Socioeconomic status
Symptoms of CVD[edit | edit source]
Often the first warning of an underlying cardiovascular disease is a heart attack or stroke.
Symptoms of a heart attack may include:
- Pain or discomfort in the centre of the chest
- Pain or discomfort in the arms, left shoulder, elbows, jaw, or back.
- Shortness of breath
- Nausea or vomiting
- Light-headedness
- Pallor
- Cold sweat
Symptoms of a stroke may include the following:
- Unilateral weakness of the face, arms or legs
- Confusion, difficulty speaking or understanding speech
- Dizziness
- Difficulty seeing with one or both eyes
- Headache
- Fainting
How Physiotherapists Can Help[edit | edit source]
Cardiac rehab programmes have been shown to be very effective, with physiotherapists playing a key role in these programmes. They have been shown to reduce the length of hospital stay as well as the number of cardiovascular-related admissions, cardiac mortality and improved quality of life[5]. Cardiac rehab classes include exercise, education and support.
Physical activity performed at an intensity of >40% of maximal aerobic capacity has shown the greatest benefits in reducing the development or progressing of CVD.[6] For every one metabolic equivalent (MET) increase in aerobic fitness, there is a reduction of 8-17% in premature death.[7] Aerobic exercise increases people’s cardiac output, maximum heart rate, endurance, and arterial blood flow. It may also enhance their blood lipid profiles. For people who already have cardiovascular disease, prescribed aerobic exercise programs by physiotherapists can reduce their risk long-term. Aerobic conditioning activities such as running, rowing and walking along with resistance strength training exercises have been shown to be inversely associated with the risk of
coronary heart disease[8].
Resources[edit | edit source]
- Cardiovascular Disease. World Confederation for Physical Therapy (2009).
- Cardiovascular Disease. The World Health Organisation [Accessed 18 July 2016]
- The Global Economic Burden of Non-Communicable Diseases. Harvard School of Public Health (2011).
- ACPICR Standards for Physical Activity and Exercise in the Cardiovascular Population (2015)
- Cardiovascular Disease (CVDs) The World Health Organisation (WHO)
- The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation (2017)
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Jan A. Cardiovascular Disease. May 2020. Available from:https://www.ncbi.nlm.nih.gov/books/NBK535419/ (last accessed 4.8.2020)
- ↑ Bloom, D.E., Cafiero, E.T., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L.R., Fathima, S., Feigl, A.B., Gaziano, T., Mowafi, M., Pandya, A., Prettner, K., Rosenberg, L., Seligman, B., Stein, A.Z., & Weinstein, C. (2011). The Global Economic Burden of Noncommunicable Diseases. Geneva: World Economic Forum
- ↑ 3.0 3.1 https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- ↑ 4.0 4.1 https://www.world-heart-federation.org/resources/risk-factors/
- ↑ British Association for Cardiovascular Prevention and Rehabilitation. The BACPR Standards and Core Components for Cardiovascular Disease Prevention and Rehabilitation 2nd Edition. London : British Association for Cardiovascular Prevention and Rehabilitation;2012.
- ↑ Farrell SW, Kampert JB, Kohl HW 3rd, et al. Influences of cardiorespiratory fitness levels and other predictors on cardiovascular disease mortality in men. Med Sci Sports Exer 1998;30:899905.
- ↑ Kavanagh T, Mertens DJ, Hamm LF, et al . Prediction of Long-Term Prognosis in 12169 Men Referred for Cardiac Rehabilitation. Circulation 2002;106:666-671.
- ↑ Dr Marilyn Moffat, President of the WCPT. How physical therapists fight non-communicable disease throughout the lifespan. 2011