Calgary-Cambridge Guide to the Medical Interview - Initiating the Session
Original Editor - Mariam Hashem based on the course by Marissa Fourie
Introduction[edit | edit source]
The importance of communication in obtaining good health outcomes is well-known.[1][2][3] Communication is an essential part of every interaction with a patient.[4] It is also a teachable skill[5] which is incorporated in the training of medical professionals at tertiary institutions worldwide. The teaching of communication skills is often based on models of communication, the products of extensive research, providing frameworks for gaining clinical data, building rapport and deciding on clinical management.[6] Kurtz and Silverman[7] introduced the Calgary-Cambridge Referenced Observation Guides, which they further refined in the early 2000s. These guidelines, which presents the medical interview in five steps, are the result of the collaboration between two very experienced teachers in clinical communication. The guide was originally intended for use in clinical education at tertiary institutes. The model has since been adapted and used in various health disciplines and serves as a blueprint for many educational institutions in the teaching of education to aspirant health care professionals.[8]
Challenges experienced in the learning of communication include the integration of communication skills with other clinical skills, and the effective carry over of theoretically taught communication skills into real-life scenarios. According to Kurtz et al.,[8] these hardships are experienced because students struggle to combine the focus on interview content (i.e. information gained) with the process of communication during the interview (for example, non-verbal behaviour). The Calgary-Cambridge model teaches communication focusing on both interview content and process simultaneously, thereby integrating the traditional clinical method of history taking with effective communication skills. Patient-centred medicine has been incorporated in both content and process [8].
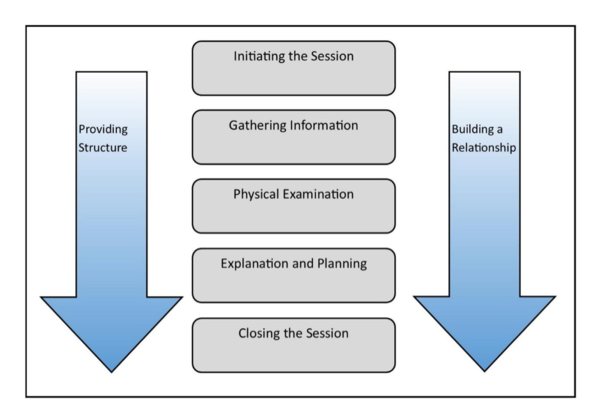
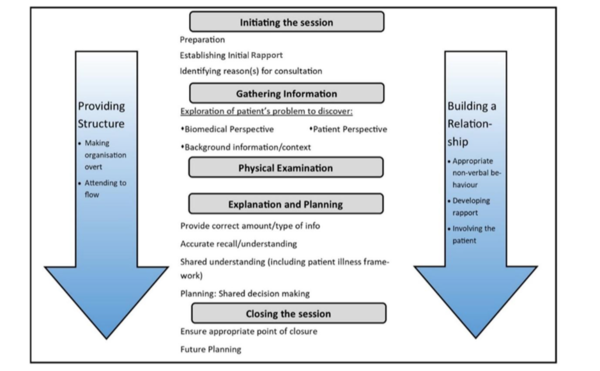
The Calgary-Cambridge model is presented in three diagrams, which aids to enhance communication skills training visually and conceptually. The first diagram (Figure 1) summarises the medical interview as a sequential five-step process: initiation of the session; gathering information; physical examination; explanation and planning; and closing the session.
In the traditional medical assessment, the subjective and objective examinations were considered two different entities. In the Calgary-Cambridge guide, they are integrated, with the inclusion of “physical examination” into the model. Hereby, the interdependence of information gathering from the physical assessment and verbal communication in the natural flow of a true-life medical assessment is illustrated. Provision of structure and relationship building are two steps that continue throughout the entire interview and that develops increasingly as the interview progresses. Figure 2 provides more detail and achievable, evidence-based objectives in each of the steps in the medical interview. The last diagram (Figure 3) shows the interrelationship between content and process, using the example of the gathering of information [8].
The Calgary-Cambridge model provides a practical, integrated method of teaching both the process of communication, as well as the effective gaining of content information.[9] It incorporates the importance of patient-centred medicine including the building of a relationship and shared decision making [10]. The model has been the base of many medical interviews and continues to provide guidance to clinicians in all fields of medicine.
Watch this video if you want to learn more about the Calgary Cambridge Guide to the Medical Interview:
Initiating the session[edit | edit source]
The first physical encounter between patient and clinician sets the scene for the entire medical management to follow. First impressions count – it takes a mere six seconds to accurately identify non-verbal behaviour indicative of personality traits [12] – and once an opinion on a person is formed, it is often difficult to undo[13]. The first few minutes of patient-clinician interaction will determine the extent to which the patient will share information with the clinician[13]. Offering a safe, empathic space from the very first moment of patient encounter will reduce potential anxiety and put patients at ease [14]. The Calgary-Cambridge guide provides three steps for the initiation of the session: Preparing for the encounter, establishing rapport with the patient, and identifying the reason for the consultation. Only once these objectives have been reached, the interview can progress to information gathering[15].
Preparing for the session[edit | edit source]
The pre-consultation period should be used wisely. Always allow for a couple of minutes between patients to end off the earlier consultation, and to get into a neutral mindset before the onset of the following appointment. If there are any loose ends from the earlier appointment that still need attention, make a list thereof and file the relevant documentation in a place where you can attend to it in a designated time at the end of the day (unless in the case of an emergency). Take a moment to identify any stress or negative emotion within yourself, and attempt to deal with it before starting with your next patient. Any distraction of the mind can have a negative effect on your performance and thereby cause clinical errors in the management of your next patient. A good way to “recalibrate” is to have a quick conversation with a colleague, or engaging in some deep breathing exercises or mindfulness prior to a consultation [15][16].
Prepare your working area physically. Pay attention to comfort and neatness, and most importantly, to safety. Remove any potentially hazardous objects (for example, make sure all sharp objects are discarded safely). In the case of a circulating epidemic, ensure that all your working surfaces are thoroughly cleaned. Also pay attention to doorknobs, chairs, taps, pens or any object of potential communal use.
Have the necessary documents at hand, such as evaluation forms, relevant informed consent forms or patient notes. For follow-up or existing patients, page through their notes prior to the consultation to familiarise yourself with their medical history, previous treatments, goals and objectives in current management, or any other relevant information [13][15][16].
Establishing Rapport[edit | edit source]
Rapport is the grasping and appreciation of another person’s intentions, connecting mentally and emotionally [15], and is the most important part of any meaningful relationship [13]. The establishing of rapport starts the moment that two people meet each other. The clinician should introduce him/herself by name, surname and designation, and not expect the patient to know exactly who he/she is. (For example, "Good day Mrs Scott, my name is Marissa Fourie, the physiotherapist who will be looking after you today.") This is especially important in an in-patient setting, where the patient interacts with numerous different health care professionals[17]. Make sure to also know the patient’s name and surname [15] and use the patient’s name often while engaged in communication[17].
An important part of establishing rapport is to convey a message of respect. Body language should not in any way contradict your verbal communication, and your demeanour and behaviour should follow suit. Clinician body positioning should be seated and positioned at patient eye level as this will communicate that you are not rushed, and willing to spend time with the patient, thereby facilitating listening[16][17][18]. Maintain an open body position, leaning somewhat forward and orientating one’s body towards the patient [16]. A balance should be obtained by not positioning yourself too close to the patient, but also not sitting too far either (at the other end of a big desk or table, for example) [15]. The use of other non-verbal cues such as eye contact, applicable gestures/greeting (for example, a handshake) and making the patient comfortable, sends a welcoming and accepting message[13][15].
Clinicians who communicate in a warm, empathic, and reassuring way improve patient satisfaction and adherence. Their patients are reported as more physically functional, more likely to follow medical recommendations, less likely to use pain medication after surgery, less likely to change clinicians and also less likely to sue for malpractice [19].
Identifying the need for the consultation[edit | edit source]
The next step is the verbal initiation of history taking. Many patients find it rather stressful to visit a health care professional due to a number of reasons. These may include feeling physically unwell due to the presenting illness; fear of conveying their message incorrectly, resulting in misdiagnosis; anxiety over a possible bad prognosis or difficult treatment regime; previous negative experience; and discomfort with disclosing personal and sensitive information [20][21]. For this reason, it may be a good idea to first build a conversation on neutral, non-clinical information to put the patient more at ease[22]. Asking a patient about his/her occupation is a convenient conversation starter that will also provide you with some information on the patient’s biopsychosocial and functional status.
Start the clinical questioning with an open-ended general enquiry (“How can I help today?”) rather than a closed-ended request for confirmation (“It looks like you have a sore neck? Let me help you with that!”). The further use of open-ended questions early in the interview is widely recommended [23][15][10][19][24]. Open-ended questions provide a blank canvas for a patient to disclose his/her complaints, rendering them active authorities over their own health information. In contrast, the use of close-ended questions/statements could imply that patients are passive and unable to take responsibility for their own health. Where closed-ended questions lead to yes-no answering, open-ended questions generally yield longer, more comprehensive answers, providing clinicians with more information for the formation of a hypothesis [19]. Also, because open-ended questions provide patients with the opportunity to tell their story in their own words,[19] clinicians can gain better insight into the patient’s perception of his/her issue [22]. Open-ended questions may be followed by closed-end questions only if the clinician needs more clarity on certain details communicated during open-ended questioning. [13] But, take care not to interrupt the patient’s train of thought by asking clarification questions too soon. Many clinicians introduce closed-end questions prematurely in the interview, especially when they are under a time constraint or do not feel that the patient is giving them the information that they need[17][25].
A common pitfall to avoid is to interrupt a patient in the early minutes of the interview. Studies have shown that clinicians typically interrupt patients after only 22 seconds of talking in their initial evaluation; yet, if patients were left to talk uninterruptedly, 80% will be done in less than two minutes, providing the majority of information needed already [25]. Once interrupted, patients tend not to disclose new information, and in this way, a lot of information is not communicated[15]. Therefore, by interrupting to pursue details of symptoms too early on, the clinician may miss an opportunity to discover the full range of patient concerns[23]. Rather encourage the patient to continue talking along relevant lines with the use of facilitation behaviour/statements, which can include cues such as nodding, or saying uh-huh, or phrases such as or tell me more?.
After the patient has completed the initial problem statement, the clinician can provide a brief summary of what is understood. Follow this up with an invitation to disclose anything else that may be problematic (“Is there anything else?”). Patients do not necessarily disclose information chronologically or prioritised according to levels of significance and relevance. Also, patients may elect not to disclose other symptoms they may be experiencing, since they may feel those symptoms are irrelevant to the presenting problem. However, biomedically the different symptoms could well be related and should be investigated.
Conclusion[edit | edit source]
The optimal use of the initial minutes of the clinical interview provides an opportunity to invest in the effectiveness of the entire medical management. This time slot holds the potential to lay the foundation for a trusting, well-functioning patient-clinician relationship and positively influence both patient satisfaction and medical outcomes.
Initiating the Session Case Studies[edit | edit source]
References[edit | edit source]
- ↑ Hiller A, Delany C. Communication in physiotherapy: Challenging established theoretical approaches. Manipulating Practices: A Critical Physiotherapy Reader. 2018:308-33.
- ↑ Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs. 2021 Sep;158.
- ↑ Baniaghil AS, Ghasemi S, Rezaei-Aval M, Behnampour N. Effect of communication skills training using the Calgary-Cambridge Model on interviewing skills among midwifery students: a randomized controlled trial. Iran J Nurs Midwifery Res. 2022 Jan 25;27(1):24-9.
- ↑ Gilligan C, Powell M, Lynagh MC, Ward BM, Lonsdale C, Harvey P, et al. Interventions for improving medical students' interpersonal communication in medical consultations. Cochrane Database Syst Rev. 2021 Feb 8;2(2):CD012418.
- ↑ Douglas AH, Acharya SP, Allery LA. Communication skills learning through role models in Nepal; what are medical students really learning? A qualitative study. BMC Med Educ. 2021 Dec 20;21(1):625.
- ↑ Modi, J.N., Anshu, Chhatwal, J., Gupta, P., Singh, T., Teaching and assessing communication skills in medical undergraduate training. Indian Pediatr. 2016 53, 497–504
- ↑ Kurtz, S.M., Silverman, J.D.. The Calgary-Cambridge Referenced Observation Guides: an aid to defining the curriculum and organizing the teaching in communication training programmes. Med. Educ. 1996 30, 83–89.
- ↑ 8.0 8.1 8.2 8.3 Kurtz, S., Silverman, J., Benson, J., Draper, J. Marrying Content and Process in Clinical Method Teaching: Enhancing the Calgary–Cambridge Guides. Acad. Med. 2003 78, 802–809.
- ↑ Ammentorp J, Bigi S, Silverman J, Sator M, Gillen P, Ryan W, Rosenbaum M, Chiswell M, Doherty E, Martin P. Upscaling communication skills training–lessons learned from international initiatives. Patient Education and Counseling. 2021 Feb 1;104(2):352-9.
- ↑ 10.0 10.1 Main, C.J., Buchbinder, R., Porcheret, M., Foster, N. Addressing patient beliefs and expectations in the consultation. Best Pract. Res. Clin. Rheumatol. 2010 24, 219–225.
- ↑ Dr Alex. Introduction to the Calgary Cambridge Guide to the Medical Interview. Published 1 June 2018. Available from: https://www.youtube.com/watch?v=zjAqbWvnFB0
- ↑ Ambady, N., Rosenthal, R.,Half a minute: Predicting teacher evaluations from thin slices of nonverbal behavior and physical attractiveness. J. Pers. Soc. Psychol. 1993: 64, 431–441.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Bakic-Miric, N., Bakić, N.,Successful doctor-patient communication and rapport building as the key skills of medical practice. Med. Biol. 2008: 15, 74–79.
- ↑ Steiner-Hofbauer, V., Schrank, B., Holzinger, A., 2018. What is a good doctor? Wien. Med. Wochenschr. 168, 398–405.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 15.7 15.8 Kaufman, G.,Patient assessment: effective consultation and history taking. Nurs. Stand. R. Coll. Nurs. G. B. 2008: 1987 23, 50–6, quiz 58, 60.
- ↑ 16.0 16.1 16.2 16.3 Zulman, D.M., Haverfield, M.C., Shaw, J.G., Brown-Johnson, C.G., Schwartz, R., Tierney, A.A., Zionts, D.L., Safaeinili, N., Fischer, M., Israni, S.T., Asch, S.M., Verghese, A.,Practices to Foster Physician Presence and Connection With Patients in the Clinical Encounter. JAMA 2020: 323, 70–81.
- ↑ 17.0 17.1 17.2 17.3 Kuehl, S.P.,Communication Tools for the Modern Doctor Bag. Physician Patient Communication Part 1: Beginning of a medical interview. J. Community Hosp. Intern. Med. Perspect. 2011:1, 8428.
- ↑ Hashim MJ. Patient-centered communication: basic skills. American family physician. 2017 Jan 1;95(1):29-34.
- ↑ 19.0 19.1 19.2 19.3 Robinson, J.D., Heritage, J.,Physicians’ opening questions and patients’ satisfaction. Patient Educ. Couns., EACH Conference 2006: 2004 60, 279–285.
- ↑ Beach, W.A., Easter, D.W., Good, J.S., Pigeron, E.,Disclosing and responding to cancer “fears” during oncology interviews. Soc. Sci. Med. 2005: 60, 893–910.
- ↑ Bensing, J.M., Verheul, W., Dulmen, A.M. van,Patient anxiety in the medical encounter: A study of verbal and nonverbal communication in general practice. Health education. 2008 Aug 29.108(5):373-383
- ↑ 22.0 22.1 Ranjan, P., Kumari, A., Chakrawarty, A.,How can Doctors Improve their Communication Skills? J. Clin. Diagn. Res. JCDR 2015: 9, JE01–JE04.
- ↑ 23.0 23.1 Dugdale, D.C., Epstein, R., Pantilat, S.Z.,Time and the Patient–Physician Relationship. J. Gen. Intern. Med. 1999: 14, S34–S40.
- ↑ Takemura, Y., Sakurai, Y., Yokoya, S., Otaki, J., Matsuoka, T., Ban, N., Hirata, I., Miki, T., Tsuda, T.,Open-Ended Questions: Are They Really Beneficial for Gathering Medical Information from Patients? Tohoku J. Exp. Med. 2005: 206, 151–154.
- ↑ 25.0 25.1 Langewitz, W., Denz, M., Keller, A., Kiss, A., Rütimann, S., Wössmer, B.,Spontaneous talking time at start of consultation in outpatient clinic: cohort study. BMJ 2002: 325, 682–683.
- ↑ University of Nottingham. 2013. Clinical communication skills - verbal communication - version 1 of 2. Available from: https://www.youtube.com/watch?v=Cgut_WRNywo
- ↑ sgulcso. 2008. History Taking (Phase One: Initiating the session). Available from: https://www.youtube.com/watch?v=CrqNa9a9PZY
- ↑ University of Nottingham. 2014. Clinical communication skills - communication using an interpreter. Available from: https://www.youtube.com/watch?v=N8iqH9qwIAQ