Burn Wound Assessment
Top Contributors - Carin Hunter, Stacy Schiurring and Jess Bell
Burn Wound Terminology[edit | edit source]
Eschar: Eschar refers to the nonviable layers of skin or tissue indicating deep partial or full thickness injury. It is black, thick and leathery in appearance. This word is not synonymous with the word "scab".
Scab: Dry, crusty residue accumulated on top of a wound, resulting from coagulation of blood, purulent drainage, serum or a combination of all.
Pseudo-Eschar: A thick gelatinous yellow or tan film that forms with silver sulfadiazine cream combining with wound exudate. It can often be mistaken for eschar, but it can be removed with mechanical debridement.
Petechiae: Pinpoint, round spots that appear on the skin as a result of bleeding. The spots can appear red, brown or purple in colour.
Classification by Depth[edit | edit source]
For an overview on wound healing, and the anatomy and physiology of the skin, please read this article.
| Type | Layers Involved | Signs and Symptoms | Healing Time | Prognosis and Complications |
| Superficial
(formerly first-degree burn) |
Epidermis |
|
Re-epithelialisation takes 2-5 days |
|
| Superficial Partial Thickness
(formerly second-degree burn) |
Epidermis and can extend into the superficial dermis |
|
Re-epithelialisation takes 1-2 weeks |
|
| Deep Partial Thickness
(formerly deep second-degree burn) |
Extends into deep (reticular) dermis
Often causes damage to the hair follicle and glandular tissue |
|
Re-epithelialisation takes 2-5 weeks.
Some require surgical closure |
|
| Full Thickness
(formerly third-degree burn) |
Extends through entire dermis and can often affect the underlying subcutaneous tissue |
|
Prolonged (months) and often requires surgical interventions to ultimately close |
|
| Subcutaneous
(formerly fourth-degree burn) |
Destruction of dermis and hypodermis, and into underlying fat, muscle and bone |
|
Does not heal on its own
Requires surgery and reconstruction |
|
Circumferential burn injury special considerations[edit | edit source]
A circumferential burn wound is typically found around an extremity or the torso and puts the patient at a significant risk for compartment syndrome. This pattern of burn injury involves Deep Partial Thickness, Full Thickness, and or Subcutaneous burns.
Circumferential burn injury signs and symptoms for potential compartment syndrome:
- Out of proportion pain with any movement distal to the circumferential injury.
- Diminished or lack of a pulse distal to the area of circumferential injury.
- Diminished or lack of capillary refill in the fingers and the toes. However, assessment for compartment syndrome can be limited if the injury prevents assessment of capillary refill due to extremity damage or amputation.
- A red flag sign of developing compartment syndrome is a decrease in temperature of the tissue distal to the area of circumferential injury, especially on an extremity.
- For patients with circumferential burn injuries around the torso: high concern for development of compartment syndrome if they experience difficulty breathing or an increase in difficulty breathing.
If a patient is experiencing the signs and symptoms of compartment syndrome, the medical team should be immediately alerted for further assessment and intervention.
Blanch Test[edit | edit source]
The blanch test is similar to the capillary refill test. It is a bedside exam to assess blood flow to the capillaries of the skin. This can be performed over intact skin or in a wound bed itself.
To perform the test:
- Gently but firmly compresses the tissue to be tested until it turns white
- Record the time taken for the area to return to the previous color
- Refill time should take 3 seconds or less. If the refill time is longer suspect capillary damage, if there is no change in color with applied pressure, suspect capillary destruction.
Please short the following short optional video for a demonstration of the blanch test.
Jacksons’ Burn Wound Model[edit | edit source]
Jacksons’ Burn Wound Model[1] is a model used to understand the pathophysiology of a burn would. This model divides the wound into three zones.
- Zone of Coagulation: This is the area central to the injury and is the area that experiences the greatest tissue damage. Often characterised by complete destruction of the capillaries leading to complete cell death. This is irreversible as there is no capillary refill.
- Zone of Stasis or Zone of Ischaemia: This area is adjacent to the zone of coagulation and as the name suggests, it is a zone in which the there is slowing of circulating blood due to the damage. These are areas of deep partial thickness burns, or burns of indeterminate depth. This zone can usually be saved with the correct wound care. Capillaries are often compromised by oedema due to hypovolemia vasoconstrictive mediators responding to injury. It is reversible if capillary flow can be restored.
- Zone of Hyperaemia: This zone is located around the edge of the previous zone and is characterised by the eased blood supply and inflammatory vasodilation. This tissue has a good recovery rate, as long as there are no complications, such as severe sepsis or prolonged hypo-perfusion. increased blood flow due to release of histamine. This area will recover completely without intervention unless complications occur, characterised by superficial and superficial partial thickness burns and has a robust capillary refill.
Burn Wound Conversion[edit | edit source]
Burn Wound Conversion: [2] This refers to the worsening of tissue damage in a superficial burn which previously was expected to spontaneously heal, but it increases in tissue depth into a deeper wound which requires excision.
Potential Causes:
- Dessication
- Infection
- Oedema
Total Body Surface Area[edit | edit source]
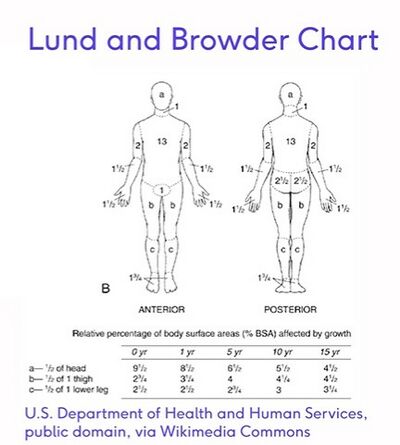
The main reason the total body surface area is needed is that it is an important figure when applying the Parkland Burn Formula. This formula is the most widely used formula to estimate the fluid resuscitation required by a burns patient on hospital admission, usually within the first 24 hours. When applying this formula, the first step is to calculate the percentage of body surface area (BSA) damaged, which is most commonly done by the "Wallace Rule of Nines".[3] When conducting a paediatric assessment, the Lund-Browder Method is commonly used, as children have a greater percentage surface area of their head and neck compared to an adult. The formula recommends 4 millilitres per kilogram of body weight in adults (3 millilitres per kilogram in children) per percentage burn of total body surface area (%TBSA) of crystalloid solution over the first 24 hours of care.[4]
4 mL/kg/%TBSA (3 mL/kg/%TBSA in children) = total amount of crystalloid fluid during first 24 hours
The latest research has indicated that while this method is still in use, the fluid levels should be constantly monitored, while assessing the urine output,[5] to prevent over-resuscitation or under-resuscitation.[6]
Calculation of Percentage Burn of Total Body Surface Area[edit | edit source]
- The Rule of Nine
- Lund-Browder Method
- Palmer Method
1. The Rule of Nine[edit | edit source]
| Body Part | Percentage for Rule of Nine |
| Head and Neck | 9% |
| Entire chest | 9% |
| Entire abdomen | 9% |
| Entire back | 18% |
| Lower Extremity | 18% each |
| Upper Extremity | 9% each |
| Groin | 1% |
2. Lund-Browder Method[edit | edit source]
3. Palmar Surface Method[edit | edit source]
The "Rule of Palm" or Palmar Surface Method can be used to estimate body surface area of a burn. This rule indicates that the palm of the patient, with the exclusion of the fingers and wrist, is approximately 1% of the patients body surface area. When a quick estimate is required, the percentage body surface area will be the number of the patient's own palm it would take to cover their injury. It is important to use the patient's palm and not the provider's palm.
References[edit | edit source]
- ↑ Harish V, Li Z, Maitz PK. First aid is associated with improved outcomes in large body surface area burns. Burns. 2019 Dec 1;45(8):1743-8.
- ↑ Palackic A, Jay JW, Duggan RP, Branski LK, Wolf SE, Ansari N, El Ayadi A. Therapeutic Strategies to Reduce Burn Wound Conversion. Medicina. 2022 Jul;58(7):922.
- ↑ Bereda G. Burn Classifications with Its Treatment and Parkland Formula Fluid Resuscitation for Burn Management: Perspectives. Clinical Medicine And Health Research Journal. 2022 May 12;2(3):136-41.
- ↑ Mehta M, Tudor GJ. Parkland formula. 2019
- ↑ Ahmed FE, Sayed AG, Gad AM, Saleh DM, Elbadawy AM. A Model for Validation of Parkland Formula for Resuscitation of Major Burn in Pediatrics. The Egyptian Journal of Plastic and Reconstructive Surgery. 2022 Apr 1;46(2):155-8.
- ↑ Ete G, Chaturvedi G, Barreto E, Paul M K. Effectiveness of Parkland formula in the estimation of resuscitation fluid volume in adult thermal burns. Chinese Journal of Traumatology. 2019 Apr 1;22(02):113-6.