Bronchiolitis
Original Editor - Jerome Ng
Top Contributors - Jerome Ng, Kim Jackson, Donald John Auson, Wendy Snyders, Naomi O'Reilly, WikiSysop, Adam Vallely Farrell, Vidya Acharya and Candace Goh
Clinically Relevant Anatomy[edit | edit source]
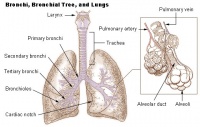
Bronchiolitis is inflammation of the bronchioles, the smallest air passages of the lungs, in which air passes through the nose or mouth to the alveoli of the lungs where gas exchange takes place.
Epidemiology[edit | edit source]
Bronchiolitis typically affects infants and children under 2 years old[1] but it can also affect people of any age. It also has a seasonal predilection, with more infections during the winter.[1]
Etiology[edit | edit source]
Bronchiolitis is usually caused by the Respiratory Syncytial Virus (RSV). Other pathogens can also cause bronchiolitis such as human rhinovirus, influenza virus, coronavirus, human metapneumovirus (hMPV) and parainfluenza virus.[2]
Mechanism of Injury / Pathological Process[edit | edit source]
Bronchiolitis typically occurs with primary infection or reinfection with a viral pathogen, but occasionally is caused by bacteria (eg, Mycoplasma pneumoniae). In young children, the clinical syndrome of bronchiolitis may overlap with recurrent virus-induced wheezing and acute viral-triggered asthma.
Clinical Presentation[edit | edit source]
Bronchiolitis is a major cause of illness and hospitalization in infants and children younger than two years. Symptoms include:
- Fever
- Dry cough
- Persistently increased respiratory effort (tachypnea, nasal flaring, intercostal or suprasternal retractions, accessory muscle use, grunting)
- Hypoxemia
- Apnea
- Acute respiratory failure
Diagnosis[edit | edit source]
Diagnosis can be made through physical examination and history taking. Confirmatory laboratory studies can also be done to identify the causative agent as well as to rule out other pathologies.
Laboratory studies can include:
- Analaysis of specimen via:
- Indirect immunofluorescent-antibody assay (IFA)
- Polymerase chain reaction (PCR)
- Reverse transcription-PCR
- Arterial blood gas analysis
- Blood culture
- Pulse oximetry
Differential Diagnosis[edit | edit source]
Other pathologies that can present with symptoms similar from bronchiolitis include:
- Asthma
- Pneumonia
- COPD
- Croup
- Cystic Fibrosis
Management / Interventions[edit | edit source]
- Hydration
- Respiratory support
- Nasal suctioning
- Supplemental oxygen
The following are interventions that may be used, but not as a routine intervention:
- Trial of inhaled bronchodilator
- Nebulized hypertonic saline
- Glucocorticoids
- Chest physiotherapy
Key Evidence[edit | edit source]
In the Cochrane review titled "Chest physiotherapy for acute bronchiolitis in children younger than two years of age", it was concluded that none of the chest physiotheray techniques (vibrations, percussions, slow passive expiratory techniques or forced expiratory techniques) have demonstrated a reduction in the severity of disease. Hence, these tecniques cannot be used as standard clinical practice for hospitalised patients with severe bronchiolitis.[3]
A state-of-art review suggests avoiding repeated airway clearance in infants and children with acute pulmonary disease.[4]
References[edit | edit source]
- ↑ 1.0 1.1 Bronchiolitis. nhs.uk. [cited 13 April 2020]. Available from: https://www.nhs.uk/conditions/bronchiolitis/
- ↑ Miller EK, Gebretsadik T, Carroll KN, et al. Viral etiologies of infant bronchiolitis, croup and upper respiratory illness during 4 consecutive years. Pediatr Infect Dis J. 2013;32(9):950–955. doi:10.1097/INF.0b013e31829b7e43 Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880140/
- ↑ Roqué i Figuls M, Giné-Garriga M, Granados Rugeles C, Perrotta C, Vilaró J. Chest physiotherapy for acute bronchiolitis in paediatric patients between 0 and 24 months old. Cochrane Database of Systematic Reviews 2016, Issue 2. Art. No.: CD004873. DOI: 10.1002/14651858.CD004873.pub5.
- ↑ Morrow BM. Airway clearance therapy in acute paediatric respiratory illness: A state-of-the-art review. South African Journal of Physiotherapy. 2019 Jun 25;75(1):12.