Borderline Personality Disorder
Introduction[edit | edit source]
Borderline personality disorder is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) as “a pervasive pattern of instability in interpersonal relationships, self-image, and affects, as well as marked impulsivity beginning by early adulthood and present in a variety of contexts.”[1]
The DSM categorizes borderline personality disorder as one of 10 personality disorders, which are separate mental illnesses that all cause difficulty with the patients ability to relate to others in healthy ways, resulting in distress or impact on functioning.[2] To note, the 2019 revision of the International Classification of Diseases (ICD-11) does not recognize borderline personality disorder as a separate condition, instead classing all personality disorders as one condition classified by severity.[3] However, at present borderline personality disorder is still treated as a recognized specific condition both in practice and in research. [4]
Etiology[edit | edit source]
It is believed borderline personality disorder is caused by the combination of genetic predisposition, neurobiological dysfunction and environmental factors. [5]
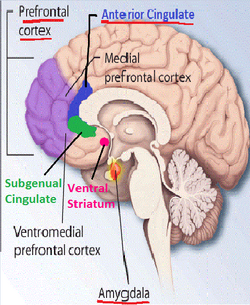
There is a higher risk if it runs in your immediate family, with one study finding a 46% heritability.[6] So far, research has identified two genes DPYD and PKP4 linked with increasing the risk of developing BPD, but it is worth noting these are also linked with the risk of developing schizophrenia and bipolar disorder.[7] The amygdala, hippocampus and orbitofrontal cortex have been identified as either being smaller or having unusual levels of activity in many patients with borderline personality disorder.[8] Impaired serotonin function has also been found in this patient group.[5]The environmental risk factors are predominantly from childhood, including physical or sexual assault, neglect, parental mental illness or substance abuse, poor maternal attachment or separation and inappropriate family boundaries. [5]
Epidemiology[edit | edit source]
The prevalence of borderline personality disorder is estimated to be 1.6% in the general population and around 20% in the inpatient psychiatric population.[5]
Characteristics/Clinical Presentation[edit | edit source]
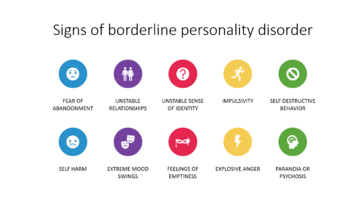
According to the National Institute of Mental Health, patients with borderline personality disorder may present with:[9]
- A long term pattern of intense and unstable relationships with family, friends, and loved ones.
- Short term episodes of variable and extreme moods.
- Trying to avoid real or perceived abandonment, including starting and ending relationships very quickly and without warning.
- Impaired sense of self.
- Anger management issues.
- Feelings of dissociation from oneself.
- Feelings of emptiness.
- Impulsive / dangerous behaviors, including with finances, binge eating, unsafe sexual practices and substance abuse.
Associated Co-morbidities[edit | edit source]
- Bipolar disorder.[10]
- Suicidal behaviors and self-harm.[11][12]
- Other personality disorders, mood disorders/depression, anxiety, substance-related disorders, somatic symptom disorders, and eating disorders. [2][13]
- Physical co-morbidities significantly associated are arteriosclerosis, hypertension, hepatic disease, cardiovascular disease, gastrointestinal disease and arthritis. [14]
Management / Interventions
[edit | edit source]
Due to the long term, complex and variable nature of borderline personality disorder, there should be a care pathway developed with an agreed set of outcome measures.[15]A survey found patients benefited from learning about the disorder, building trust with clinical staff, and when validated felt empowered.[16] Psychotherapy is the main treatment for borderline personality disorder. Specific types of psychotherapy include dialectical behavior therapy (DBT), schema-focused therapy, mentalization based therapy (MBT), systems training for emotional predictability and problem-solving (STEPPS), transference-focused psychotherapy (TFP).[17] There are no specific medications for the overall treatment of borderline personality disorder, but antidepressants, anti-psychotics and other mood-stabilizing drugs can help with symptoms including depression, anger, anxiety, impulsiveness and improve global functioning.[17][18]
Physiotherapy Management[edit | edit source]
Physiotherapy can provide health promotion, injury prevention, and rehabilitation. [19] Exercise and other healthy lifestyle habits, including diet and sleep patterns, which physiotherapists can support with, can help to supplement medical and psychological management of borderline personality disorder.[20]These interventions are also cost effective. [21]
Differential Diagnosis
[edit | edit source]
- Bipolar disorder
- Depression
- Schizophrenia
- Attention-deficit disorder
- Post-traumatic stress disorder[22]
Resources
[edit | edit source]
References[edit | edit source]
- ↑ American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-IV-TR. New York: APA, 2000.
- ↑ 2.0 2.1 Salters-Pedneault, K. What are Personality Disorders in the DSM-5? [Internet] 2022. (Accessed 07/05/2022) Available from: https://www.verywellmind.com/personality-disorders-a2-425427
- ↑ World Health Organisation, International Statistical Classification of Diseases and Related Health Problems, 11th ed, 2019.
- ↑ Mind. Types of Personality Disorder [Internet] 2020 (Accessed 07/05/2022) Available from: https://www.mind.org.uk/information-support/types-of-mental-health-problems/personality-disorders/types-of-personality-disorder/
- ↑ 5.0 5.1 5.2 5.3 Chapman J, Jamil RT, Fleisher C. Borderline Personality Disorder. Florida: StatPearls Publishing, 2022
- ↑ Skoglund C., Tiger A., Rück C., Petrovic P., Asheron P., Hellner C. et al. Familial risk and heritability of diagnosed borderline personality disorder: a register study of the Swedish population. Mol Psychiatry. 2021: [[1]]
- ↑ Witt SH, Streit F, Jungkunz M, Frank J, Awasthi S, Reinbold CS, et al. Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl Psychiatry. 2017; 7.
- ↑ NHS. Borderline Personality Disorder. 2019. (Accessed 07/05/2022) Available from: https://www.nhs.uk/mental-health/conditions/borderline-personality-disorder/causes/#:~:text=Environmental%20factors&text=being%20a%20victim%20of%20emotional,drink%20or%20drug%20misuse%20problem
- ↑ National Institute of Mental Health. Borderline Personality Disorder. 2022. (Accessed 07/05/2022) Available from: https://www.nimh.nih.gov/health/topics/borderline-personality-disorder
- ↑ Fornaro M, Orsolini L, Marini S, De Berardis D, Perna G, Valchera A, et al. The prevalence and predictors of bipolar and borderline personality disorders comorbidity: Systematic review and meta-analysis. J Affect Disord. 2016; 195: 105-118
- ↑ Paris J. Suicidality in Borderline Personality Disorder. Medicina (Kaunas). 2019; 55: 6
- ↑ Oumaya M, Friedman S, Pham A, Abou Abdallah T, Guelfi JD, Rouillon F. Personnalité borderline, automutilations et suicide : revue de la littérature [Borderline personality disorder, self-mutilation and suicide: literature review]. L’Encephale. 2008; 34: 452-458
- ↑ Mark Zimmerman. Overview of Personality Disorders. MSD Manual Professional Version. [Internet] 2021. (Accessed 07/05/2022) Available from: https://www.msdmanuals.com/professional/psychiatric-disorders/personality-disorders/overview-of-personality-disorders
- ↑ El-Gabalawy R, Katz LY, Sareen J. Comorbidity and associated severity of borderline personality disorder and physical health conditions in a nationally representative sample. Psychosom Med. 2010; 72: 641-647
- ↑ National Institute of Health and Care Excellence. Borderline personality disorder: recognition and management. Clinical guideline [CG78] 2009. (Accessed 07/05/2022). Available from: https://www.nice.org.uk/guidance/cg78
- ↑ Romeu-Labayen M, Rigol Cuadra MA, Galbany-Estragués P, Blanco Corbal S, Giralt Palou RM, Tort-Nasarre G. Borderline personality disorder in a community setting: service users' experiences of the therapeutic relationship with mental health nurses. Int J Ment Health Nurs. 2020; 29: 868-877
- ↑ 17.0 17.1 Mayo Clinic. Borderline Personality Disorder. 2019. (Accessed 07/05/2022). Available from: https://www.mayoclinic.org/diseases-conditions/borderline-personality-disorder/diagnosis-treatment/drc-20370242
- ↑ Parker JD, Naeem A. Pharmacologic Treatment of Borderline Personality Disorder. Am Fam Physician. 2019; 99
- ↑ Probst, M. . Physiotherapy and Mental Health. In: Suzuki, T. , editor. Clinical Physical Therapy . London: IntechOpen, 2017
- ↑ Choi-Kain L., Finch E., Masland S., Jenkins J., Unruh B. “What Works in the Treatment of Borderline Personality Disorder.” Current Behavioural Neuroscience Reports 2017; 4: 21-30
- ↑ Van Asselt A., Dirksen C., Arntz A., Giesen-Bloo J., Van Dyck R., Spinhoven P., et al Out-patient psychotherapy for borderline personality disorder: Cost-effectiveness of schema-focused therapy v. transference-focused psychotherapy. British Journal of Psychiatry. 2008; 192: 450-457
- ↑ Paris J. Differential Diagnosis of Borderline Personality Disorder. Psychiatr Clin North Am. 2018; 41: 575-582
- ↑ About Medicine. What is Borderline Personality Disorder? Available from: https://www.youtube.com/watch?v=KSPhc2NJA2Q