Body Awareness in Survivors of Trauma
Original Editor - Naomi O'Reilly
Top Contributors - Naomi O'Reilly, Jess Bell and Nupur Smit Shah
Body Awareness[edit | edit source]
Body awareness is an approach often used within rehabilitation for individuals with persistent / complex pain[1][2] and / or psychosomatic / psychiatric conditions.[3][4][5][6] It explores and uses the mind-body-(spirit) connection to develop a more positive experience of the body and self through reflection of our bodily experiences.[7][8]
Body awareness has been defined as a treatment directed towards "an awareness of how the body is used in terms of body function, behaviour, and interaction with self and others."[9] It can be influenced by our emotional regulation (i.e. our ability to exert control over our emotional state) and interoception (i.e. our perception of sensations from inside the body, including the perception of physical sensations related to internal organ function such as heartbeat, respiration, satiety, and autonomic nervous system activity related to our emotions).[10]
Use of body awareness strategies and therapies aim to normalise and help restore breathing, posture, balance, and muscular tension, which are commonly experienced and visible in the movement behaviour of individuals who have experienced trauma or displacement.[9][11]
It is, however, important to note that the use of techniques such as body awareness and mindfulness require significant care. They can open up emotional wounds that need more than mindful awareness for healing.[12] Treleaven and Britton state that: "When we ask someone with trauma to pay close, sustained attention to their internal experience, we invite them into contact with traumatic stimuli - thoughts, images, memories, and physical sensations that may be related to a traumatic experience….this can aggravate and intensify symptoms of traumatic stress, in some cases even lead to retraumatization - a relapse into an intensely traumatized state."[13]
To find out more about the use of mindfulness, please see: Mindfulness for our Patients.
Barriers to Care[edit | edit source]
Access to healthcare is a complex concept. If services are available and there is an adequate supply of services, then the opportunity to obtain healthcare exists, and a population may 'have access' to services. However, the services available must be relevant and effective if the population is to 'gain access to satisfactory health outcomes'. There are many factors that can influence a person's ability to receive care. Commonly reported barriers to health include:
- logistical factors (distance to service, lack or cost of transport)
- affordability (of services, treatment, lack of insurance)
- knowledge, attitudinal and cultural factors (including perceived need, fear, and lack of awareness about the service)
The following barriers are just some examples of factors that can significantly impact healthcare access in the context of trauma.
Language Barriers[edit | edit source]
Research suggests that communication difficulties act as a critical barrier for displaced persons seeking health and social services.[14] The majority of displaced persons may not speak the language of the host country and have fear of and difficulty in expressing their medical symptoms in a second language.[15] Therefore, people with a language barrier are often unable to seek adequate medical attention without interpreters or translators, and these services may not be widely available depending on the language of the person.[16] Even when an interpreter is available, miscommunication can occur between individuals and rehabilitation professionals due to the lack of proficient medical interpreters, potentially resulting in inappropriate and inadequate care.[14] Confusion might arise during medical and rehabilitation consultations, which can lead to feelings of alienation and mistrust, and may prevent the individual from seeking out future medical care.[17]
For more information, please see: Working With Interpreters.
Cultural Barriers[edit | edit source]
"Cultural competence is a set of congruent behaviors, attitudes and policies that come together in a group of people to work effectively in cross-cultural situations such as an evaluation of programs and services provided to immigrants and refugees. The word 'culture' is the integrated pattern of learned human behavior that includes thoughts, communications, actions, customs, beliefs, values and institutions of a social group. The word 'competence' implies having the capacity to function effectively."[18]
Unfortunately, there is evidence to suggest that race and ethnicity can affect the way that individuals report pain and also the way in which rehabilitation professionals interpret an individual's pain. Research suggests that physicians are twice as likely to underestimate a patient with black ethnicity’s pain in comparison to patients of white ethnicity.[19] Rehabilitation professionals need to be aware of their own cultural identity, develop an understanding of cultural knowledge of common health beliefs and behaviours and ensure they display culturally-sensitive behaviours (e.g., empathy, trust, acceptance, respect) to improve therapeutic alliance and clinical outcomes.[20]
To gain more insight into implicit bias and its impact on healthcare, please see: Implicit Bias in Healthcare.
Understanding of the Healthcare System[edit | edit source]
Lack of knowledge about how to navigate complex healthcare systems can result in poor access to healthcare services. The limited information on accessing primary healthcare services and not knowing who to ask or where to go for healthcare can result in frustration. It can also prompt individuals to seek help from inappropriate sources.
Impacts of Trauma[edit | edit source]
Trauma "results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that has lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being".[21] It can also include second-hand experiences (e.g. an individual might not have experienced the trauma directly, but they were indirectly affected by it).[21]
For some people, reactions to traumatic events are temporary, with immediate psychological and / or physical effects. For others, trauma can have lasting effects on a person’s life and well-being. Some people have a more sustained reaction to trauma. This reaction can become chronic or persistent, resulting in more severe, prolonged, or enduring mental health consequences (e.g., post-traumatic stress and other anxiety disorders, substance use and mood disorders) and physical impairments (e.g., arthritis, headaches, chronic pain). These ongoing symptoms can lead to a lack of trust or confidence in their body. It can also alter individual biology and behaviour over the life course, which can impact interpersonal and intergenerational relationships, often resulting in a sense of a loss of voice and powerlessness, and difficulty expressing thoughts and feelings.[22]
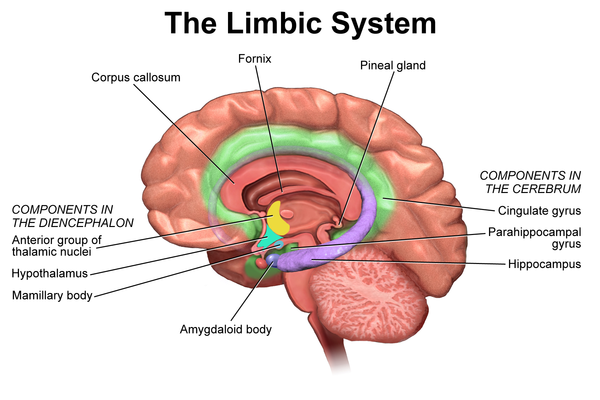
Role of the Limbic System[edit | edit source]
The limbic system is a collection of structures, including the cerebrum, diencephalon and midbrain. It supports a range of functions, such as emotion, behaviour, motivation, long-term memory and olfaction.[23] Subparts of the limbic system ultimately regulate important aspects of our conscious and unconscious patterns (including our emotions, perceptions, relationships, behaviours and motor control). It is the part of the brain that is involved in behaviours we need for survival: feeding, reproduction and caring for our young, and fight-or-flight responses.
The limbic system helps us process emotions such as fear, pleasure, and anger, and helps control our drives (e.g. hunger drive, sexual drive, sleep drive).[24] It also combines higher mental functions and primitive emotion into a single system known as the emotional nervous system. It is responsible for our emotions and higher mental functions, like learning and forming memories.[25]
The limbic system is dynamic and can change in response to input from a person’s environment. Experience also changes this region of the brain. For example, stress has been found to alter plasticity in the nervous system, including in the limbic system.[26] This may help to explain why an individual's psychological and physiological experiences change over time.
Both the limbic system and the cerebral cortex influence autonomic nervous system activities "associated with emotional responses by way of hypothalamic-brainstem pathways."[27] The autonomic nervous system has two divisions:
- Sympathetic nervous system: predominant during emergency “fight-or-flight” responses and exercise
- Parasympathetic nervous system: predominant during quiet activities (i.e. "rest and digest")[27]
The prefrontal cortex is the more of the conscious part of our brain, and it helps us to process information. It is important to note that when we are in a fight or flight response, we can't "rewire" that part of our through our prefrontal cortex. However, body awareness can play a role in changing the limbic system by training the brain to process information differently, assigning new emotions to old memories or supporting an individual to manage chronic stress, pain and trauma.[24]
Resources[edit | edit source]
References[edit | edit source]
- ↑ Gard G. Body awareness therapy for patients with fibromyalgia and chronic pain. Disability and rehabilitation. 2005 Jun 17;27(12):725-8.
- ↑ Ferro Moura Franco K, Lenoir D, dos Santos Franco YR, Jandre Reis FJ, Nunes Cabral CM, Meeus M. Prescription of exercises for the treatment of chronic pain along the continuum of nociplastic pain: A systematic review with meta‐analysis. European Journal of Pain. 2021 Jan;25(1):51-70.
- ↑ Gyllensten AL, Ekdahl C, Hansson L. Long-term effectiveness of basic body awareness therapy in psychiatric out-patient care. A randomised controlled study. Adv Physiother. 2009;11:2–12.
- ↑ Gyllensten AL, Ekdahl C, Hansson L 2009 Long-term effectiveness of Basic Body Awareness Therapy in psychiatric outpatient care. A randomized controlled study. Advances in Physiotherapy 11: 2–12
- ↑ Gyllensten AL, Jacobsen LN, Gard G. Clinician perspectives of Basic Body Awareness Therapy (BBAT) in mental health physical therapy: An international qualitative study. Journal of Bodywork and movement therapies. 2019 Oct 1;23(4):746-51.
- ↑ Solano Lopez AL, Moore S. Dimensions of body-awareness and depressed mood and anxiety. Western journal of nursing research. 2019 Jun;41(6):834-53.
- ↑ Mehling W, Wrubel J, Daubenmier J. Body awareness: a phenomenological inquiry into the common ground of mind-body therapies. Philos Ethics Humanit Med. 2011;6:6.
- ↑ Gyllensten AL, Hansson L, Ekdahl C 2003a Patient experiences of basic body awareness therapy and the relationship with the physiotherapist. Journal of Bodywork and Movement Therapies 7: 173–183
- ↑ 9.0 9.1 Gard G, Nyboe L, Gyllensten AL. Clinical reasoning and clinical use of basic body awareness therapy in physiotherapy–a qualitative study?. European Journal of Physiotherapy. 2020 Jan 2;22(1):29-35.
- ↑ Barrett L. F., Quigley K., Bliss-Moreau E., Aronson K. (2004). Interoceptive sensitivity and self-reports of emotional experience. J. Pers. Soc. Psychol. 87 684–697.
- ↑ Solano Lopez AL, Moore S. Dimensions of body-awareness and depressed mood and anxiety. Western journal of nursing research. 2019 Jun;41(6):834-53.
- ↑ Physiopedia. Mindfulness for our Patients.
- ↑ Treleaven D.A., Britton W. Trauma-sensitive mindfulness: Practices for safe and transformative healing. New York: WW Norton & Company; 2018 Feb 13.
- ↑ 14.0 14.1 Fang ML, Sixsmith J, Lawthom R, Mountian I, Shahrin A. Experiencing ‘pathologized presence and normalized absence’; understanding health related experiences and access to health care among Iraqi and Somali asylum seekers, refugees and persons without legal status. BMC public health. 2015 Dec;15(1):923.
- ↑ Carta MG, Bernal M, Hardoy MC, Haro-Abad JM. Migration and mental health in Europe (the state of the mental health in Europe working group: appendix 1). Clinical practice and epidemiology in mental health. 2005 Dec 1;1(1):13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1236945/
- ↑ Quickfall J. Cross-cultural promotion of health: a partnership process? Principles and factors involved in the culturally competent community based nursing care of asylum applicants in Scotland.https://era.ed.ac.uk/handle/1842/4466
- ↑ Health Challenges for Refugees and Immigrants by Ariel Burgess, VOLUME 25, NUMBER 2 https://reliefweb.int/sites/reliefweb.int/files/resources/ACB7A9B4B95ED39A8525723D006D6047-irsa-refugee-health-apr04.pdf
- ↑ The Colorado Trust. Keys to Cultural Competency: A Literature Review for Evaluators of Recent Immigrant and Refugee Service Programs in Colorado, REFT Institute, Inc. March 2002.
- ↑ Staton LJ, Panda M, Chen I, Genao I, Kurz J, Pasanen M, et al. When race matters: disagreement in pain perception between patients and their physicians in primary care. J Natl Med Assoc. 2007 May;99(5):532-8.
- ↑ Bialocerkowski A, Wells C, Grimmer-Somers K. Teaching physiotherapy skills in culturally-diverse classes. BMC medical education. 2011 Dec;11(1):34. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3146421/
- ↑ 21.0 21.1 Substance Abuse and Mental Health Service Administration. SAMHSA's Concept of Trauma and Guidance for a Trauma-Informed Approach. HHS Publication No.(SMA) 14-4884. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014. Available from:https://ncsacw.acf.hhs.gov/userfiles/files/SAMHSA_Trauma.pdf (last accessed 27 March 2022).
- ↑ Gentsch A, Kuehn E. Clinical manifestations of body memories: The impact of past bodily experiences on mental health. Brain Sciences. 2022 May 3;12(5):594.
- ↑ Kiddle Limbic system facts for kids Available from: https://kids.kiddle.co/Limbic_system (accessed 28.12.2020)
- ↑ 24.0 24.1 Blaney D. Body Awareness in Trauma Survivors Course. Plus, 2023.
- ↑ Boundless. The Limbic System. Available from: https://bluebox.creighton.edu/demo/modules/en-boundless-old/www.boundless.com/psychology/textbooks/boundless-psychology-textbook/biological-foundations-of-psychology-3/structure-and-function-of-the-brain-35/the-limbic-system-154-12689/index.html (last accessed 26 March 2023).
- ↑ Sapolsky RM. Stress and plasticity in the limbic system. Neurochem Res. 2003 Nov;28(11):1735-42.
- ↑ 27.0 27.1 McCorry LK. Physiology of the autonomic nervous system. Am J Pharm Educ. 2007 Aug 15;71(4):78.
- ↑ Abby Vanmunijen. Emotions Wheel. Available from: https://www.avanmuijen.com/watercolor-emotion-wheel (accessed 2 March 2023).
- ↑ Body Needs Mapping Worksheet. Available from: https://www.avanmuijen.com/watercolor-emotion-wheel (accessed 2 March 2023).